Exam Code: HAAD-RN
Exam Name: HAAD Licensure Examination for Registered Nurses
Certification Provider: HAAD
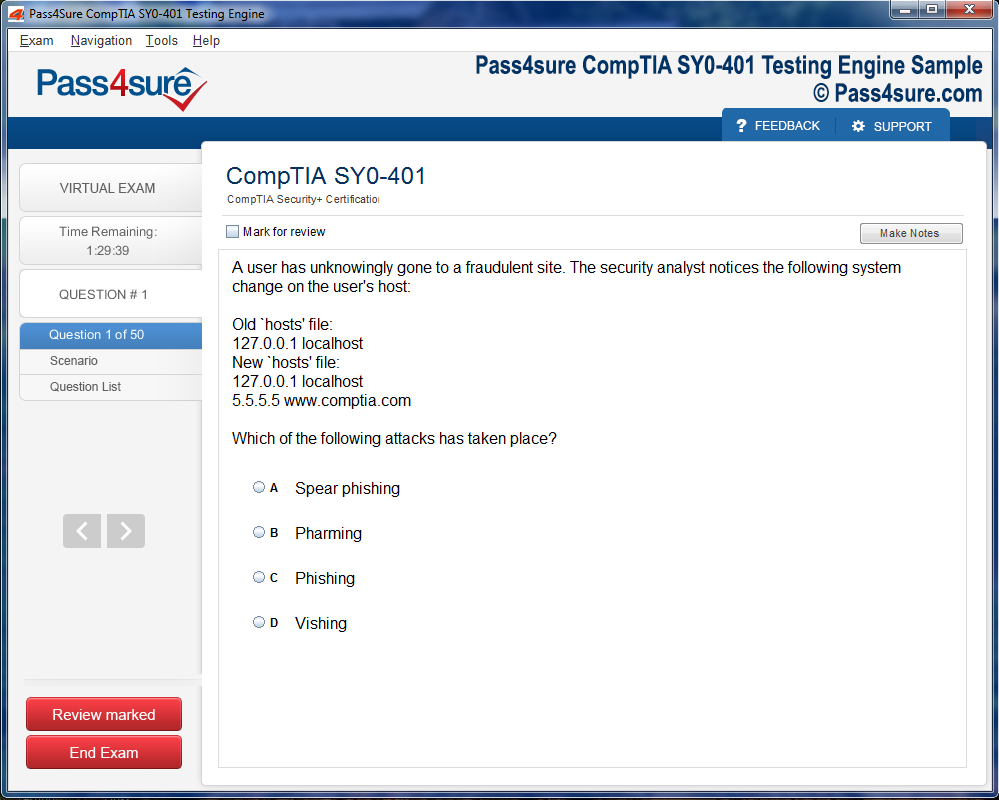
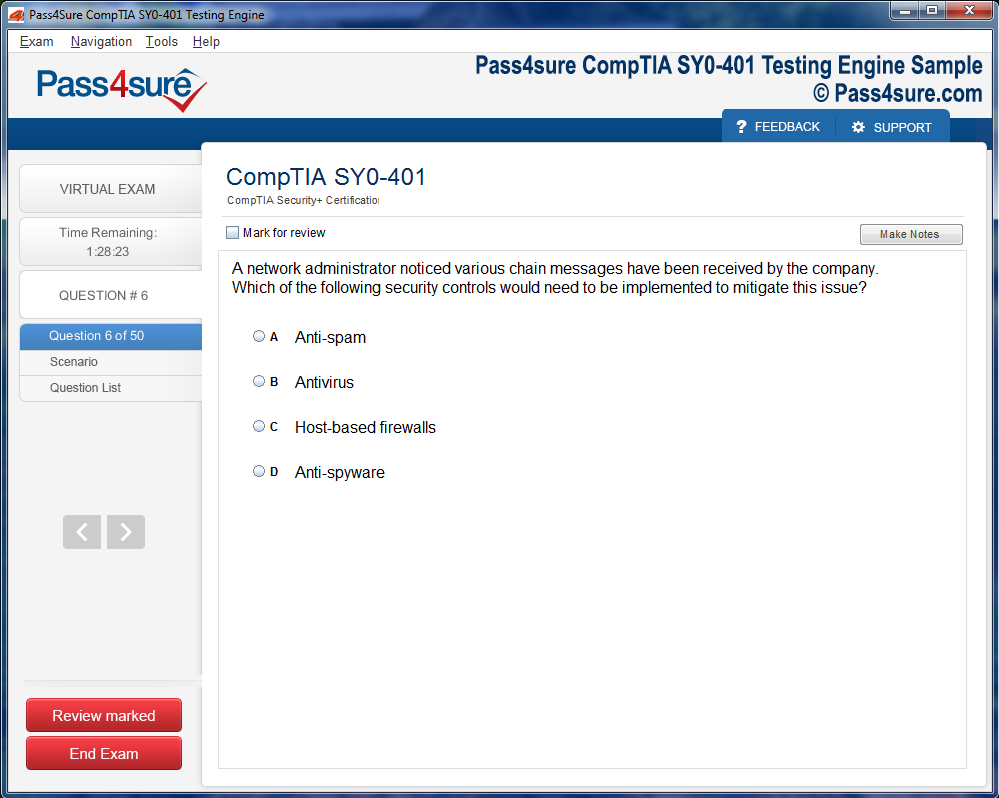
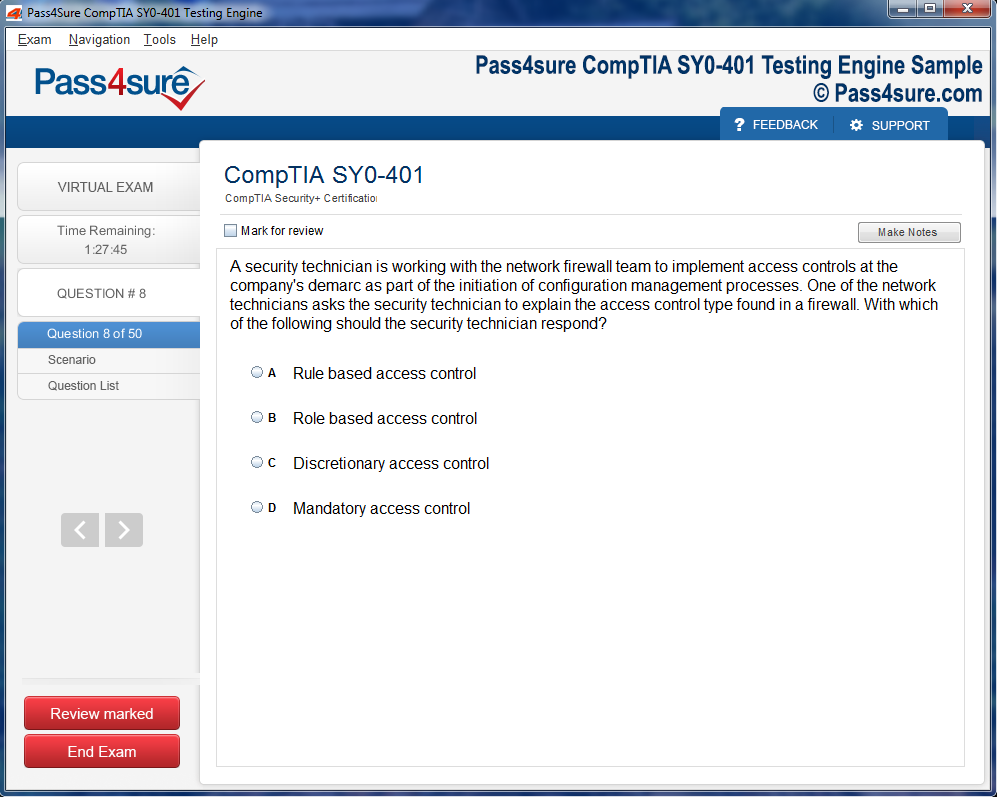
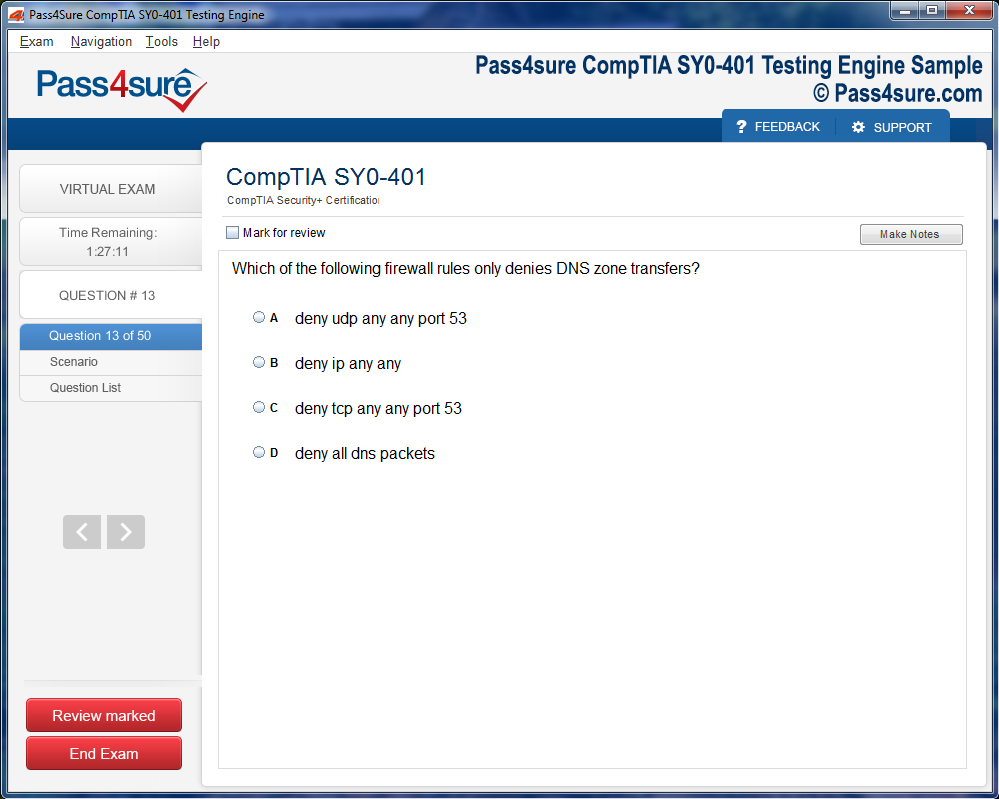
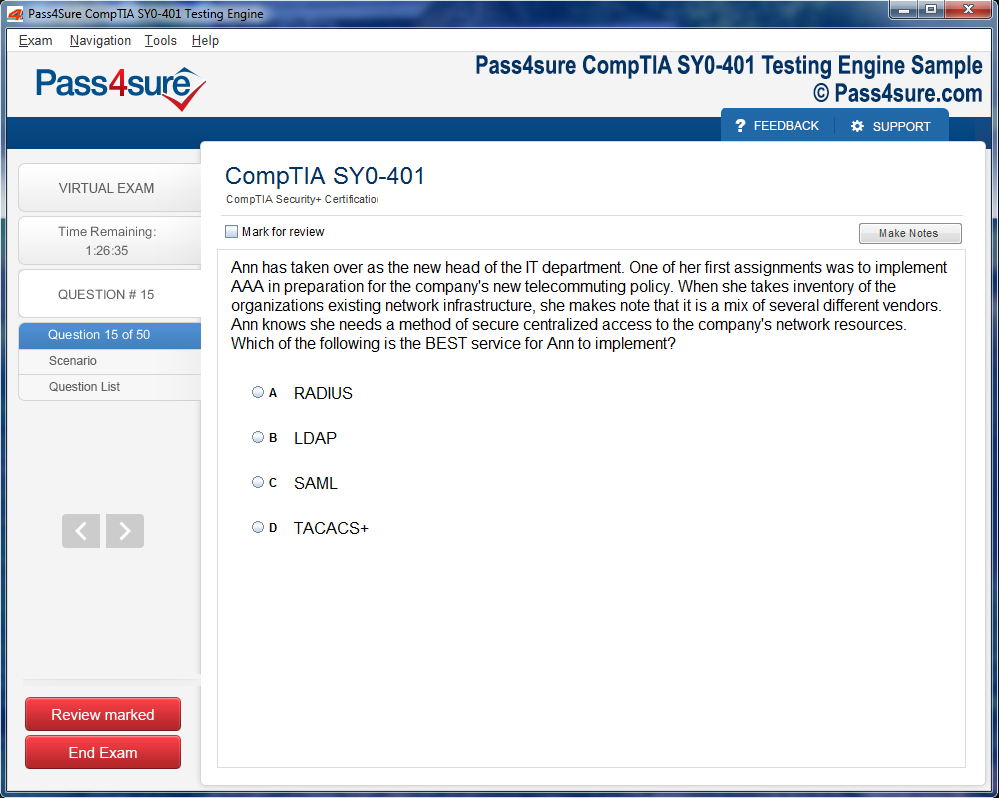
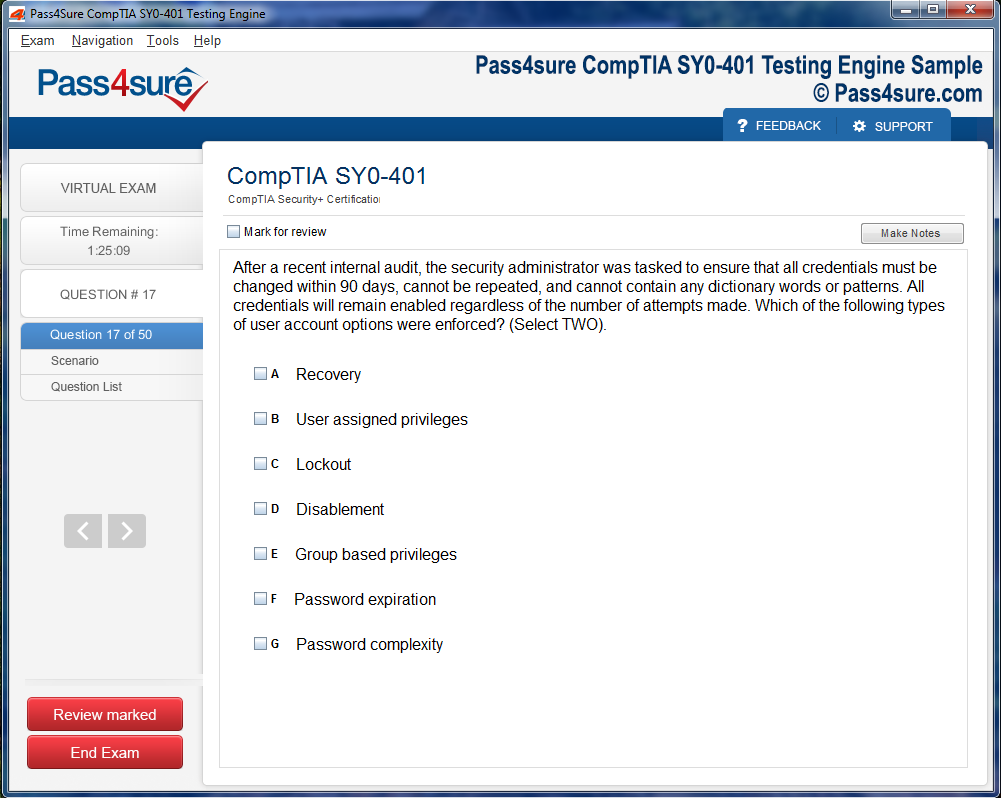
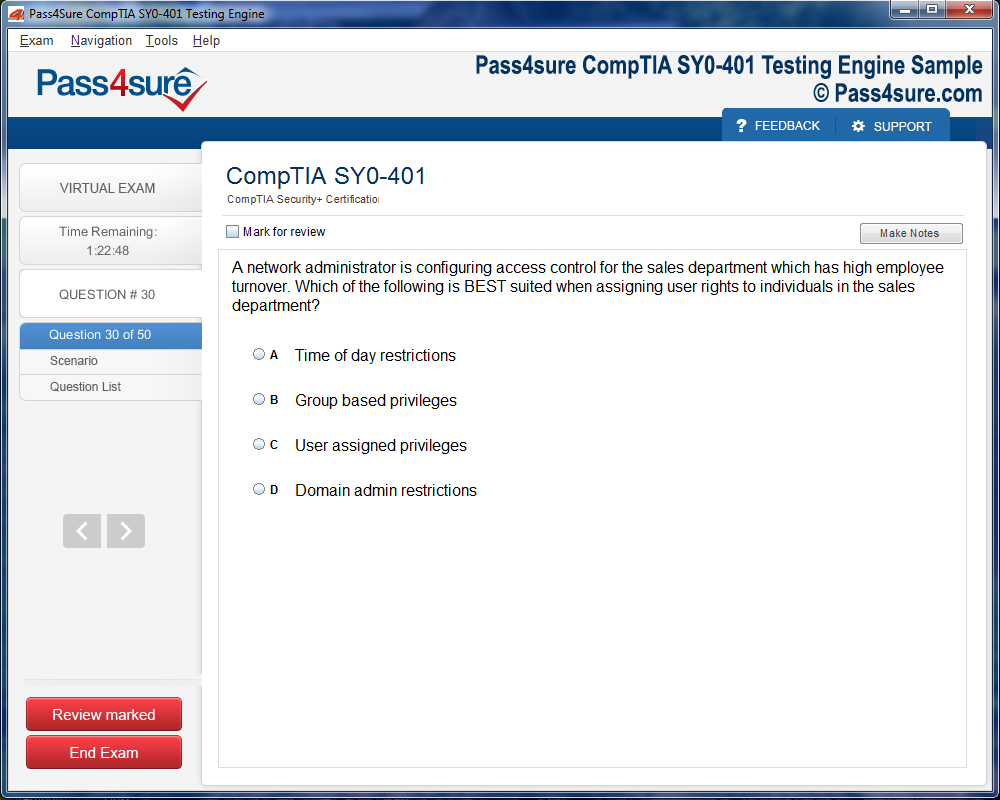
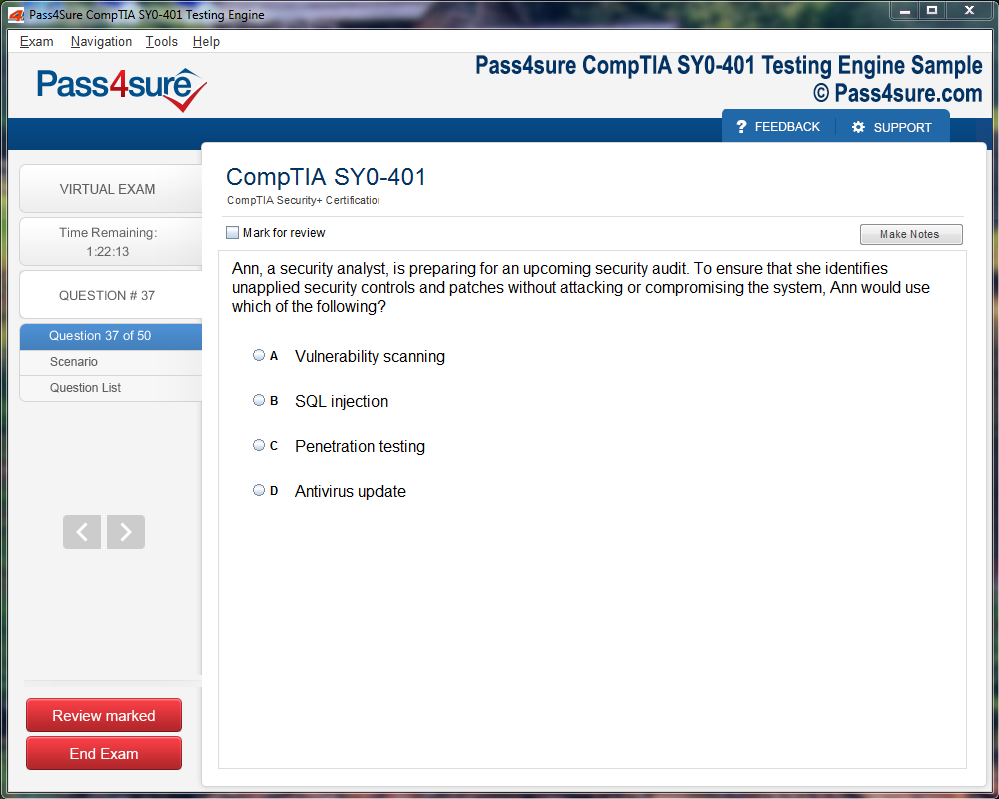
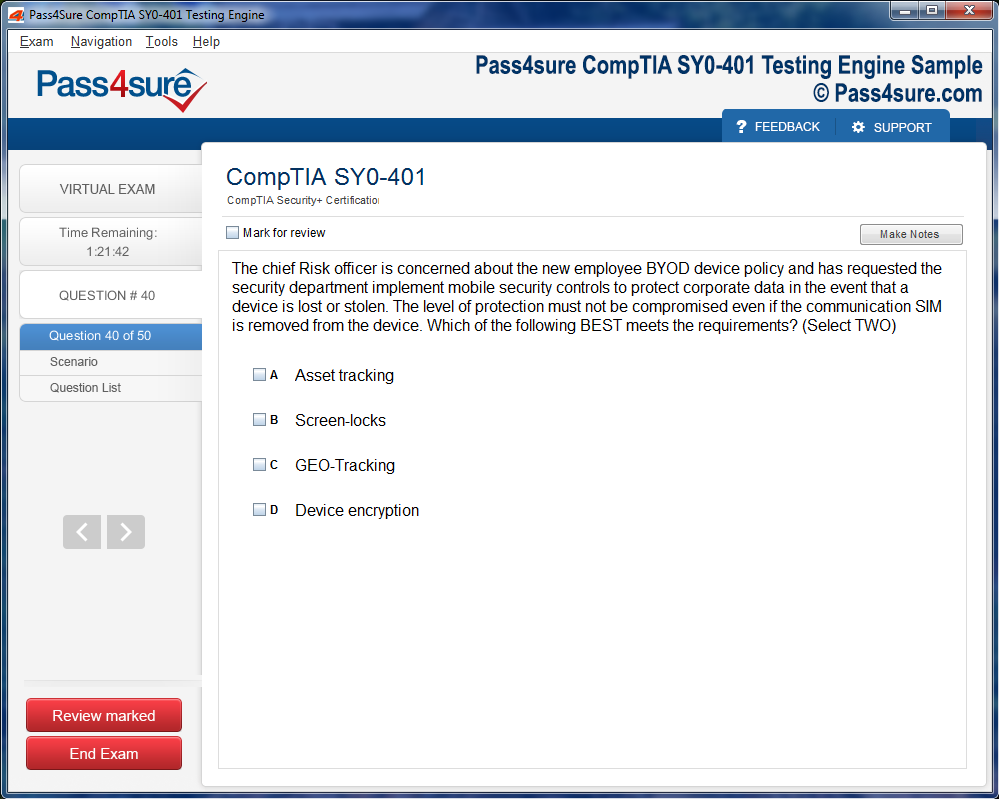
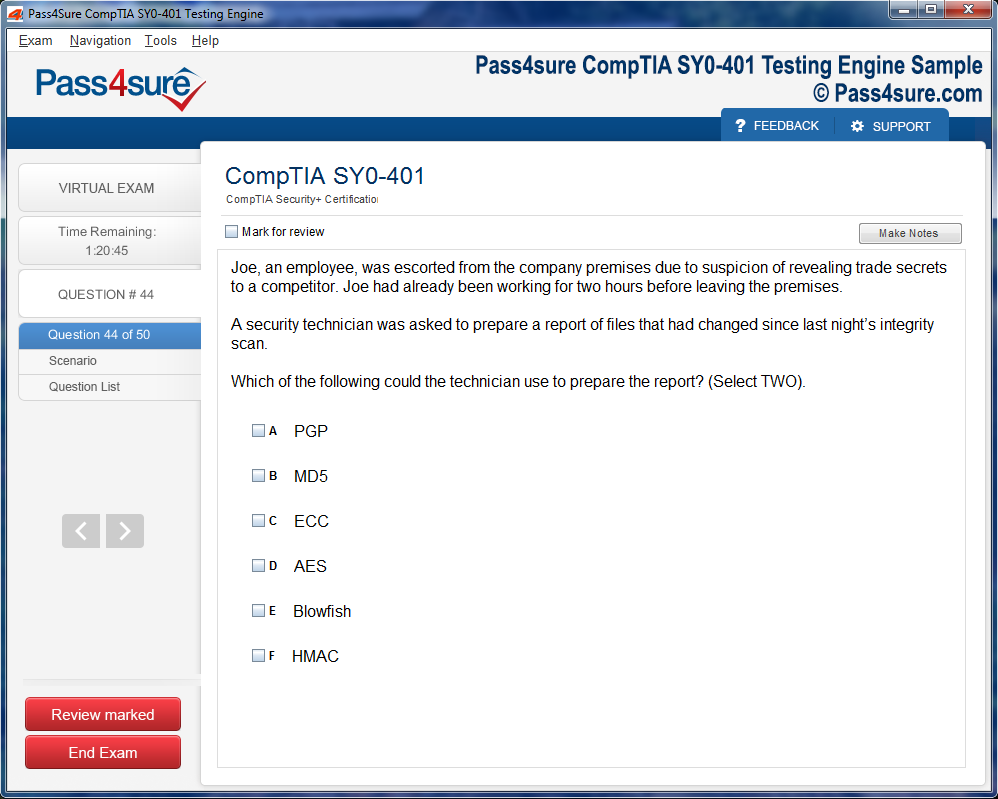
Product Screenshots
Frequently Asked Questions
How does your testing engine works?
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations.
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.
The Ultimate Handbook for HAAD-RN Exam Preparation
Cognitive agility in the HAAD-RN exam transcends rote memorization, demanding perspicacity and nuanced discernment. Nurses are evaluated on their capacity to synthesize multifaceted clinical data and prognosticate patient outcomes. This entails the ability to discriminate between corollary symptoms and pathognomonic indicators, to preempt complications, and to orchestrate care sequences with impeccable temporal acuity.
A critical element of cognitive preparation is cultivating metacognition—the awareness of one’s own thought processes. Reflective practice allows candidates to recognize cognitive biases that could skew clinical judgment, such as anchoring on initial impressions or succumbing to confirmation bias. Engaging in deliberate scenario-based exercises fosters cognitive elasticity, enabling swift adaptation to atypical presentations, which often occur in acute care settings.
Mastery of complex diagnostic algorithms is indispensable. For example, discerning between Type 1 and Type 2 diabetes mellitus in a patient exhibiting polyuria and polydipsia requires an intricate understanding of pathophysiology, biochemical markers, and patient history nuances. High-stakes scenarios, such as managing a patient with acute myocardial infarction, require rapid assimilation of cardiac biomarkers, ECG interpretations, and pharmacologic interventions. These exercises refine the mind’s ability to navigate labyrinthine clinical predicaments with dexterity.
Technical Proficiency: Beyond Procedural Competence
Technical aptitude extends beyond mere execution of procedures; it embodies anticipatory awareness and strategic precision. The HAAD-RN exam scrutinizes competencies ranging from intravenous therapy, tracheostomy care, and complex wound management to neonatal resuscitation and advanced cardiac life support protocols. Nurses must exhibit dexterity in utilizing sophisticated medical apparatus while simultaneously ensuring patient safety and comfort.
Simulation-based preparation has emerged as a cardinal strategy. High-fidelity mannequins and virtual patient encounters allow aspirants to rehearse intricate interventions under controlled stress conditions. This cultivates procedural memory and reduces performance anxiety during the examination. Meticulous attention to aseptic technique, pharmacokinetics, and equipment calibration reflects both technical mastery and adherence to rigorous clinical standards.
Furthermore, understanding the pharmacologic landscape is paramount. Candidates must navigate an extensive pharmacopeia, recognizing indications, contraindications, and adverse effect profiles. Integration of drug-drug interactions, renal and hepatic considerations, and patient-specific modifiers demonstrates the nuanced proficiency expected by examiners. This technical lexicon of medication management often distinguishes top performers from average candidates.
Ethical Acumen in Multifaceted Healthcare Scenarios
Ethical competency represents a pillar of professional nursing practice, challenging candidates to reconcile theoretical principles with pragmatic exigencies. The HAAD-RN exam presents scenarios where moral discernment is tested, such as conflicts between patient autonomy and medical necessity, or allocation of scarce resources in critical care settings.
Candidates must internalize frameworks such as principlism—balancing beneficence, non-maleficence, autonomy, and justice—while navigating culturally sensitive dilemmas intrinsic to the UAE. For instance, considerations around family involvement in end-of-life decision-making necessitate both ethical perspicacity and cultural fluency. Case-based questioning evaluates the ability to deliberate ethically under temporal pressure, ensuring patient-centric care without compromising professional integrity.
Augmenting ethical preparation involves reflective journaling, peer discourse, and engagement with real-world clinical conundrums. Awareness of institutional policies, legal precedents, and patient rights fortifies candidates’ ability to negotiate complex ethical landscapes. This amalgamation of cognitive reflection and contextual understanding exemplifies the sophistication expected in HAAD-RN ethical evaluation.
Decoding the Multifaceted Question Taxonomy
The HAAD-RN examination employs a kaleidoscopic array of question types, each engineered to probe distinct cognitive strata. Multiple-choice questions often test foundational knowledge, while situational judgment items assess analytical thinking and prioritization skills. Case-based scenarios demand integrative reasoning, blending pathophysiologic understanding, procedural proficiency, and ethical acumen into coherent decision-making.
Situational questions frequently simulate high-stakes clinical environments. A patient presenting with tachycardia, hypotension, and confusion may represent early septic shock. Candidates must swiftly recognize red-flag symptoms, initiate protocolized interventions, and communicate effectively with the multidisciplinary team. Success hinges on not merely knowing what to do, but understanding why each action is temporally and clinically imperative.
Cognitive rehearsal and iterative practice with such question formats enhance pattern recognition, decision-making efficiency, and situational adaptability. Utilizing diverse question banks, timed practice sessions, and analytical review of incorrect responses allows aspirants to internalize both content and strategic test-taking skills.
Cultivating Cognitive Tenacity for HAAD-RN
Cognitive tenacity transcends mere memorization; it embodies the ability to synthesize complex medical scenarios and render judicious decisions. Developing this faculty requires deliberate exposure to multifarious clinical vignettes. Rather than superficial familiarity, immerse yourself in labyrinthine case studies encompassing cardiac arrhythmias, septic shock, and multisystem pathologies. Contemplate potential complications, anticipate interventional priorities, and articulate rationale sequences with meticulous precision. The mind, when conditioned through such rigorous mental gymnastics, gains resilience against the ambiguities inherent in real-time examination dilemmas.
The Alchemy of Multisensory Learning
Engaging multiple sensory channels significantly amplifies knowledge retention. Auditory reinforcement, such as verbalizing procedures or dictating patient assessments, synergizes with visual stimuli like anatomical diagrams or pharmacological flowcharts. Kinesthetic interaction, through skill simulations or model-based practice, consolidates muscle memory essential for procedural mastery. This triad—auditory, visual, and kinesthetic—transforms ephemeral information into enduring cognition, offering aspirants a cognitive scaffold capable of sustaining nuanced clinical reasoning under temporal constraints.
Neuroplasticity and Strategic Repetition
The concept of neuroplasticity underpins all effective study paradigms. Repeated exposure to intricate information reshapes synaptic pathways, fortifying recall efficiency. Implement a scaffolded approach to repetition: commence with high-frequency review sessions for foundational topics, gradually transitioning to lower-frequency, integrative revisions encompassing case amalgamations. Utilize mnemonic stratagems and semantic clustering to entrench pathophysiological sequences, ensuring that pharmacological mechanisms, clinical presentations, and procedural protocols coalesce into a coherent mental lattice.
Immersive Scenario-Based Drills
Simulated clinical encounters are a crucible for cognitive endurance. Engage in scenario-based drills encompassing emergent, acute, and chronic conditions. Each session should incorporate unpredictable variables, compelling adaptive thinking. For example, modify patient vitals or introduce comorbidities during cardiovascular scenarios. Such deliberate perturbations cultivate analytical dexterity, enabling aspirants to navigate the labyrinth of HAAD-RN questions with alacrity and accuracy. Peer-to-peer simulations can further enrich this process by providing immediate feedback and exposing subtle misconceptions.
Metacognition and Reflective Analysis
Metacognitive awareness empowers aspirants to monitor their cognitive strategies and identify gaps in comprehension. Maintain a reflective log post-study sessions, noting areas of uncertainty, recurrent errors, and topics eliciting cognitive friction. Periodically revisit these entries to discern patterns and recalibrate study priorities. This self-auditing mechanism ensures that preparation evolves from rote repetition to dynamic, insight-driven mastery, allowing learners to preemptively address vulnerabilities before they manifest in high-stakes examination settings.
Optimizing Temporal Cadence
Temporal orchestration of study sessions can substantially influence retention and cognitive stamina. Embrace chronobiological insights by scheduling complex analytical tasks during peak alertness periods, typically morning hours for most individuals. Interleave high-intensity study blocks with restorative intervals, employing techniques such as the Pomodoro method to preserve attentional acuity. This temporal calibration prevents cognitive atrophy, mitigates burnout, and optimizes the absorption of multifaceted clinical knowledge essential for HAAD-RN success.
Cognitive Cross-Training Through Interdisciplinary Exposure
Expanding intellectual horizons beyond nursing-specific curricula enriches problem-solving dexterity. Delve into disciplines such as clinical psychology, biostatistics, and medical ethics to cultivate lateral thinking. Exposure to diverse analytical frameworks equips aspirants to interpret unconventional question stems, assess risk-benefit paradigms, and apply evidence-based judgment with nuanced sophistication. Interdisciplinary cross-pollination thus functions as a cognitive crucible, refining the capacity to navigate the spectrum of HAAD-RN challenges with agility and discernment.
Emotional Resilience as an Examination Catalyst
Equally paramount to intellectual preparation is the cultivation of emotional resilience. High-stakes examinations impose cognitive stress that can distort reasoning. Implement mindfulness protocols, diaphragmatic breathing, and guided visualization to fortify emotional equilibrium. Periodic reflection on personal achievements, coupled with incremental goal-setting, reinforces self-efficacy. The aspirant who navigates the nexus of intellectual rigor and emotional stability is primed not only for examination success but for sustainable clinical excellence.
Integrative Knowledge Mapping
Constructing intricate mental schemas facilitates the organization of voluminous information. Employ integrative mapping techniques, connecting pathophysiology, pharmacology, procedural guidelines, and patient safety considerations into unified conceptual frameworks. Visual diagrams, color-coded matrices, and hierarchical charts transform disparate data points into an accessible cognitive lattice. This structural consolidation enables rapid retrieval during time-pressured examination conditions, mitigating the cognitive load and enhancing decision-making fluidity.
Adaptive Resource Utilization
Effective HAAD-RN preparation necessitates judicious selection of resources. Prioritize high-yield materials that synthesize complex information into accessible formats without sacrificing depth. Incorporate mobile platforms, interactive modules, and peer-reviewed literature for dynamic engagement. Critically evaluate each source for relevance, accuracy, and currency. By cultivating discernment in resource utilization, aspirants avoid cognitive saturation from superfluous materials while optimizing learning efficiency.
The Nuances of Differential Diagnosis in Complex Cases
Differential diagnosis is the fulcrum upon which clinical acumen pivots. Discerning subtle manifestations of disease requires meticulous observation, cognitive flexibility, and pattern recognition. For example, tachypnea may signify a spectrum of conditions ranging from metabolic acidosis to early sepsis. Nurses must sift through multifarious symptoms, laboratory indices, and patient history to triangulate the most plausible etiology.
Case-based exercises accentuate diagnostic reasoning. Presenting nurses with polymorbid patients cultivates the ability to weigh probabilities and anticipate cascading complications. Engaging with atypical presentations—such as silent myocardial infarctions in diabetic patients or covert infections in immunocompromised individuals—hones vigilance and cognitive agility.
Furthermore, interprofessional collaboration enhances diagnostic precision. Consulting with physicians, pharmacists, and allied health professionals ensures comprehensive evaluation and mitigates cognitive biases. In exam scenarios, demonstrating adeptness at coordinating multidisciplinary input can distinguish high-performing candidates from the merely competent.
Strategic Prioritization in Nursing Interventions
Prioritization transcends rote task management; it embodies the art of triaging interventions to maximize patient outcomes. The HAAD-RN examination often probes scenarios demanding instantaneous assessment and judicious allocation of resources. A patient with hemodynamic instability, electrolyte derangements, and acute pain requires layered decision-making that integrates urgency, risk, and prognostic significance.
Employing frameworks such as the ABCDE (Airway, Breathing, Circulation, Disability, Exposure) paradigm fosters methodical prioritization. However, seasoned nurses transcend algorithms by incorporating situational awareness, patient preferences, and environmental variables. Exercises that simulate overlapping crises—respiratory distress concurrent with a hypoglycemic episode—cultivate both decisiveness and composure under pressure.
Time-sensitive interventions, such as rapid insulin administration or emergent oxygen therapy, underscore the importance of anticipatory planning. In addition, reflective practice, wherein nurses evaluate the impact and sequencing of their actions, reinforces cognitive resilience and adaptive judgment.
Ethical Conundrums and Cultural Sensitivity
Navigating ethical conundrums requires dexterity in balancing moral principles with pragmatic clinical realities. Patient autonomy, beneficence, nonmaleficence, and justice often converge in intricate patterns that defy simplistic resolution. Nurses may encounter scenarios where familial expectations conflict with the patient’s informed choices or where resource limitations necessitate triage decisions.
Cultural competence amplifies ethical discernment. Understanding UAE-specific mores, religious considerations, and familial dynamics is indispensable for patient-centered care. Simulation exercises that embed ethical dilemmas—such as withholding aggressive interventions in terminally ill patients—sharpen moral reasoning and the ability to articulate rationale coherently.
Documentation of ethical deliberations further consolidates professional integrity. Maintaining detailed records of informed consent discussions, cultural considerations, and decision-making processes safeguards both patient welfare and regulatory compliance.
Pharmacological Vigilance and Therapeutic Nuances
Pharmacological vigilance extends beyond memorization; it embodies a holistic comprehension of therapeutic intent, mechanistic action, and patient-specific modulation. Nurses must anticipate drug-drug interactions, recognize early toxicity signals, and tailor interventions to individual physiology. Administering nephrotoxic agents in patients with borderline renal function exemplifies the delicate balance between therapeutic benefit and iatrogenic risk.
High-yield exam preparation involves dissecting case scenarios for pharmacodynamic subtleties. Consider polypharmacy in geriatric patients, where altered pharmacokinetics magnifies vulnerability to adverse effects. Equally, understanding temporal factors—such as peak plasma concentrations and half-life variations—enhances precision in scheduling and monitoring.
Simulation exercises incorporating medication administration and complication management fortify both competence and confidence. Repetitive engagement with scenarios such as anticoagulant titration or insulin dose adjustment instills an instinctive, reflexive approach that transcends theoretical knowledge.
High-Fidelity Clinical Simulations and Procedural Mastery
Simulation-based learning accelerates procedural mastery while mitigating patient risk. High-fidelity mannequins and immersive virtual environments provide tactile, cognitive, and emotional rehearsal for complex interventions. Intravenous line insertion, central venous catheter management, and emergency resuscitation can be practiced iteratively to achieve fluency.
Observational acuity during simulation is as critical as procedural skill. Detecting subtle changes in vital signs or early manifestations of adverse reactions requires integrated sensory and cognitive processing. Structured debriefings post-simulation reinforce learning by illuminating errors, reinforcing correct technique, and promoting adaptive reasoning.
Procedural competence is inseparable from anticipatory planning. A nurse preparing for airway management, for instance, must orchestrate equipment readiness, monitor patient parameters, and anticipate potential complications. The integration of technical skill with situational foresight epitomizes professional excellence and is frequently assessed in high-stakes licensure examinations.
Precision in Documentation and Information Synthesis
Accurate documentation is the silent scaffold upon which effective patient care rests. Beyond recording vital signs, nurses synthesize observations, interventions, and patient responses into coherent, actionable narratives. The HAAD-RN exam often evaluates the ability to discern pertinent details, organize information chronologically, and update electronic medical records with precision.
Cognitive clarity during documentation prevents errors, enhances continuity of care, and supports medico-legal integrity. Incorporating structured frameworks—SOAP (Subjective, Objective, Assessment, Plan) or PIE (Problem, Intervention, Evaluation)—streamlines information synthesis and facilitates rapid retrieval.
Moreover, documentation functions as a cognitive tool, reinforcing reflective practice. Recording clinical reasoning, intervention rationale, and anticipated outcomes consolidates experiential knowledge, promotes self-assessment, and prepares nurses for complex future scenarios.
The Art of Deliberate Question Practice
Engaging in deliberate question practice is far more than mere repetition; it is a methodical choreography of cognition and retention. Aspirants should approach practice questions with an analytical lens, dissecting each query as if unraveling a complex tapestry. Recognize subtle cues, differentiate between plausible distractors, and internalize the nuance embedded in wording. Precision in interpretation often dictates success more than rote knowledge.
Prioritize questions that compel higher-order reasoning rather than simple recall. Conceptual entanglement, scenario-based dilemmas, and multi-step clinical decision-making foster synaptic agility. Employ techniques such as the process-of-elimination with layered scrutiny, rather than cursory guesswork. This cultivates a mental architecture robust enough to withstand the labyrinthine nature of high-stakes examinations.
Strategic Integration of Topic-Specific Drills
Isolated, subject-specific drills fortify the bedrock of knowledge. Dive into areas prone to complexity or frequent misconceptions, such as hematology, neonatal care, or psychiatric interventions. Targeted drills should not merely echo textbook material; they should interrogate the student’s ability to apply principles under varying contexts. Repetition, when coupled with incremental difficulty, enforces neural reinforcement, transforming tentative knowledge into automaticity.
Rotate through subjects in an orchestrated cadence to prevent cognitive stagnation. Microcycles of focused practice interspersed with interleaved topics cultivate adaptive thinking, ensuring a nimble response to unpredictable question frameworks. This is particularly crucial in examinations where interdisciplinary connections are tested through composite clinical vignettes.
Mastering Mock Exams as Cognitive Simulators
Mock examinations function as cognitive simulators, reproducing the pressure, tempo, and intricacies of actual testing environments. Full-length mocks are not exercises in endurance alone; they are instruments for metacognitive calibration. Tracking time per question, observing decision fatigue, and gauging attention drift are equally critical as scoring accuracy.
Post-mock analysis must be exhaustive. Examine not only which answers were incorrect but why each distractor was persuasive. Such scrutiny sharpens judgment and illuminates latent conceptual ambiguities. Annotate insights meticulously, creating a personalized repository of patterns in errors, recurring themes, and knowledge blind spots, which serves as an evolving blueprint for further practice.
The Imperative of Rationale Engagement
Absorbing rationales is an often-overlooked yet transformative strategy. Understanding the cognitive underpinnings behind correct choices cultivates discernment and diagnostic acuity. For instance, discerning the most appropriate intervention for a hypotensive post-operative patient requires more than memorization; it demands prioritization, temporal reasoning, and comprehension of pathophysiological trajectories. Rationales elucidate these layers, converting abstract knowledge into operational competence.
Documenting rationales and revisiting them periodically strengthens long-term retention. Cross-referencing rationales with prior errors fosters a dialectic approach, wherein knowledge gaps are not merely recognized but systematically rectified. This practice engenders intellectual resilience and a proactive mindset toward continuous improvement.
Reflective Synthesis After Practice
Reflection transforms routine practice into strategic growth. After each session, distill key lessons, identify recurring pitfalls, and recalibrate learning strategies. Consider questions that provoked hesitation, distractor patterns that misled, and mental shortcuts that yielded errors. Such reflective synthesis cultivates metacognition, the awareness of one’s own thought processes, which is indispensable in high-stakes clinical examinations.
Maintaining a reflective journal enhances the process, providing a longitudinal view of progress. Over time, patterns emerge: weaknesses become identifiable, strengths crystallize, and study strategies evolve. This self-dialogue encourages intentionality in learning, converting mistakes into stepping stones rather than obstacles.
Cognitive Rest and Efficiency Management
Cognitive endurance is as crucial as knowledge mastery. Overexertion without intervals breeds fatigue, reducing both comprehension and retention. Implement micro-rests, alternating high-intensity practice with brief periods of mental recuperation. Techniques such as spaced repetition, focused meditation, or simple physical movement revitalize mental acuity.
Efficiency is not measured by volume alone but by the quality of engagement during each session. Even short, focused practices surpass marathon, unstructured study in fostering durable mastery. This equilibrium of exertion and rest ensures sustainable performance and prevents the insidious erosion of cognitive clarity over prolonged preparation periods.
Temporal Orchestration and Cerebral Pacing
Mastery over temporal orchestration is indispensable for aspirants confronting intellectually demanding assessments such as the HAAD-RN. Constructing an intricate schema of study intervals, revision junctures, and reflective pauses ensures a symphony of mental agility rather than a cacophony of chaotic cramming. Segment topics into digestible epistemic clusters, interspersed with rehearsal of intricate clinical paradigms. Establish quotidian or hebdomadal benchmarks, emphasizing high-yield material while relegating peripheral topics to ancillary reinforcement. The sagacious allocation of cognitive resources mitigates entropy and fosters retention with minimal cognitive attrition.
Neuropsychological Resilience and Anxiety Modulation
The cerebration required for sustained examination performance is inextricably linked to neuropsychological equilibrium. Implementing techniques that attenuate sympathetic overactivation—such as diaphragmatic respiration, somatic scanning, and guided imagery—cultivates a serene cognitive substrate. Visualizing triumphant navigation of challenging scenarios engenders anticipatory self-efficacy, a potent psychological bulwark against anticipatory stress. Strategically interspersed micro-respites during study epochs facilitate synaptic consolidation and prevent neurocognitive fatigue, preserving vigilance for analytical reasoning tasks.
Tactical Examination Cognition
Optimal performance on exam day necessitates tactical cognitive deployment. Engage in meticulous reconnaissance of the testing environment and procedural prerequisites to reduce extraneous cognitive load. Approach each interrogative with deliberate scrutiny; resist the cognitive pitfall of precipitous selection. For complex clinical vignettes, mentally architect intervention schemas prior to option appraisal. Chronometric awareness is paramount: pacing should accommodate initial problem-solving and final review iterations without inducing hurried errors. The judicious partitioning of temporal resources functions as both cognitive scaffolding and anxiety attenuator.
Scenario Rehearsal and Cognitive Preconditioning
Simulated confrontation with hypothetical quandaries primes the mind for exigent circumstances. Mental rehearsal of adverse contingencies—including technical malfunctions, ambiguous prompts, or multi-layered patient scenarios—cultivates anticipatory adaptability. Such cognitive preconditioning enhances executive function under duress and fortifies emotional resilience. Repeated exposure to high-stakes simulations fosters procedural memory, ensuring that analytical fluency emerges instinctively rather than reactively during actual examination conditions.
Reflexive Iteration and Growth-Oriented Cognition
Adopting a perspective of reflexive iteration transforms errors into instruments of skill refinement. Each misstep during practice sessions serves as a micro-laboratory for procedural recalibration and analytical augmentation. A mindset anchored in progressive mastery rather than static perfectionism engenders intellectual plasticity. Persistent, strategic engagement with both foundational principles and nuanced clinical contingencies cultivates an epistemic robustness that withstands temporal pressures and cognitive perturbations. In this cognitive paradigm, disciplined preparation, iterative rehearsal, and anticipatory strategizing converge to scaffold peak performance.
Embedding Theoretical Acumen into Clinical Praxis
Transmuting theoretical acumen into tangible clinical praxis is paramount for post-exam excellence. The cognitive scaffolding developed during HAAD-RN preparation must be actively reconciled with quotidian patient care. Reflection becomes an indispensable tool; scrutinize each clinical decision, parsing nuances between protocol adherence and individualized patient needs. Integrating pathophysiological insights with real-time assessment cultivates an elevated level of clinical perspicacity.
The Imperative of Continuing Professional Development
Continuing Professional Development (CPD) is not merely a regulatory requisite; it constitutes the sine qua non of sustained expertise. Engage in immersive workshops, symposia, and digital colloquia to remain attuned to the evolving intricacies of UAE healthcare legislation, novel pathogeneses, and emergent therapeutic modalities. CPD cultivates a dynamic cognitive elasticity, ensuring practitioners are perpetually adept in their specialty. Such endeavors also fortify one’s professional dossier, augmenting prospects for leadership and advanced practice roles.
Synergistic Networking and Peer Enrichment
Professional vitality is inextricably linked to collegial synergies. Active networking through nursing guilds, digital fora, and interdisciplinary conferences fosters a vibrant exchange of esoteric knowledge. Discussing multifaceted cases, juxtaposing experiential paradigms, and offering reciprocal mentorship engenders a collective intelligence that surpasses isolated learning. These interactions catalyze both cognitive enrichment and emotional sustenance, reinforcing resilience against occupational stressors.
Evidence-Based Practice as a Pillar of Competence
In an era dominated by empirical rigor, evidence-based practice remains an indispensable fulcrum of clinical excellence. Continually recalibrate your therapeutic approach in alignment with emergent guidelines, pharmacological innovations, and investigative studies. Cultivating research literacy empowers nurses to discern robust evidence from anecdotal convention, ensuring patient care is both efficacious and defensible. This perpetual engagement with contemporary literature embodies professional accountability and intellectual rigor.
Documentational Mastery and Analytical Acuity
Documentation transcends administrative formality; it is an epistemic tool that chronicles clinical reasoning and safeguards continuity of care. Mastery of charting, nuanced patient histories, and meticulous reporting fosters both operational clarity and legal compliance. Analytical acuity, intertwined with precise documentation, allows practitioners to detect subtle physiological aberrancies and preempt adverse events, thereby elevating patient outcomes and reinforcing the credibility of the nursing profession.
Cultivating Resilience and Emotional Dexterity
Healthcare is a crucible of emotional and cognitive demands. Post-exam, the cultivation of resilience is not optional; it is imperative. Develop emotional dexterity, cultural acumen, and situational adaptability to navigate the vicissitudes of patient care. Mindful self-regulation, stress inoculation strategies, and reflective practices serve as scaffolds for sustained professional engagement. These qualities not only safeguard mental well-being but also enhance the capacity for compassionate, patient-centered care.
Integrating Mentorship and Reciprocal Learning
Mentorship functions as a bidirectional conduit for experiential wisdom and novel insights. By mentoring novice practitioners and simultaneously seeking guidance from seasoned clinicians, nurses engage in a continuous feedback loop that refines both practical skills and strategic judgment. This symbiotic exchange fosters professional solidarity, reinforces clinical confidence, and accelerates the internalization of complex procedural knowledge.
Advancing Specialization and Niche Expertise
Beyond foundational practice, specialization within clinical niches is a pathway to distinction. Focused expertise in areas such as critical care, infectious disease management, or pediatric oncology amplifies professional influence and positions practitioners as authoritative resources within their domains. Pursuing certifications, sub-specialty training, and targeted research ensures that one’s skill set remains both relevant and indispensable in an ever-evolving healthcare ecosystem.
Harnessing Digital Platforms for Knowledge Expansion
The contemporary healthcare landscape is increasingly mediated by digital platforms, which can be leveraged for asynchronous learning, peer discourse, and rapid dissemination of guidelines. Curated e-libraries, virtual simulation modules, and interactive case studies provide immersive avenues for knowledge consolidation. Proficiency in digital fluency not only augments clinical competence but also cultivates adaptability to technology-driven healthcare innovations.
Balancing Professional Obligations with Personal Growth
Sustained excellence is contingent upon a harmonious integration of professional rigor and personal enrichment. Strategic time management, reflective journaling, and deliberate self-care rituals buffer against occupational fatigue and cognitive depletion. By maintaining equilibrium between vocational duties and holistic well-being, practitioners cultivate enduring efficacy and satisfaction in their professional trajectories.
Cultivating Analytical Vigilance in Clinical Environments
Analytical vigilance constitutes the bedrock of sustained clinical excellence. Nurses must engage in continuous cognitive calibration, dissecting symptomatology with meticulous scrutiny to discern subtle deviations from normative physiology. Employing diagnostic heuristics in tandem with evidence-based protocols enhances precision and mitigates clinical ambiguity. Reflexive analysis—where past decisions are interrogated for efficacy and potential improvement—amplifies both cognitive flexibility and decision-making acumen.
Strategic Implementation of Interdisciplinary Collaboration
Interdisciplinary collaboration transcends conventional teamwork by fostering a syncretic approach to patient care. Engaging with physicians, pharmacists, physiotherapists, and allied health professionals cultivates holistic problem-solving capabilities. Structured communication frameworks, such as SBAR (Situation, Background, Assessment, Recommendation), augment clarity and minimize the risk of clinical misinterpretation. Such strategic partnerships facilitate a harmonized therapeutic trajectory, ensuring patient outcomes are optimized and clinical redundancy minimized.
Mastery of Pharmacological Nuances
Pharmacological mastery is not limited to rote memorization of drug regimens; it encompasses an intricate understanding of pharmacokinetics, pharmacodynamics, and adverse interaction potential. Nurses must continually update their pharmacopeia knowledge to accommodate new agents, evolving therapeutic guidelines, and population-specific dosage modifications. This depth of understanding ensures that medication administration transcends procedural compliance, becoming a deliberative, evidence-driven intervention that maximizes efficacy and patient safety.
Leveraging Reflective Practice for Cognitive Enrichment
Reflective practice serves as both a metacognitive and professional enrichment tool. By systematically examining clinical encounters, nurses refine their interpretive frameworks, identify latent biases, and enhance patient-centered judgment. Techniques such as Gibbs’ reflective cycle or the Schön model facilitate structured contemplation, enabling practitioners to translate introspective insights into actionable improvements. Over time, reflective practice cultivates a heightened sense of situational awareness, anticipatory problem-solving, and nuanced empathy.
Navigating Ethical Complexities in Healthcare Delivery
Healthcare is replete with ethical intricacies requiring judicious discernment. Post-exam nurses encounter dilemmas surrounding autonomy, confidentiality, beneficence, and resource allocation. Engaging with ethical frameworks, institutional policies, and case-based discourse equips practitioners to navigate these complexities with integrity and consistency. Ethical literacy ensures that clinical decisions are morally defensible, culturally sensitive, and aligned with both patient welfare and professional standards.
Augmenting Cultural Competence in Multicultural Contexts
The UAE presents a uniquely multicultural healthcare environment, demanding elevated cultural competence. Understanding sociocultural determinants of health, religious nuances, and language variations enhances patient rapport and care efficacy. Nurses must employ culturally attuned communication strategies, leverage interpreters judiciously, and respect divergent health beliefs while maintaining evidence-based interventions. Cultivating this competence reduces care disparities, enhances patient satisfaction, and fortifies professional credibility.
Strategic Time Management and Prioritization Skills
Post-exam professional growth necessitates mastery over temporal dynamics in clinical practice. Effective time management is more than task sequencing; it entails prioritizing interventions based on acuity, resource availability, and patient safety imperatives. Utilizing tools such as the Eisenhower Matrix or acuity-based scoring systems facilitates decisive allocation of attention and effort. Nurses who refine these skills optimize workflow efficiency, mitigate burnout, and maintain a proactive stance in fast-paced care environments.
Enhancing Patient Education and Health Literacy
Patient education is a critical vector for improving health outcomes and fostering self-efficacy. Nurses must distill complex medical information into comprehensible, actionable guidance tailored to individual literacy levels and cultural contexts. Employing visual aids, teach-back methodologies, and motivational interviewing techniques enhances comprehension and adherence. This strategic investment in patient literacy reduces readmission rates, fosters preventive care, and positions the nurse as a pivotal agent in health promotion.
Integrating Simulation-Based Learning for Clinical Proficiency
Simulation-based learning offers a dynamic conduit for translating theoretical knowledge into procedural mastery. High-fidelity mannequins, virtual reality modules, and scenario-based drills cultivate technical skill, critical thinking, and rapid decision-making without patient risk. Consistent engagement with simulation fosters confidence, hones reflexive responses, and exposes practitioners to rare or emergent clinical presentations. Over time, simulation becomes an indispensable adjunct to experiential learning, bridging the gap between classroom theory and real-world practice.
Developing Leadership Acumen in Nursing Practice
Leadership acumen extends beyond hierarchical roles, encompassing informal influence, mentorship, and advocacy. Nurses who cultivate leadership skills excel in team coordination, conflict resolution, and strategic problem-solving. This includes fostering an environment that encourages knowledge-sharing, critical inquiry, and accountability. Leadership development initiatives—ranging from workshops to action-learning projects—enhance professional presence, prepare nurses for advanced roles, and amplify impact within the healthcare system.
Harnessing Research Literacy for Evidence-Informed Practice
Research literacy is pivotal in translating scientific discovery into clinical application. Nurses must adeptly interpret study design, statistical relevance, and translational applicability to inform practice decisions. Engaging with peer-reviewed journals, critically appraising research, and integrating findings into care plans ensures interventions are grounded in robust evidence. This intellectual rigor enhances credibility, promotes patient safety, and cultivates a culture of continuous inquiry within healthcare settings.
Optimizing Emotional Intelligence for Patient and Team Interactions
Emotional intelligence (EI) underpins effective interpersonal engagement, stress management, and adaptive problem-solving. High EI enables nurses to perceive, interpret, and regulate both personal and patient emotions, enhancing therapeutic relationships and mitigating workplace tension. Developing empathy, self-awareness, and social skills fosters trust, reduces conflict, and enhances team cohesion. In high-stakes environments, EI is a decisive factor in sustaining both professional efficacy and personal well-being.
Cultivating Adaptive Expertise for Evolving Healthcare Challenges
Adaptive expertise entails the ability to flexibly apply knowledge across novel, ambiguous, or complex scenarios. Post-exam, nurses confront rapidly shifting clinical landscapes, emergent diseases, and technological innovations. Cultivating adaptive expertise requires continuous learning, scenario rehearsal, and reflective integration of experience. This cognitive elasticity enables practitioners to innovate, problem-solve under uncertainty, and maintain optimal patient outcomes amidst evolving clinical challenges.
Strategic Utilization of Technology in Patient Care
Technological fluency is now integral to contemporary nursing practice. From electronic health records and telemedicine platforms to predictive analytics and wearable health monitors, nurses must integrate digital tools with clinical judgment. Leveraging technology enhances diagnostic accuracy, streamlines workflow, and facilitates real-time patient monitoring. Embracing digital competencies ensures practitioners remain at the forefront of healthcare innovation while delivering safe, efficient, and patient-centered care.
Fostering Interpersonal Resilience in High-Stress Environments
Healthcare environments are inherently stress-laden, necessitating robust interpersonal resilience. Cultivating coping strategies, peer support networks, and mindfulness practices mitigates emotional fatigue and enhances performance consistency. Resilient practitioners demonstrate sustained engagement, rapid recovery from adverse events, and a capacity to provide high-quality care under duress. Over time, resilience reinforces professional identity, fortifies mental health, and bolsters longevity within the nursing profession.
Engaging in Policy Advocacy and Healthcare Reform
Post-exam nurses are uniquely positioned to influence systemic healthcare transformation. Engaging with policy advocacy—through professional associations, community initiatives, or research dissemination—amplifies the nurse’s voice in legislative discourse. Understanding regulatory frameworks, health economics, and population health strategies equips practitioners to contribute meaningfully to reform efforts. Such engagement enhances the broader healthcare ecosystem while fostering a sense of agency and professional fulfillment.
Refining Critical Thinking Through Case-Based Learning
Critical thinking is honed through the iterative analysis of complex clinical cases. Employing structured frameworks, such as the nursing process or decision trees, cultivates systematic evaluation of patient presentations. Case-based learning exposes practitioners to a diversity of scenarios, enhancing diagnostic accuracy, prioritization skills, and contingency planning. This methodology reinforces cognitive agility, clinical intuition, and the capacity to synthesize disparate data points into coherent care strategies.
Integrating Global Best Practices into Local Healthcare Delivery
Post-exam professional growth involves synthesizing global nursing best practices with the specific exigencies of UAE healthcare. Comparative analysis of international protocols, cultural adaptation of interventions, and benchmarking against global standards fosters excellence. By contextualizing universal principles within local healthcare realities, nurses ensure that patient care is both innovative and culturally congruent. This integrative approach enhances outcomes, reinforces professional credibility, and positions practitioners as leaders in evidence-informed practice.
Leveraging Mentorship to Cultivate Future Nursing Leaders
Mentorship is a dynamic conduit for knowledge transfer, skill refinement, and professional socialization. Seasoned nurses who mentor juniors reinforce their own expertise while shaping the next generation of practitioners. Structured mentorship programs facilitate goal-setting, reflective feedback, and competency mapping, ensuring that learning is both personalized and strategic. This reciprocal exchange fosters resilience, professional identity, and a legacy of clinical excellence.
Cognitive Cartography and Conceptual Mapping
Navigating the labyrinthine expanse of medical knowledge necessitates a methodical approach akin to cognitive cartography. Map intricate interrelations among pathophysiology, pharmacology, and procedural interventions to construct a multidimensional mental atlas. Utilize mnemonic scaffolds, metaphorical associations, and schema integration to encode abstruse information into retrievable nodes. The act of conceptual mapping transforms diffuse knowledge into a structured lattice, permitting rapid retrieval under temporal duress and enhancing synaptic fidelity.
Revisitation of these cognitive maps through spaced repetition fortifies neural consolidation, embedding high-yield concepts in long-term memory. Interleave disparate subjects—such as pediatric pharmacology with geriatric pathophysiology—to cultivate cross-domain synthesis, a skill crucial for multifactorial problem-solving during the HAAD-RN examination. The deliberate juxtaposition of complex domains fosters lateral reasoning, allowing aspirants to discern patterns that elude linear study methods.
Psychophysiological Optimization for Peak Performance
The nexus of mental acuity and physiological homeostasis cannot be overstated. Optimizing circadian rhythms, nutritional intake, and somatic activity establishes a neurochemical milieu conducive to sustained concentration and executive function. Engage in moderate aerobic exercise to elevate cerebral perfusion and enhance neurotrophin synthesis, supporting both memory consolidation and analytical flexibility. Hydration and nutrient-dense sustenance ensure glucose stability, which underpins attentional control and mitigates cognitive lapses during prolonged study sessions.
Equally crucial is the management of psychophysiological stress markers. Chronic sympathetic overactivation erodes cognitive precision, while parasympathetic modulation—achieved through meditation, progressive muscle relaxation, and controlled respiratory rhythms—cultivates a neuroendocrine environment optimal for learning and retention. By attuning the body to a state of poised readiness, aspirants acquire not only stamina for intensive study but also resilience for high-pressure examination scenarios.
Strategic Simulation and Analytical Rehearsal
Simulation transcends rote memorization, offering a dynamic platform for procedural fluency and decision-making agility. Construct complex vignettes that replicate the unpredictable nature of clinical encounters. Engage in analytical rehearsal by dissecting each scenario, anticipating potential complications, and preemptively formulating interventions. This iterative cognitive rehearsal embeds procedural heuristics, reducing reaction latency and enhancing adaptive reasoning during actual examination conditions.
Incorporate error tracking as an analytical tool. Record recurrent miscalculations, ambiguous interpretations, or lapses in protocol comprehension. Subsequent deconstruction of these errors illuminates systemic gaps in knowledge and cognitive strategy. By transforming mistakes into diagnostic instruments, aspirants evolve a meta-cognitive awareness that streamlines subsequent study sessions and fortifies problem-solving under duress.
Temporal Segmentation and Micro-Scheduling
The human attentional apparatus exhibits a finite endurance for high-cognitive-load tasks. Effective temporal segmentation optimizes productivity by balancing intensive focus with restorative intervals. Deploy micro-scheduling, structuring study periods into concentrated bursts of 50–90 minutes interspersed with deliberate micro-pauses. During these intervals, engage in brief psychophysiological resets—hydration, stretching, or sensory modulation—to prevent cognitive entropy.
Strategically sequence study segments to exploit circadian peaks in attentional capacity. Allocate complex analytical tasks during periods of maximal alertness, reserving rote memorization or lighter review for cognitive troughs. This synchronization between temporal architecture and mental acuity enhances learning efficiency and prevents the deleterious effects of cognitive fatigue.
Metacognitive Vigilance and Adaptive Self-Monitoring
Success in high-stakes examinations is contingent upon rigorous metacognitive oversight. Cultivate an acute awareness of personal cognitive strengths and vulnerabilities, adapting study strategies accordingly. Employ reflective journaling to chronicle comprehension trajectories, emotional fluctuations, and problem-solving efficacy. This practice enables anticipatory adjustment of study intensity and focus, preventing plateauing of intellectual progress.
Adaptive self-monitoring extends into examination strategy itself. Evaluate each question not only for content accuracy but for strategic value—identifying high-impact items and judiciously allocating time. By integrating real-time metacognitive assessment, aspirants transform passive cognition into proactive, strategic engagement, mitigating the risks of misallocation or cognitive tunnel vision.
Neuroplasticity and Interdisciplinary Integration
Harnessing neuroplastic potential necessitates active engagement with varied and complex material. Interdisciplinary integration—melding physiology, pharmacology, ethics, and clinical judgment—stimulates neural networks and enhances associative reasoning. Construct comparative frameworks that juxtapose differing clinical approaches, ethical dilemmas, or pharmacotherapeutic regimens, cultivating a multifaceted cognitive lens.
Such integration not only reinforces memorization but also primes the mind for the unpredictable synthesis required by scenario-based questions. The deliberate cross-pollination of domains encourages flexible problem-solving, fostering the emergence of novel insights from seemingly disparate informational nodes. In this manner, neuroplastic engagement becomes both a tool for retention and a crucible for analytical sophistication.
Emotional Equanimity and Cognitive Poise
Examination performance is inextricably linked to the regulation of affective states. Emotional equanimity, achieved through deliberate psychological conditioning, enhances decision-making under duress. Techniques such as visualization, cognitive reframing, and anticipatory coping convert potential stressors into manageable cognitive stimuli.
Cultivate a mental environment where challenges are perceived not as threats but as structured opportunities for problem-solving. This recalibration of emotional response preserves cognitive bandwidth for analytical reasoning and prevents anxiety from triggering counterproductive heuristics, such as rushed decisions or over-reliance on intuition alone.
Dynamic Review and Iterative Reinforcement
Repetition is not mere recitation but an active, dynamic process of reinforcement. Engage with content through multidimensional review—auditory, visual, kinesthetic—embedding knowledge across diverse cognitive pathways. Incorporate active retrieval techniques, scenario-based questioning, and conceptual cross-linking to transform passive familiarity into functional mastery.
Iterative reinforcement extends beyond content acquisition into strategic refinement. Continuously evaluate temporal pacing, error patterns, and cognitive resilience, adjusting study intensity, modality, and scope as necessary. This cyclical approach transforms study into an adaptive ecosystem, responsive to both personal growth trajectories and the evolving complexity of material.
Interleaving and Spaced Repetition Techniques
To transcend rote memorization, interleaving and spaced repetition are indispensable cognitive strategies. Interleaving, the deliberate alternation between topics or question types, fosters adaptability and deepens conceptual connections. For example, toggling between cardiology, obstetrics, and psychiatric scenarios prevents compartmentalized thinking, promoting a fluid approach to multifaceted clinical problems.
Spaced repetition leverages the psychological spacing effect, reinforcing memory just as it begins to fade. Digital tools, flashcards, or self-designed question banks can orchestrate this rhythm. The temporal spacing ensures that information is not merely transiently stored but permanently integrated into long-term memory, enabling instant recall under the pressure of timed examinations.
Harnessing Pattern Recognition
Clinical pattern recognition is the silent architect of swift decision-making. By repeatedly exposing oneself to varied question structures and patient vignettes, the mind begins to intuitively identify hallmark signs and differential cues. Patterns emerge not only in disease presentation but also in recurring distractors, phrasing tendencies, and conceptual traps set by examiners.
Cultivating pattern recognition reduces cognitive load during actual exams, allowing faster prioritization of options and more confident selection. Integrating this with reflective analysis of errors creates a feedback loop that continually sharpens instinctual clinical judgment.
Cognitive Load Management
Excessive information can overwhelm even the most prepared aspirants. Cognitive load theory emphasizes the need to manage intrinsic, extraneous, and germane load during preparation. Intrinsic load arises from the complexity of the material itself, extraneous from poorly structured study methods, and germane from efforts that enhance schema construction.
Strategies to mitigate overload include chunking information, using mnemonics, diagrammatic representations, and concept maps. Transforming textual content into visual or symbolic schemas not only reduces cognitive strain but reinforces retention through dual coding mechanisms. When used deliberately, these strategies enable the mind to navigate complex clinical scenarios with elegance and precision.
Simulation-Based Immersive Learning
Beyond traditional mock exams, immersive simulation-based learning offers unparalleled experiential advantage. High-fidelity scenarios—ranging from simulated resuscitations to intricate post-operative care—allow aspirants to experience procedural and cognitive demands in real-time. These simulations nurture situational awareness, critical thinking, and rapid decision-making, all of which are vital for high-stakes examinations.
Post-simulation debriefing is as critical as the exercise itself. By dissecting decisions, exploring alternatives, and reviewing physiological responses, students solidify both procedural knowledge and cognitive reasoning. This bridge between theory and practice enhances the capacity to transfer skills from preparation to real-world contexts.
Emotional Regulation Under Exam Pressure
Examination anxiety can erode performance even in well-prepared candidates. Cultivating emotional regulation is thus a non-negotiable element of preparation. Techniques such as mindfulness, diaphragmatic breathing, and cognitive restructuring reduce physiological arousal, sharpen focus, and stabilize judgment.
Visualizing success in conjunction with rehearsal of complex scenarios enhances confidence. Recognize that stress is not inherently detrimental; moderate levels of arousal can enhance alertness. The key is harnessing this energy strategically, transforming potential anxiety into purposeful motivation that drives focused performance.
Strategic Prioritization and Time Allocation
Examinations with multi-topic, multi-step questions demand acute prioritization. Understanding which questions to tackle first, which require extended reasoning, and which can be addressed swiftly is crucial. Time management strategies include flagging complex questions for later review, allocating fixed intervals per section, and rehearsing timing during mock exams.
Effective prioritization is synergistic with reflective practice. Review sessions after each timed exercise should evaluate whether the chosen time allocations optimized both accuracy and efficiency. This iterative process sharpens temporal judgment and prevents the pitfalls of both procrastination and hasty, error-prone responses.
Advanced Error Analysis
Analyzing mistakes is more than noting what went wrong; it is an intricate dissection of cognitive pathways. Errors can be categorized into knowledge deficits, misinterpretation, distractor susceptibility, or lapses in procedural logic. Each category necessitates distinct remedial strategies.
For example, a misinterpretation of a clinical vignette may indicate the need to improve reading for nuance, whereas distractor susceptibility may reveal superficial memorization without deep conceptual understanding. Systematic classification transforms errors from demoralizing setbacks into precise opportunities for targeted cognitive refinement.
Integrating Multimodal Learning
Multimodal learning exploits the complementary strengths of auditory, visual, kinesthetic, and textual modalities. For nursing exam preparation, this could involve listening to expert discussions while simultaneously reviewing visual diagrams, or practicing procedural steps while verbally articulating underlying rationale.
This poly-sensory engagement strengthens neural pathways, increases retention, and enhances the ability to recall information under varying cognitive conditions. By merging modalities, learners not only encode knowledge more robustly but also build versatile retrieval strategies adaptable to diverse question structures.
Cultivating Cognitive Flexibility
Cognitive flexibility—the ability to shift perspectives, adapt reasoning, and integrate disparate information—is critical for unpredictable examination scenarios. Exposure to interdisciplinary questions, ethical dilemmas, and case studies that span multiple domains nurtures this mental agility.
Exercises that deliberately challenge assumptions, force alternative prioritizations, or present conflicting data sets enhance cognitive elasticity. Over time, this practice fosters a mindset capable of nuanced reasoning, rapid synthesis, and adaptive problem-solving—qualities that separate high-performing aspirants from the merely competent.
The Role of Meta-Learning
Meta-learning, or learning about learning, is an advanced strategy often overlooked. By systematically evaluating which study techniques yield the most retention, which questioning strategies produce deeper comprehension, and which time management methods optimize output, learners refine not only their knowledge but their approach to knowledge acquisition itself.
Maintaining a meta-learning journal allows for the documentation of strategy effectiveness, cognitive energy patterns, and adaptive modifications. This continuous cycle of evaluation, adjustment, and implementation creates a self-sustaining framework for increasingly efficient and effective exam preparation.
Harnessing Intrinsic Motivation
Sustaining high-intensity preparation requires more than discipline; it requires intrinsic motivation. Identifying personal drivers—such as professional aspirations, patient impact, or intellectual curiosity—infuses study sessions with purpose. Motivation anchored in personal values is more resilient than extrinsic incentives, fostering persistence in the face of setbacks and monotony.
Ritualizing study habits, setting micro-goals, and celebrating incremental progress transforms preparation into an engaging, self-reinforcing process. This not only enhances engagement but also deepens cognitive integration, as motivated learning is consistently associated with improved retention and problem-solving capacity.
Scenario-Based Critical Reasoning
Scenario-based reasoning is an advanced cognitive skill integral to nursing exams. It requires the simultaneous application of theoretical knowledge, clinical judgment, ethical considerations, and temporal prioritization. For example, evaluating a polytrauma patient while anticipating potential complications demands multi-layered cognitive orchestration.
Practice with diverse scenarios, followed by reflective debriefing, develops mental heuristics that streamline decision-making. Over time, the aspirant cultivates the ability to anticipate complications, sequence interventions optimally, and justify decisions with evidence-based reasoning—qualities that are directly transferrable to both exams and clinical practice.
Optimizing Retention Through Elaboration
Elaborative rehearsal is a potent strategy to fortify memory. Instead of merely reading or memorizing facts, learners create associations, analogies, and narratives that integrate new information into existing cognitive schemas.
For instance, linking pharmacological mechanisms to real-life patient outcomes or conceptualizing pathophysiological processes as dynamic, interactive systems enhances both understanding and recall. This narrative embedding transforms abstract content into meaningful constructs, ensuring that retention is durable and recall is contextually rich.
Advanced Critical Thinking in Dynamic Clinical Environments
Clinical environments are inherently dynamic, demanding nurses to continuously synthesize information, anticipate complications, and make judicious decisions. Advanced critical thinking transcends rote protocols and requires adaptive cognition, pattern recognition, and contextual awareness. Nurses must be able to navigate ambiguous situations where textbook solutions may not apply, especially in high-acuity care settings.
Cognitive flexibility allows practitioners to pivot strategies as new patient data emerges. For instance, a patient initially diagnosed with community-acquired pneumonia may develop acute kidney injury secondary to aggressive fluid resuscitation. Recognizing the evolving pathology, recalibrating interventions, and prioritizing renal preservation over routine pneumonia management exemplifies advanced reasoning.
Scenario-based exercises, incorporating multilayered complications, cultivate such thinking. Nurses can practice identifying early warning signs, integrating laboratory trends, and predicting potential deterioration. The capacity to anticipate “what-if” scenarios before they fully manifest is a hallmark of expert clinical judgment.
Managing Complex Patient Populations
Nurses frequently encounter patients with multifactorial health issues, necessitating sophisticated assessment and management skills. Polymorbid patients, geriatric populations, and immunocompromised individuals require individualized care plans that consider physiological, psychological, and sociocultural variables.
Polymorbidity amplifies the risk of cascading complications. A patient with congestive heart failure, diabetes mellitus, and chronic kidney disease exemplifies a clinical puzzle where fluid management, glycemic control, and renal preservation must be simultaneously balanced. Prioritization, vigilant monitoring, and rapid intervention are critical.
In geriatric care, subtle changes often herald significant pathology. Delirium may masquerade as depression, and minor electrolyte shifts can precipitate cardiac arrhythmias. Nurses must apply nuanced assessment techniques, integrating cognitive screening, mobility evaluations, and nutrition assessment to detect deviations from baseline.
Immunocompromised patients pose additional challenges, as classical signs of infection may be blunted. Nurses must maintain heightened vigilance, employ rigorous aseptic techniques, and understand pharmacological modifications to immunosuppressive regimens. Mastery of these complex scenarios demonstrates both clinical dexterity and intellectual acuity.
Interdisciplinary Collaboration and Synergistic Care
Optimal patient outcomes frequently hinge upon seamless interdisciplinary collaboration. Nurses operate as critical nodes within healthcare networks, synthesizing input from physicians, pharmacists, dietitians, physical therapists, and social workers. Effective communication, role clarity, and proactive coordination are essential competencies.
Case conferences and interprofessional rounds exemplify collaborative problem-solving. Presenting comprehensive patient assessments, highlighting subtle changes, and proposing evidence-based interventions foster trust and shared decision-making. For example, coordinating wound care for a diabetic patient may require negotiating with a podiatrist for offloading strategies, a nutritionist for glycemic optimization, and a physiotherapist for mobility support.
Interdisciplinary collaboration also mitigates cognitive biases. By engaging multiple perspectives, nurses refine clinical reasoning, verify assumptions, and identify overlooked complications. Mastery of these dynamics is critical for both patient safety and success in licensure examinations.
Nuanced Communication with Patients and Families
Communication in nursing extends beyond conveying information; it is a sophisticated interplay of empathy, clarity, and cultural sensitivity. Effective dialogue fosters patient adherence, enhances safety, and mitigates anxiety. Nurses must tailor their approach to individual literacy levels, emotional states, and cultural norms.
Active listening is central to nuanced communication. By discerning verbal and nonverbal cues, nurses uncover latent concerns and detect discrepancies between reported symptoms and clinical findings. For instance, a patient may underreport pain due to cultural stoicism, necessitating careful observation and validation.
Delivering complex information, such as explaining medication regimens or post-operative care, requires precision and tact. Analogies, visual aids, and iterative confirmation can enhance comprehension. When addressing families, nurses must balance honesty with reassurance, navigating emotionally charged situations while maintaining professional integrity.
Communication is also vital in high-stakes scenarios. Rapid handovers, escalation of deteriorating conditions, and documentation of informed consent all rely on clarity, brevity, and assertiveness. Developing these competencies through simulation and reflective practice strengthens professional confidence and exam readiness.
Cognitive Load Management in Critical Care
Critical care nursing demands the management of high cognitive load, where multiple simultaneous inputs must be processed and prioritized. Effective cognitive load management prevents errors, enhances situational awareness, and maintains decision-making accuracy under stress.
Strategies for managing cognitive load include mental rehearsal, checklists, and cognitive chunking. For instance, preparing for a cardiac arrest scenario involves mentally simulating airway management, defibrillation protocols, and pharmacological interventions simultaneously. Checklists provide cognitive scaffolding, reducing reliance on memory and minimizing omission errors.
Additionally, mindfulness techniques and structured debriefings support cognitive resilience. By reflecting on high-stakes experiences, nurses consolidate procedural memory, identify patterns, and develop adaptive strategies for future encounters. In licensure examinations, demonstrating an ability to handle layered complexity without cognitive overload signals advanced competency.
Integrating Evidence-Based Practice into Daily Nursing
Evidence-based practice (EBP) forms the bedrock of modern nursing, merging empirical research with clinical expertise and patient preferences. Nurses must critically appraise literature, assess applicability to their patient population, and implement interventions with documented efficacy.
Incorporating EBP enhances outcomes in diverse scenarios. For example, selecting the optimal dressing for a chronic wound requires understanding comparative studies on healing rates, infection prevention, and patient comfort. Similarly, antibiotic stewardship demands knowledge of local resistance patterns and evidence-based guidelines to avoid overuse or underdosing.
High-stakes exam scenarios often test the ability to apply EBP in situ. Nurses must evaluate emerging data, integrate institutional protocols, and make patient-centered recommendations rapidly. Mastery of this skill reflects intellectual rigor and practical acumen, bridging theory and bedside application.
Vigilance in Early Detection of Deterioration
The ability to detect early signs of clinical deterioration is a defining attribute of expert nurses. Subtle physiological changes, minor deviations in vital signs, or early laboratory anomalies often precede life-threatening events. Recognizing these harbingers enables timely intervention and prevents escalation.
Tools such as the Modified Early Warning Score (MEWS) or Rapid Response Team protocols provide structured frameworks, but seasoned nurses supplement these with intuitive pattern recognition. For example, subtle tachycardia combined with mild confusion in an elderly patient may indicate sepsis even before overt hypotension develops.
Simulation exercises and real-time scenario drills reinforce these competencies. Practicing escalation protocols, recognizing atypical presentations, and documenting observations precisely cultivates vigilance and rapid-response capability.
Managing Ethical and Legal Complexities
Ethical and legal complexity in nursing is multifaceted, encompassing patient rights, informed consent, confidentiality, and regulatory adherence. Nurses must navigate these dimensions without compromising care quality or professional integrity.
Situations often require balancing competing ethical principles. For instance, honoring a patient’s refusal of treatment may conflict with beneficence, particularly if refusal risks imminent deterioration. Knowledge of UAE-specific legal statutes and institutional policies provides a framework for ethical decision-making while safeguarding professional accountability.
Documenting ethical reasoning, patient preferences, and informed consent discussions is crucial. The ability to articulate rationale in both written and verbal formats ensures transparency, supports interdisciplinary collaboration, and demonstrates professional maturity during high-stakes examinations.
Leveraging Technology for Enhanced Nursing Practice
Modern nursing is increasingly intertwined with technological innovations that enhance patient monitoring, data synthesis, and procedural accuracy. Electronic health records, smart infusion pumps, telemedicine platforms, and clinical decision support systems empower nurses to deliver precision care.
Technological fluency allows nurses to detect anomalies, anticipate complications, and streamline documentation. For example, integrating continuous glucose monitoring with automated insulin delivery systems reduces the risk of hypo- or hyperglycemic events. Similarly, remote monitoring tools facilitate timely intervention for patients in critical care or post-discharge settings.
Examination scenarios often assess the ability to interpret digital data, reconcile discrepancies, and make evidence-informed decisions rapidly. Proficiency in leveraging technology not only enhances patient safety but also reflects adaptability and modern clinical competence.
Precision in Clinical Reasoning
Precision in clinical reasoning is the fulcrum upon which HAAD-RN success pivots. Aspirants must cultivate the ability to discriminate subtle diagnostic cues from misleading data. This requires a meticulous approach: deconstructing patient histories, parsing laboratory indices, and correlating pathophysiological sequences with clinical manifestations. Engage in iterative exercises that challenge the identification of atypical presentations—such as silent myocardial infarctions in diabetic patients or occult sepsis in immunocompromised individuals. By embedding such analytical rigor into daily study routines, aspirants develop an intellectual acuity that transcends formulaic responses, enabling rapid, nuanced judgments under temporal duress.
The Semantics of Medical Language
Mastery of medical lexicon enhances interpretive precision and cognitive efficiency. HAAD-RN aspirants benefit from developing an intricate understanding of medical terminology, including rare eponyms, archaic nomenclature, and pathognomonic descriptors. For instance, grasping distinctions between ‘tachypnea’ and ‘hyperpnea’ or differentiating ‘pleuritic’ from ‘non-pleuritic’ pain can decisively influence answer accuracy. Employ semantic mapping techniques, linking terminology to underlying pathophysiology, clinical implications, and procedural interventions. This triadic linkage ensures that vocabulary acquisition is functionally integrated, rather than superficially memorized, thereby amplifying comprehension and recall.
Cognitive Resilience Through Error Analysis
Error analysis is a formidable tool in reinforcing cognitive resilience. Maintain a comprehensive repository of mistakes encountered during practice questions, categorizing them by content area, question type, and reasoning flaw. Examine each error meticulously: distinguish between knowledge gaps, misinterpretations, and lapses in temporal management. By transforming errors into actionable learning modules, aspirants cultivate an adaptive mindset, whereby missteps become catalysts for intellectual growth rather than sources of discouragement. This reflective discipline fosters an enduring capacity to navigate complex clinical conundrums with confidence.
Strategic Integration of Pharmacology
Pharmacology, a domain often regarded as daunting, can be rendered approachable through strategic integration. Organize medications by mechanism of action, adverse effect profiles, and critical nursing considerations. Construct comparative matrices linking therapeutic classes with pathophysiological targets, reinforcing conceptual associations rather than rote memorization. Engage in scenario-based exercises: for example, determine the optimal pharmacologic intervention for a hypertensive patient with renal impairment, considering drug metabolism, contraindications, and monitoring parameters. This applied approach consolidates knowledge into functional decision-making capabilities, vital for HAAD-RN assessments.
Situational Judgment Acumen
Situational judgment questions (SJQs) assess ethical reasoning, prioritization, and patient-centered decision-making. Developing acumen in this realm requires deliberate exposure to clinical dilemmas, ranging from triage in emergency scenarios to conflict resolution in multidisciplinary teams. Employ reflective exercises to evaluate decision pathways: anticipate potential consequences, weigh risk-benefit paradigms, and articulate rationales with ethical clarity. By internalizing principles of professional conduct, patient safety, and empathetic communication, aspirants cultivate a decision-making framework aligned with real-world nursing praxis and HAAD-RN evaluative criteria.
Cognitive Ergonomics in Study Design
Cognitive ergonomics, the optimization of study environments to align with neural processing efficiency, significantly impacts knowledge retention. Design study spaces that minimize extraneous stimuli, regulate lighting to enhance visual acuity, and employ auditory conditions conducive to focus, such as low-level ambient sound. Incorporate ergonomic tools: adjustable seating, supportive posture, and accessible reference materials. By harmonizing physical, sensory, and cognitive parameters, aspirants reduce mental fatigue, augment attentional endurance, and maximize the efficacy of intensive preparation sessions.
Advanced Pathophysiological Correlation
Advanced comprehension of pathophysiological mechanisms underlies successful clinical reasoning. Aspirants should endeavor to connect cellular-level processes to systemic manifestations. For instance, consider the cascade from endothelial dysfunction to atherosclerotic plaque formation, culminating in myocardial infarction, and correlate it with emergent nursing interventions. Similarly, tracing the interplay between cytokine dysregulation and septic shock enables precise anticipatory care. Construct detailed causal diagrams to visually map these relationships, reinforcing both memory retention and the ability to apply theoretical knowledge to dynamic clinical scenarios.
Temporal Adaptation and Exam Simulation
Temporal adaptation, the conditioning of cognitive faculties to high-stakes temporal constraints, is indispensable. Integrate progressive simulation exercises mimicking HAAD-RN time pressure: allocate strict intervals for discrete question blocks, progressively reducing buffer time as proficiency develops. Track response latency and accuracy meticulously, analyzing patterns of temporal inefficiency. This habituation enhances decision-making velocity without sacrificing analytical depth, ensuring readiness to navigate the dual demands of speed and precision intrinsic to examination conditions.
Interpersonal Cognitive Exchange
Engaging in structured discourse with peers catalyzes intellectual growth. Collaborative study groups, case-based discussions, and mentorship interactions provide alternative cognitive pathways, revealing nuanced approaches to clinical interpretation. Exposure to diverse reasoning methodologies mitigates cognitive rigidity and fosters adaptive flexibility. Moreover, articulating one’s thought process enhances metacognitive awareness, revealing latent misconceptions and consolidating conceptual mastery. Strategic dialogue thus functions as both a cognitive accelerator and a reflective amplifier.
Integrative Multimodal Review Techniques
To sustain high-level retention, integrate multimodal review techniques that interweave reading, auditory processing, and experiential application. For instance, after reading about renal pathophysiology, summarize the key points aloud, create illustrative diagrams, and apply the knowledge through hypothetical patient scenarios. This reinforcement through multiple sensory and cognitive channels solidifies neural encoding, facilitating rapid retrieval during examination conditions. Iterative application across subject domains ensures a holistic, interconnected knowledge framework rather than isolated factual recall.
Neurocognitive Priming Before Examination
Neurocognitive priming can optimize examination performance. Engage in preparatory routines that activate memory recall, enhance focus, and modulate emotional state. Techniques may include guided visualization of successfully navigating challenging questions, recapitulation of high-yield content, and short, focused bursts of cognitive drills. Combined with physical priming, such as controlled breathing and light aerobic activity, these strategies heighten alertness, reduce anxiety, and foster a neurochemically favorable environment for sustained cognitive performance.
Ethical Foresight in Clinical Decision-Making
Ethical foresight is a crucial, yet often underemphasized, facet of HAAD-RN preparation. Anticipate scenarios where moral judgment intersects with clinical imperatives, such as resource allocation in critical care or managing informed consent dilemmas. Analyze case studies through ethical frameworks—principlism, utilitarianism, and deontological reasoning—to discern appropriate courses of action. This ethical literacy ensures that aspirants are not merely technically proficient but also capable of navigating the moral complexities intrinsic to modern nursing practice.
Adaptive Learning Algorithms and Technology Utilization
Harnessing technological platforms that incorporate adaptive learning algorithms can significantly amplify preparation efficiency. These systems analyze performance trends, identify knowledge gaps, and dynamically adjust content difficulty. Engage with interactive modules, question banks, and virtual simulations tailored to the HAAD-RN framework. By leveraging data-driven insights, aspirants optimize study allocation, focus on high-impact areas, and progressively elevate cognitive competence in a targeted, evidence-based manner.
Resilience Through Iterative Challenge
True resilience emerges from the iterative confrontation of progressively complex challenges. Structure study sequences to escalate in difficulty, incorporating multifactorial scenarios, overlapping disease processes, and atypical presentations. Reflect upon each session, extracting lessons, recalibrating strategies, and reinforcing cognitive scaffolding. Over time, this iterative exposure fosters not only intellectual dexterity but also psychological fortitude, preparing aspirants to confront the unpredictable and high-pressure milieu of the HAAD-RN examination with composure and confidence.
Embracing the Nuances of UAE Healthcare Landscape
The HAAD-RN exam mandates a profound understanding of the regional healthcare ecosystem, which is characterized by a confluence of advanced medical infrastructure and intricate sociocultural dynamics. Nurses must possess both epidemiological literacy and cultural sagacity to deliver efficacious, patient-centered care. Knowledge of disease prevalence patterns, such as the heightened incidence of diabetes mellitus, cardiovascular pathology, and genetic hemoglobinopathies in the UAE, informs both clinical reasoning and preventive strategies.
Cultural competence is indispensable. The UAE hosts a heterogeneous population encompassing Emirati nationals, expatriates from diverse geographies, and transient labor communities. This multiplicity necessitates the ability to navigate linguistic, religious, and familial paradigms that influence healthcare perceptions, consent, and adherence. For instance, understanding the pivotal role of familial consultation in decision-making can enhance communication efficacy, reduce patient anxiety, and improve clinical outcomes. A nuanced approach to culturally sensitive interventions demonstrates professional maturity and elevates the quality of care.
Patient Education Strategies and Communication Dexterity
Patient education transcends mere dissemination of information; it embodies pedagogical acumen tailored to the patient’s cognitive, linguistic, and cultural context. Effective nurses in the UAE integrate health literacy assessment into practice, recognizing the variability in comprehension and receptivity across age, education, and cultural backgrounds. For example, explaining diabetic self-management to a middle-aged Emirati patient requires different linguistic phrasing and culturally relevant analogies compared to expatriate patients with divergent health paradigms.
Communication dexterity is closely allied with ethical competency. Nurses must employ therapeutic communication strategies, including reflective listening, motivational interviewing, and teach-back methods. These techniques ensure comprehension, adherence, and patient empowerment, which are vital components assessed in situational judgment questions. Moreover, nurses are expected to document patient interactions with precision, reflecting adherence to Ministry of Health protocols and electronic medical record systems.
Strategic Study Planning for Cognitive Optimization
A structured study plan functions as the scaffolding upon which comprehensive exam preparedness is constructed. Initial diagnostic assessments, such as practice tests and topic-wise self-evaluation, identify areas of scholastic vulnerability and strength. High-yield domains, including pharmacology, adult medical-surgical nursing, and emergency care, demand augmented study time. Conversely, lower-yield yet indispensable areas, such as neonatal and psychiatric care, should not be neglected, but rather reinforced through selective review and applied practice.
Temporal structuring is paramount. Dividing study periods into focused intervals interspersed with restorative breaks enhances memory consolidation and mitigates cognitive fatigue. Employing the Pomodoro technique or time-blocked sessions can optimize attention span and knowledge retention. Integrating a hybrid approach of reading, audiovisual learning, simulation, and group discussion fosters multidimensional engagement, reinforcing both declarative and procedural knowledge.
Integrating Simulation-Based and Case-Oriented Learning
Simulation-based learning functions as a crucible for honing technical and cognitive skills concurrently. High-fidelity simulations expose candidates to realistic patient scenarios, permitting experiential learning without compromising patient safety. Critical interventions, such as managing anaphylactic shock or ventilator-associated complications, can be rehearsed repetitively until procedural precision and clinical reasoning become second nature.
Case-oriented learning complements simulations by cultivating analytical rigor and pattern recognition. Systematic dissection of case studies—evaluating history, physical examination, laboratory findings, and ethical considerations—mirrors the multifaceted complexity of HAAD-RN questions. Peer discussions and debriefing sessions enhance reflective thinking, allowing candidates to recognize cognitive biases, anticipate complications, and refine prioritization strategies.
Advanced Pharmacologic Cognition
Pharmacologic mastery transcends memorization of drug names and dosages; it encompasses understanding mechanisms of action, pharmacodynamics, pharmacokinetics, adverse effect spectra, and contraindications. HAAD-RN aspirants must adeptly navigate polypharmacy scenarios, anticipate drug-drug interactions, and tailor medication regimens based on patient-specific factors such as age, comorbidities, and organ function.
Integration of pharmacologic knowledge with clinical scenarios is crucial. For instance, selecting an appropriate antihypertensive for a patient with concurrent renal insufficiency requires simultaneous consideration of drug clearance, hemodynamic effect, and potential for adverse reactions. Case-based questions often simulate such scenarios, challenging candidates to apply pharmacologic principles in dynamic clinical contexts rather than relying on rote recall.
Navigating Complex Ethical Dilemmas
Ethical challenges in the UAE healthcare system are frequently nuanced by sociocultural and legal considerations. Nurses may encounter conflicts between patient autonomy and familial authority, dilemmas surrounding organ donation, or questions of resource allocation in high-demand critical care environments. Mastery of principled ethical frameworks, including utilitarianism, deontology, and principlism, equips candidates to navigate these scenarios with intellectual rigor and moral clarity.
Reflective exercises and ethical case reviews augment this preparation. Candidates should practice articulating rationale for decisions, balancing beneficence and non-maleficence while remaining cognizant of cultural sensitivities. Such preparation enhances not only examination performance but also real-world professional practice, fostering resilience in ethically charged environments.
Mastering Situational Judgment and Prioritization
Situational judgment questions constitute a significant proportion of the HAAD-RN exam, assessing both cognitive and ethical acumen. Success in these questions hinges on prioritization skills, rapid assessment of clinical urgency, and judicious application of nursing interventions. Candidates must discern between emergent and non-emergent conditions, allocate resources effectively, and anticipate the trajectory of patient deterioration.
Developing a systematic approach to prioritization is invaluable. Techniques such as the ABCDE framework (Airway, Breathing, Circulation, Disability, Exposure) or Maslow’s hierarchy of patient needs provide structured heuristics for decision-making under pressure. Iterative practice with simulated scenarios cultivates reflexive application of these principles, ensuring fluid integration during examination.
Leveraging Cognitive Techniques for Retention and Recall
Advanced cognitive strategies enhance long-term retention and retrieval under examination stress. Techniques such as spaced repetition, mind mapping, and dual-coding integrate visual and semantic processing to solidify memory traces. Elaborative interrogation, which involves probing the rationale behind clinical interventions, reinforces conceptual understanding and facilitates application in novel scenarios.
Mindfulness and metacognitive reflection further optimize cognitive performance. By cultivating awareness of mental fatigue, cognitive biases, and emotional responses to complex scenarios, candidates can modulate stress, sustain attention, and enhance reasoning efficiency. These strategies synergize with structured study plans to maximize exam preparedness.
Exam-Day Psychology and Performance Optimization
The psychological milieu on exam day significantly impacts performance. Candidates must cultivate equanimity, managing anticipatory anxiety and cognitive overload. Techniques such as controlled breathing, progressive muscle relaxation, and visualization of successful scenario resolution can attenuate stress responses. Maintaining a steady pace, judicious time allocation, and strategic question triage are critical to optimizing scoring potential.
Meticulous logistical preparation also enhances confidence. Familiarity with testing platforms, procedural protocols, and timing sequences reduces extraneous cognitive load. By entering the examination environment with preparedness both cognitive and logistical, candidates position themselves to demonstrate their full spectrum of competencies effectively.
Conclusion
Preparing for the HAAD-RN exam is more than memorizing facts; it is a journey of cultivating knowledge, clinical judgment, and professional resilience. Success hinges on understanding the exam structure, mastering nursing competencies, and practicing strategic decision-making under realistic conditions. Through structured study plans, active recall, practice questions, and simulated scenarios, aspirants can transform theoretical knowledge into confident, adaptable clinical reasoning.
Equally important is nurturing mental clarity, managing stress, and building time management skills. The ability to prioritize, reflect, and apply knowledge in practical, culturally sensitive ways not only ensures exam success but also fosters excellence in real-world nursing practice. Post-exam, continuous professional development, evidence-based practice, and engagement with the broader healthcare community sustain growth, competence, and professional fulfillment.
Ultimately, the HAAD-RN exam is not just a test of memory; it is a celebration of preparation, critical thinking, and dedication to patient care. By approaching it with a holistic, disciplined, and reflective mindset, nurses not only achieve licensure but also lay a solid foundation for a thriving, impactful career in the UAE healthcare system. Success is the culmination of preparation, perseverance, and a commitment to lifelong learning.