Product Screenshots
Frequently Asked Questions
How does your testing engine works?
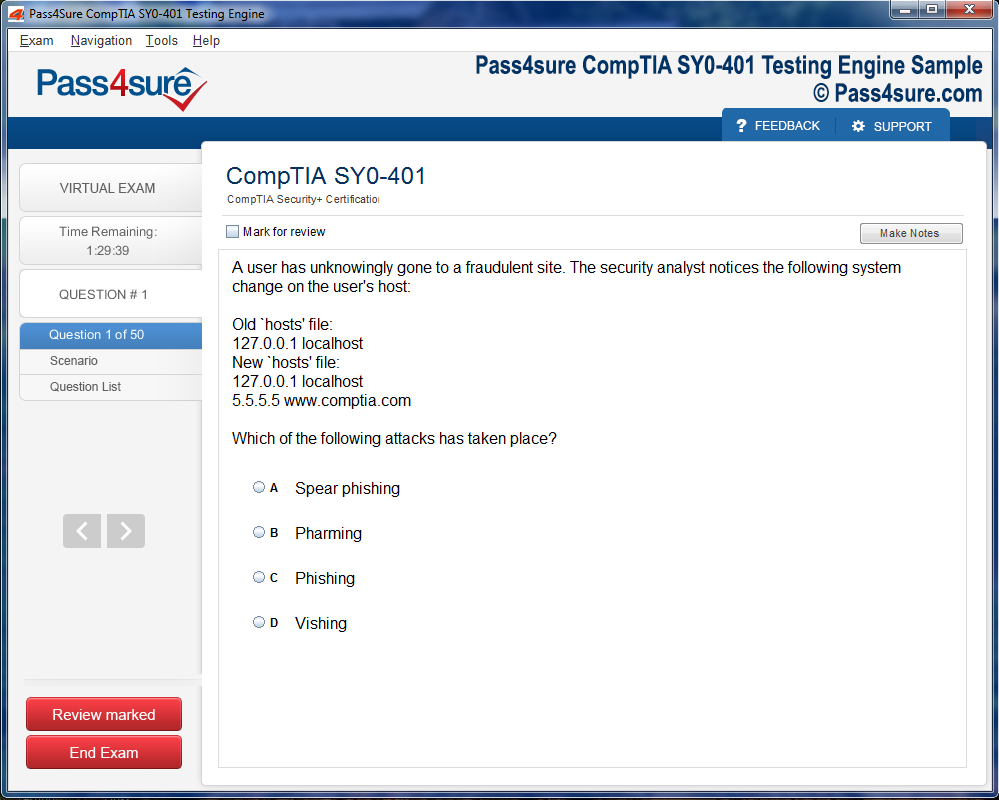
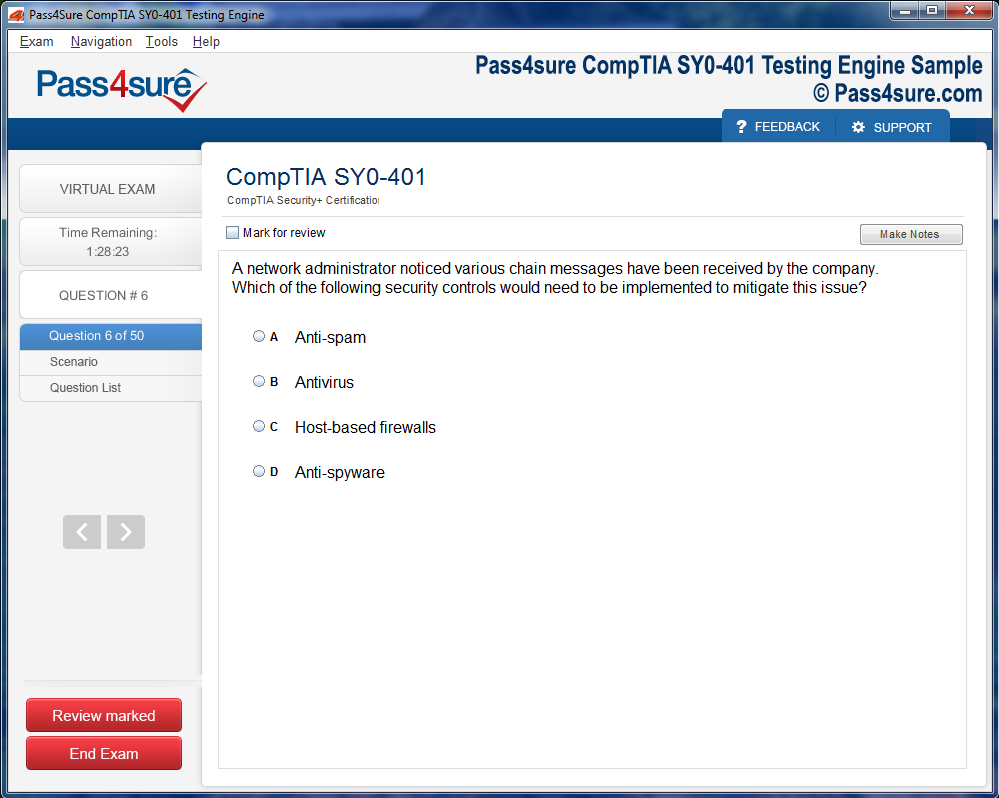
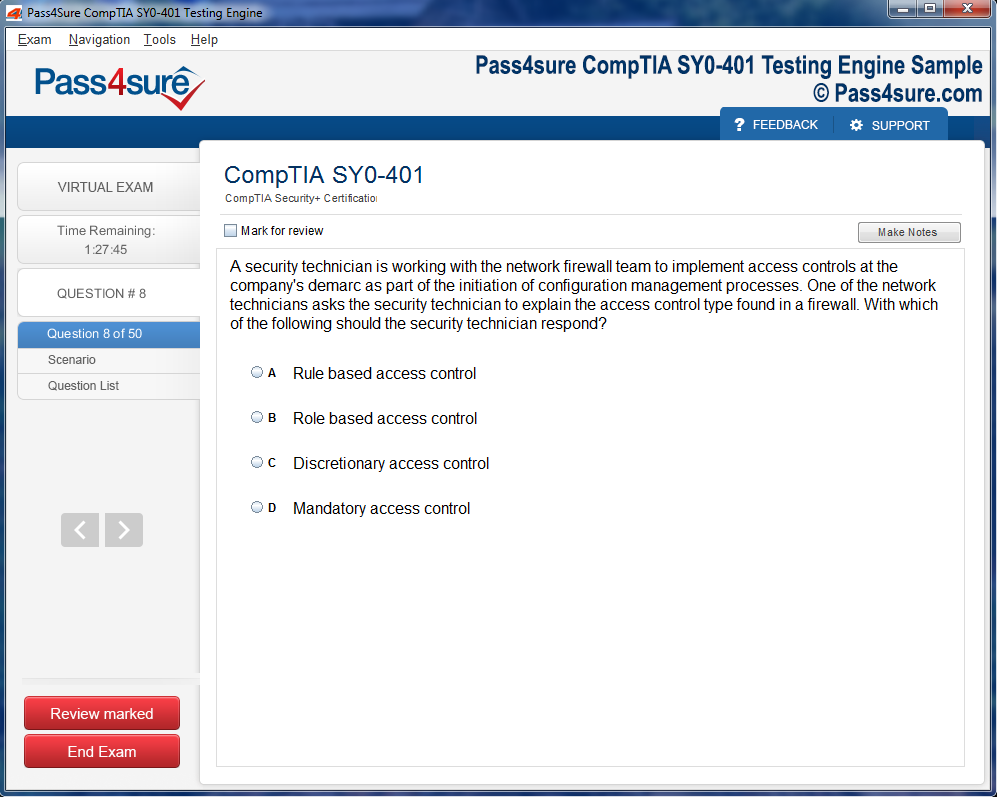
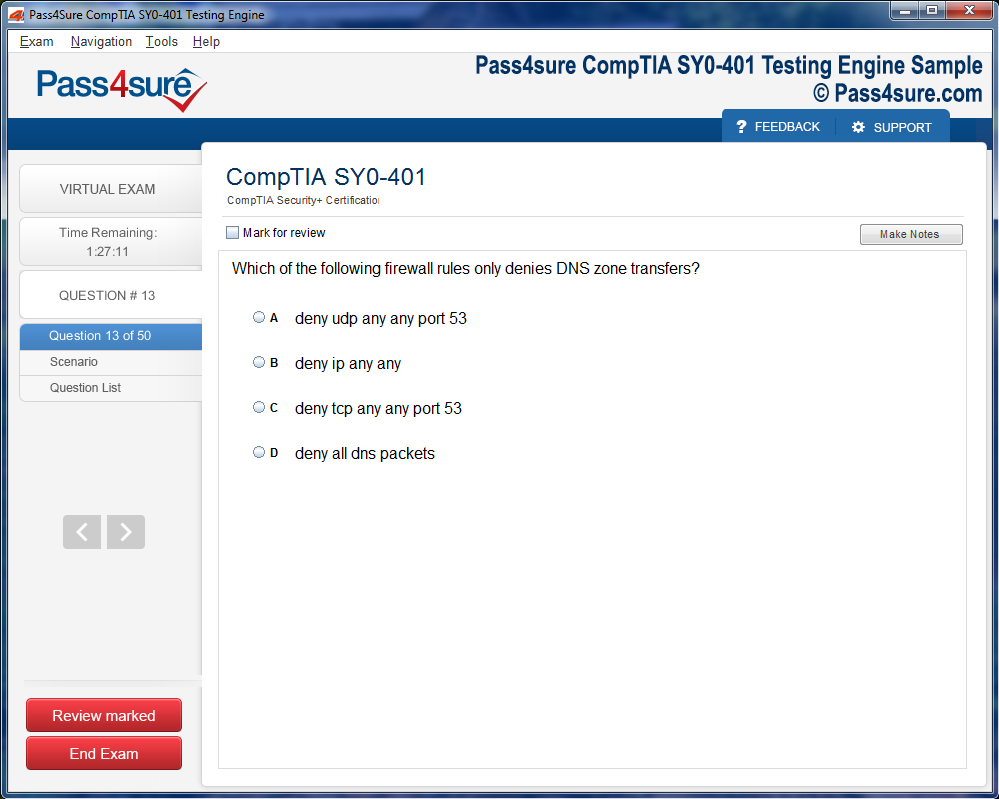
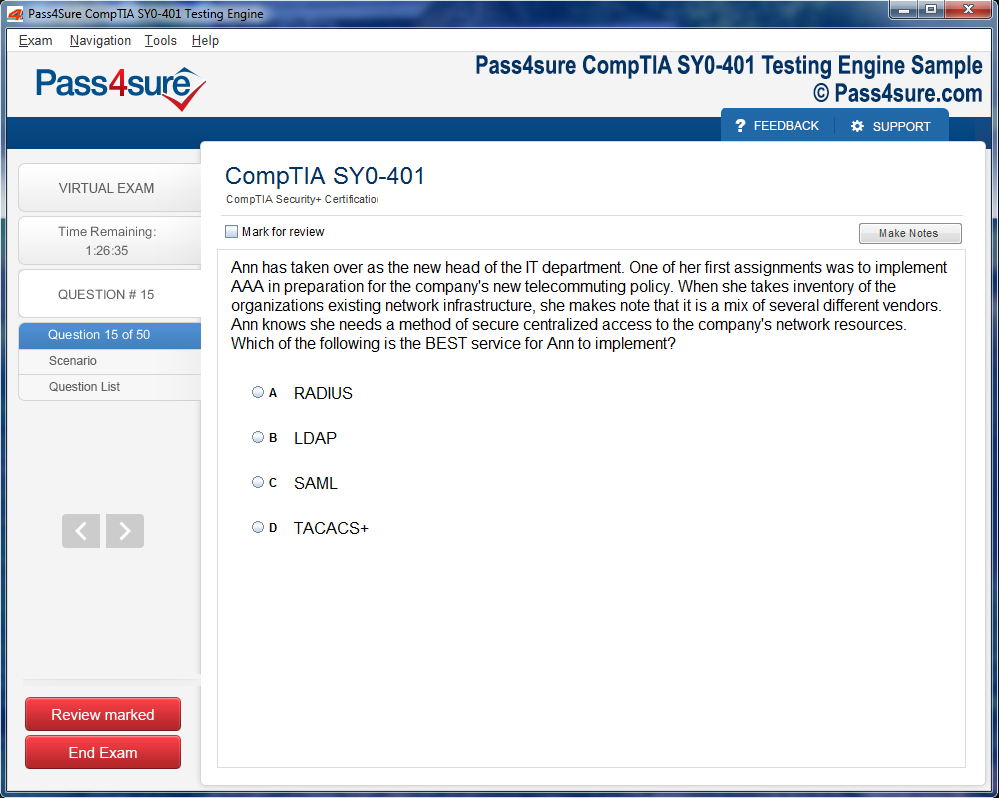
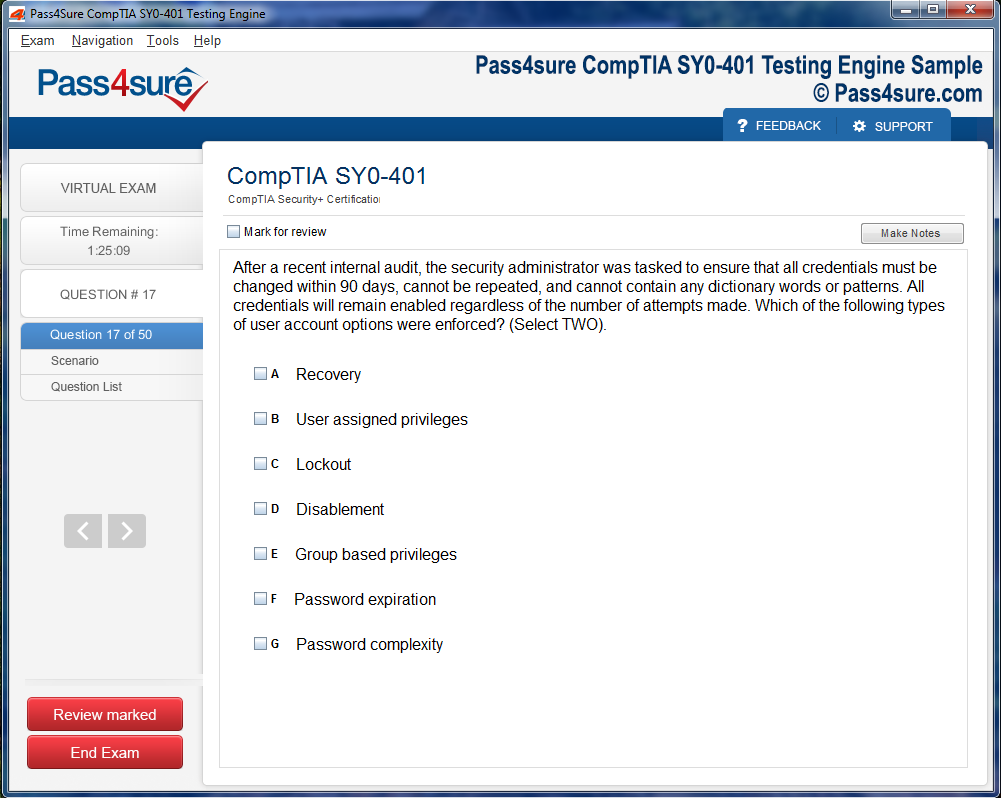
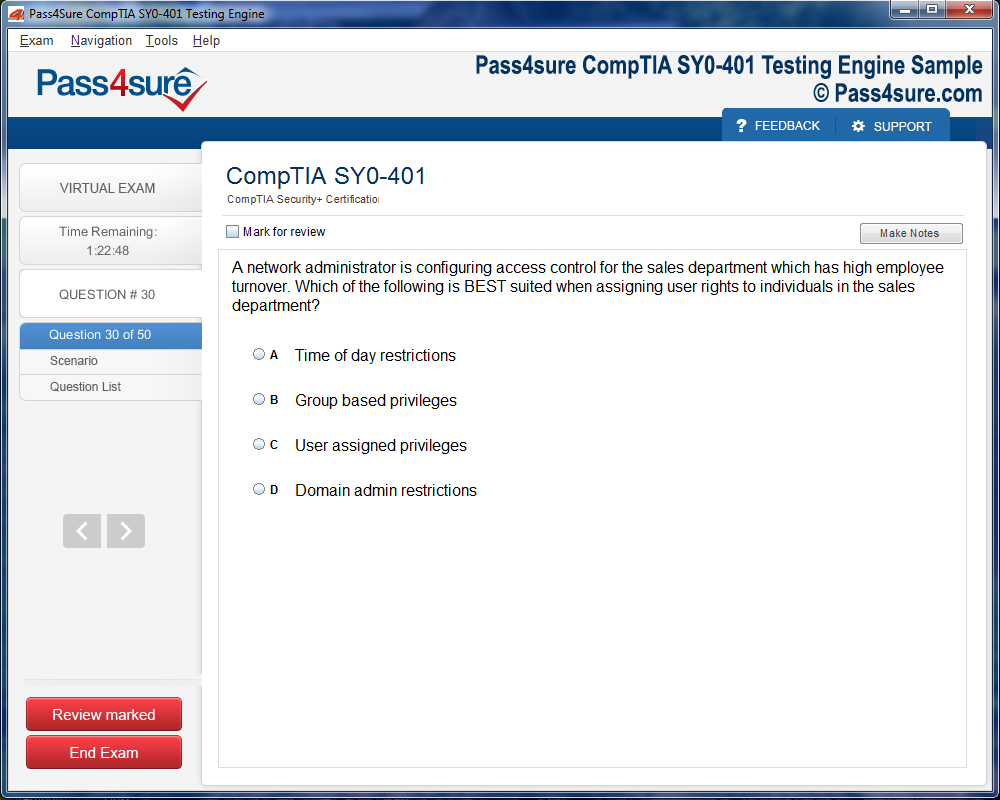
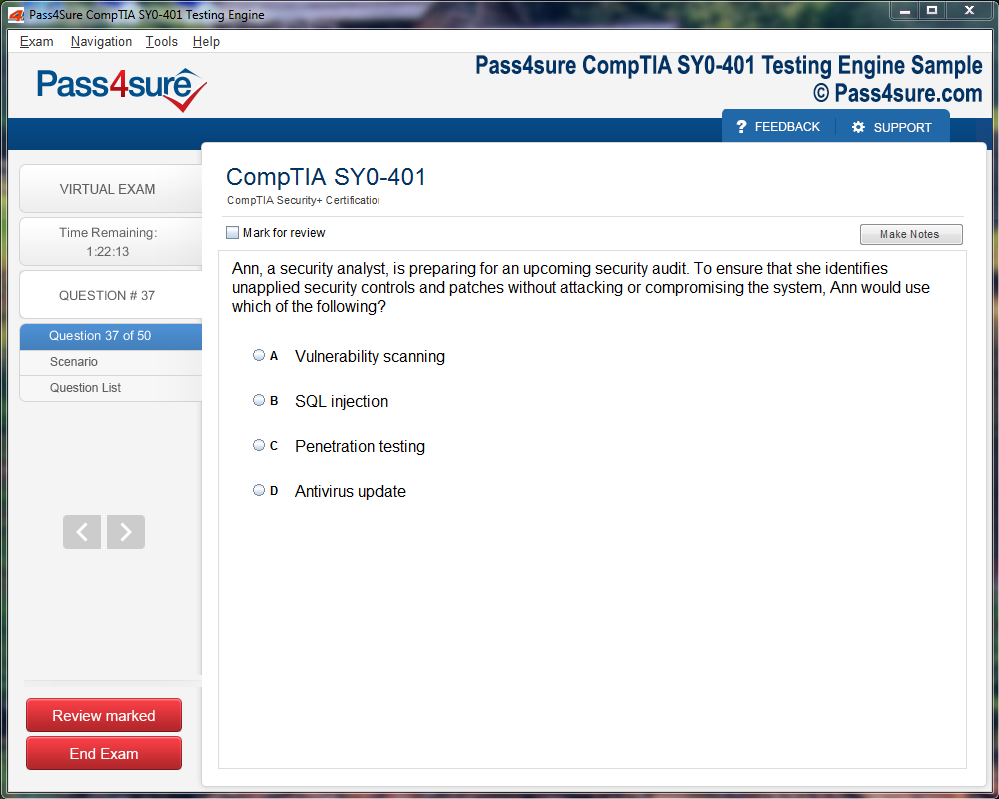
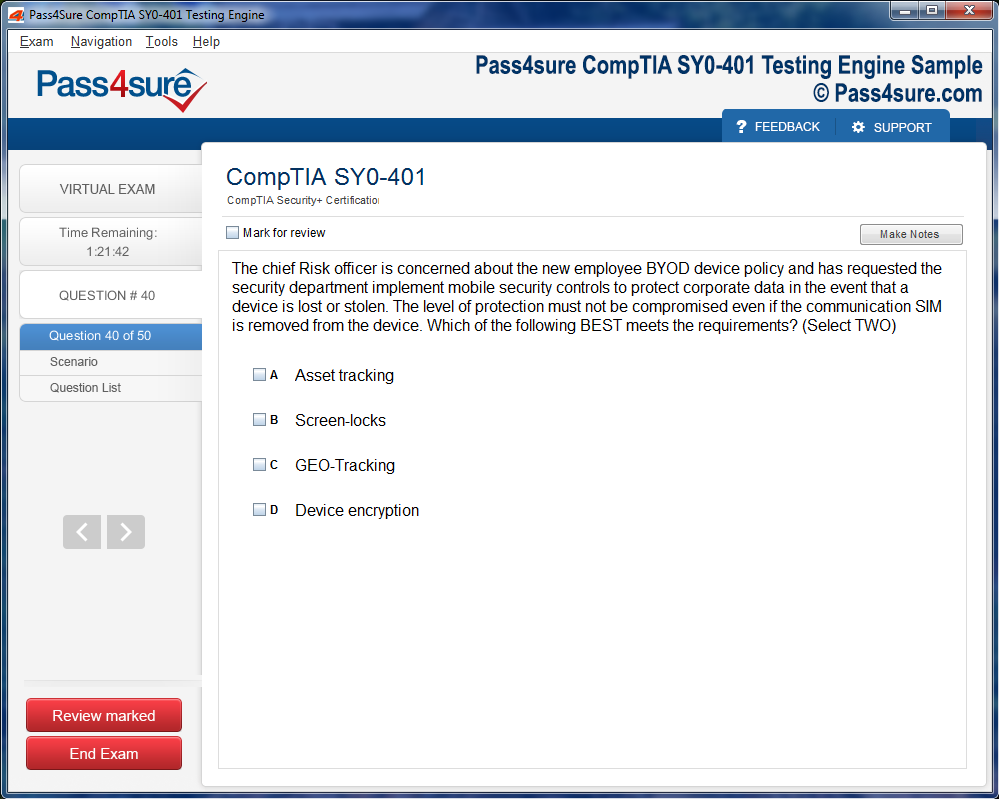
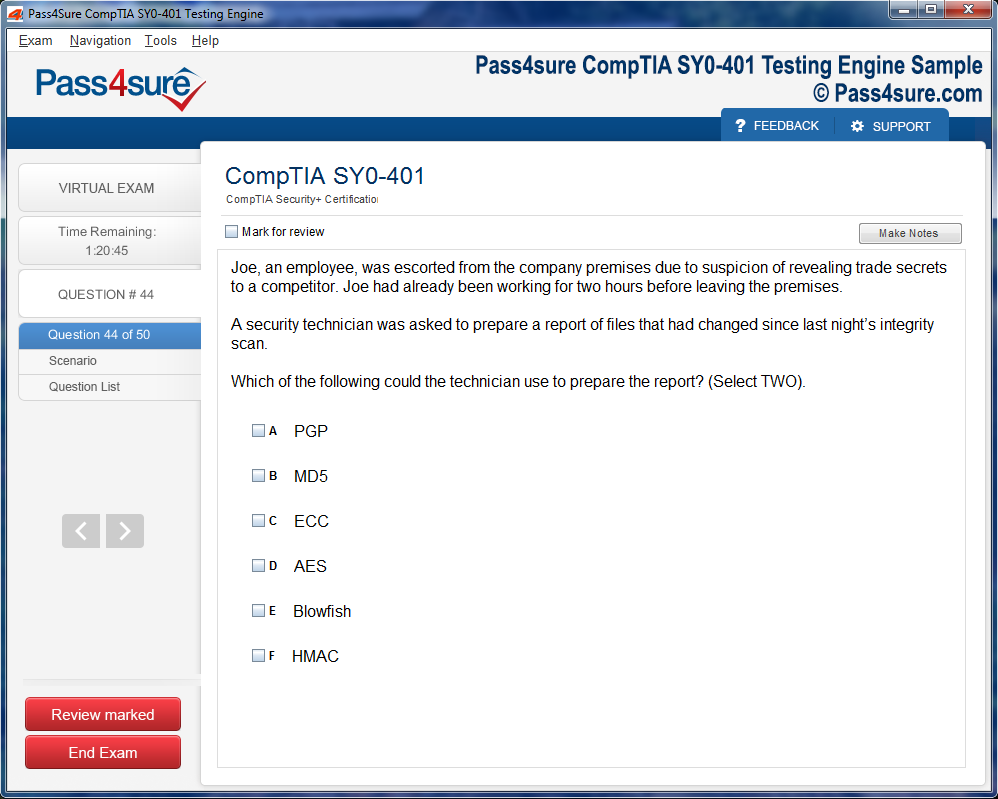
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations.
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.
Master the CPB Exam Essential Study Tips and Tricks
It starts with eligibility, a threshold designed to ensure that candidates arrive equipped with both theoretical grounding and practical familiarity. Unlike some certifications that demand years of prior experience, the CPB exam invites a broader range of aspirants—those with formal training, recent graduates from billing programs, and individuals transitioning into healthcare finance from related fields. The openness is intentional, for the billing profession thrives on diversity of perspective, analytical strength, and adaptability.
However, eligibility does not imply simplicity. Even if professional experience is not mandated, successful candidates often carry some exposure to medical environments, insurance operations, or revenue cycle tasks. This exposure shapes intuition, the ability to recognize nuances in claims, and the confidence to navigate the labyrinth of insurance guidelines. In many ways, the prerequisites are less about strict academic mandates and more about readiness—a combination of curiosity, discipline, and willingness to wrestle with intricate financial narratives that underpin healthcare delivery.
Registration Process and Exam Logistics
Embarking on the CPB journey requires not only preparation of the mind but also careful attention to administrative detail. Registration is straightforward yet unforgiving if overlooked. Candidates select their exam date and location, balancing personal readiness with the availability of testing centers. Some pursue the exam online with strict proctoring environments, while others prefer the tactile familiarity of in-person testing halls. Regardless of the mode, the principles of security and fairness remain unwavering, ensuring that every credential earned carries identical weight.
Scheduling is only one facet. Candidates must also ensure that identification, fee payment, and documentation align precisely with stated requirements. This is where the professionalism expected of billers first manifests—through meticulous adherence to procedural details. Just as an incomplete claim can delay reimbursement, an incomplete registration can obstruct entry into the exam. The very process foreshadows the discipline demanded in the profession itself.
The Anatomy of the CPB Exam
The architecture of the CPB exam is as deliberate as a surgeon’s incision. Each question is sculpted to reflect practical dilemmas: deciphering payer contracts, identifying fraudulent patterns, navigating the nuances of Medicare, or aligning clinical notes with billing codes. This is not a theoretical trial but a mirror of daily reality in billing offices nationwide.
Time management becomes the silent adversary. Five hours may appear generous at the outset, yet as candidates wade through two hundred questions, the minutes evaporate. The exam measures not just knowledge, but endurance, focus, and the ability to sustain accuracy under pressure. For this reason, preparation is not only intellectual but also psychological, training the candidate to pace themselves, manage fatigue, and maintain clarity until the final minute.
Core Domains of Knowledge Assessed
To grasp the full scope of the CPB exam, one must dissect the domains of knowledge it evaluates. Insurance claims processing forms the backbone, requiring mastery of submission rules, payer requirements, and rejection protocols. Compliance is another pillar, demanding an unflinching awareness of federal guidelines, fraud detection, and the ethical standards that govern billing.
Coding integration is equally critical, even though the exam is billing-focused. Billers must harmonize procedural and diagnostic codes, ensuring that claims not only represent services truthfully but also meet payer expectations. Additional domains stretch into patient billing, collection procedures, and appeal management. The exam’s breadth reflects the profession’s reality: billers are not mere form-fillers but strategic custodians of financial accuracy, compliance, and patient trust.
Preparation Strategies That Yield Mastery
Preparation for the CPB exam resembles training for a marathon rather than a sprint. Cramming may deliver short-lived recall, but it rarely produces the durable understanding required to thrive. Instead, successful candidates cultivate a layered strategy: structured study schedules, consistent practice tests, and immersion in real-world scenarios.
Textual study is crucial, but so is experiential learning. Reviewing sample claims, practicing denial management, or shadowing billing professionals creates a tactile connection to abstract concepts. Many candidates also simulate exam conditions—timed practice sessions that mimic the five-hour gauntlet, conditioning the mind to think sharply even as exhaustion encroaches.
Discipline is paired with adaptability. Billing rules evolve, payer policies shift, and compliance requirements expand. Thus, studying is not simply memorization but the cultivation of a mindset prepared for perpetual learning. This mindset becomes a professional habit long after the exam ends.
Psychological Readiness and Exam-Day Composure
Beyond knowledge lies composure. Anxiety has derailed countless skilled candidates, not for lack of understanding but for loss of calm. Preparing psychologically is as vital as academic study. Techniques such as paced breathing, structured breaks during the exam, and mindful refocusing can preserve mental stamina.
Exam-day rituals also matter. Arriving early, verifying documentation, and avoiding last-minute cramming contribute to confidence. The CPB exam is less a battle to be conquered and more a proving ground where preparation meets resilience. Success often belongs not to the most brilliant, but to the most balanced—those who can summon clarity under pressure.
The Professional Impact of Certification
Earning the CPB credential is transformative. It is not merely an additional line on a résumé but a recalibration of professional identity. Certified billers occupy a tier of recognition that sets them apart in hiring pools, granting them access to positions with higher responsibility, autonomy, and compensation. Employers view the credential as assurance of competence, diligence, and commitment to ethical billing.
The impact extends beyond personal advancement. Certified billers elevate entire organizations, reducing claim denials, ensuring regulatory compliance, and securing revenue streams that sustain patient care. The credential becomes a badge not only of knowledge but of reliability, symbolizing an individual’s capacity to safeguard financial health in an industry where errors can mean lost millions or legal jeopardy.
The Broader Value of the CPB Community
Certification is not an endpoint but an induction into a professional community. CPBs across the country form a network bound by shared expertise and shared challenges. Through conferences, forums, and continuing education, this community exchanges insights on emerging payer policies, evolving compliance requirements, and strategies to streamline revenue cycles.
Belonging to this network provides more than intellectual enrichment; it fosters resilience. Billing professionals often navigate stressful terrain, where denials, audits, and regulatory scrutiny create constant pressure. Knowing one is part of a larger fellowship of experts transforms isolation into collaboration and challenges into shared problem-solving.
The Ethical Imperative in Billing
At its heart, billing is not just a financial transaction—it is an ethical act. Every claim represents a patient encounter, a human story translated into codes and charges. The CPB credential carries with it the implicit responsibility to honor this story with accuracy and integrity. Fraudulent practices, whether intentional or negligent, compromise not only finances but also trust in healthcare itself.
Certified billers, therefore, embody an ethical imperative. They are guardians of transparency, ensuring that patients are billed fairly, providers are reimbursed justly, and systems remain compliant with the law. This ethical backbone elevates the profession beyond clerical tasks into a vocation grounded in accountability.
Lifelong Learning and Continuing Education
Certification is not static. Healthcare finance evolves ceaselessly, and with it, the responsibilities of the CPB. Continuing education ensures that certified professionals remain agile, capable of adapting to new billing software, emerging compliance mandates, and shifting payer landscapes.
Workshops, webinars, and specialized courses become essential tools, keeping billers attuned to the rhythm of industry change. Far from being a burden, this requirement for ongoing learning nurtures a professional culture of growth. CPBs become lifelong learners, embodying adaptability in a sector where stagnation equates to obsolescence.
The CPB as a Beacon of Precision and Integrity
The role of the Certified Professional Biller is often unseen by patients yet indispensable to their care. By transforming complex documentation into accurate claims, CPBs ensure that healthcare institutions remain financially viable and legally compliant. Their certification, validated through the rigor of the CPB exam, symbolizes more than academic achievement—it symbolizes trust, responsibility, and resilience.
The exam itself is a crucible, demanding not only technical mastery but psychological endurance. Those who emerge successful do so as stewards of accuracy, ethics, and financial stewardship. They step into a profession that, though invisible to many, holds immense power over the survival of healthcare delivery systems.
Ultimately, the CPB credential is not about passing a test; it is about embracing a calling. It is about carrying the weight of precision where imprecision is costly, and sustaining the heartbeat of healthcare institutions by ensuring that resources flow as they should. In this sense, the Certified Professional Biller is not just a participant in healthcare finance but a custodian of its integrity, a role whose importance cannot be overstated.
Eligibility and Registration for the CPB Exam
The pursuit of the Certified Professional Biller (CPB) credential begins not with the test itself, but with the gateway of eligibility. Unlike many professional certifications that place steep academic prerequisites as barriers, the CPB path extends its hand with inclusivity. A high school diploma or its equivalent is often recommended, but the absence of rigid degree requirements grants entry to aspirants from diverse intellectual and vocational landscapes. This open-door policy ensures that talent, rather than formal academic pedigree, remains the driving force behind participation.
Yet, while the academic threshold is lenient, the demand for real-world familiarity is steadfast. Prospective candidates are generally expected to possess two or more years of tangible experience in billing or related domains. Such stipulations are not arbitrary; they serve as a filter, allowing only those who have already weathered the unpredictable terrain of claim denials, insurance intricacies, and coding ambiguities to step forward. This requirement transforms the CPB examination from a mere theoretical assessment into an applied measure of lived competency.
Experience, after all, is the hidden curriculum. No textbook can truly simulate the tension of resubmitting a rejected claim or the persistence required to untangle labyrinthine payer policies. These challenges are the crucibles that shape billing professionals, and the exam seeks to measure not just memory but judgment born from such encounters.
The CPB journey also entices candidates toward professional membership, though it does not impose it as an obligation. Joining a structured community of peers presents manifold advantages. From discounted examination fees to a treasury of educational resources, workshops, and professional symposiums, such affiliations often evolve into long-term investments. While the lone candidate may march ahead without joining, the fortified community stands as an invaluable citadel of shared wisdom and support, guiding aspirants well beyond the exam itself.
The act of registration, though administrative in appearance, symbolizes the transformation of intention into commitment. The first step requires the creation of a secure account through the official platform, followed by navigation toward the certification menu where the CPB exam is listed. Once identified, the candidate is presented with the choice between a traditional in-person venue or the modern convenience of online proctoring. This duality embodies the flexibility of contemporary education and assessment—catering equally to those who thrive in physical environments and those who require the adaptability of remote access.
Upon remittance of the examination fee, the candidate officially crosses into the preparatory realm. Yet, this transaction is more than a financial exchange—it is a psychological threshold. For many, the moment of payment conjures both exhilaration and apprehension. The abstract dream now carries tangible weight, binding the candidate to a forthcoming challenge. Registration, in this light, is not a perfunctory step but a declaration of intent, marking the genesis of the certification odyssey.
Strategies for Studying and Preparing for Success
Preparation for the CPB exam is as much an art as it is a discipline. The enormity of the subject matter can intimidate even the most diligent learner if approached without a strategy. Success requires more than rote memorization; it demands comprehension of how disparate billing concepts converge within the intricate framework of healthcare systems. Those who master this interplay not only pass the exam but also cultivate skills transferable to real-world practice.
Crafting a Roadmap Through the Content Outline
The starting point of effective preparation is the exam content outline. This document functions as a compass, delineating every major subject area from regulatory mandates to submission procedures. Ignoring its structure is akin to wandering through an unfamiliar forest without a map. By aligning study sessions with each listed domain, learners distribute their effort intelligently rather than scattering it haphazardly. The outline becomes both a guardrail and a lantern, preventing detours while illuminating the scope of knowledge expected.
Prioritizing Official Materials
Authoritative manuals and sanctioned guides are indispensable. These resources are not simply informative; they are engineered to echo the exam’s architecture. Their carefully curated scenarios, exercises, and reference tables replicate the evaluative environment that candidates will encounter. Supplementary resources, such as independent textbooks or scholarly articles, can deepen understanding, but the official content provides the skeletal framework upon which all knowledge rests. To neglect these is to prepare with incomplete armor for a demanding battle.
The Power of Practice Exams
Simulated examinations are not merely drills; they are transformative tools that refine timing, sharpen recognition, and expose fragile areas of knowledge. Each incorrect response, though momentarily discouraging, unveils a fissure that can be mended before the official exam. Repeated exposure to the exam’s rhythm trains the mind to regulate pace, ensuring that candidates do not squander precious minutes pondering excessively over a single question. Over time, practice tests metamorphose anxiety into confidence.
The Communal Energy of Study Groups
Learning in isolation can feel sterile, while shared study cultivates vibrancy. When candidates gather—whether physically in study circles or virtually through discussion forums—they engage in dialectics that deepen comprehension. Wrestling with a convoluted reimbursement problem or dissecting coding anomalies alongside peers fosters perspectives no solitary reading could unveil. Moreover, the fellowship of others kindles motivation, transforming preparation from an arduous solo trek into a shared expedition. Moral encouragement within these groups often becomes the hidden fuel sustaining long-term effort.
Harnessing Structured Learning Platforms
For individuals who thrive on scaffolding, structured courses deliver essential discipline. Online programs and workshops weave together lectures, interactive simulations, and assessments, blending visual, auditory, and kinesthetic modalities. Scheduled classes impose accountability, reducing the risk of procrastination and anchoring the learner to a rhythm of progress. The synergy of guided instruction with independent review forms a powerful duet, ensuring both depth and breadth of knowledge acquisition.
Building Consistency Over Cramming
The temptation to compress vast learning into frantic bursts is alluring but treacherous. Knowledge absorbed hastily often evaporates just as swiftly. Consistent study, spread across weeks or months, encourages gradual internalization. Like a sculptor chiseling stone, daily effort refines understanding until concepts become instinctive. By exam day, the candidate is not scrambling to recall scattered facts but is thinking fluidly, weaving knowledge into coherent solutions reflective of real billing practice.
Developing a Personalized Study Ritual
Preparation thrives when infused with routine. Some learners absorb material best in the quiet hush of dawn, while others flourish under the serenity of late-night solitude. Crafting a ritual—whether beginning each session with a quick review of flashcards, or closing with a brief reflective journal—creates a rhythm that signals the brain to enter a focused state. These rituals transform abstract ambition into tangible progress, turning study from obligation into ritualized mastery.
Embracing Active Recall Techniques
Passive reading breeds illusionary competence, while active recall fortifies retention. Candidates should frequently close their books and attempt to reconstruct information from memory. By retrieving concepts rather than rereading them, the brain strengthens neural connections, ensuring durability of knowledge. Techniques such as self-quizzing, flashcards, or teaching material aloud to an imaginary audience elevate passive exposure into active engagement. Over time, recall becomes effortless, enabling rapid access during the actual exam.
The Value of Incremental Mastery
Instead of confronting the entire body of content at once, breaking it into digestible segments allows mastery step by step. Dividing study into thematic clusters—such as compliance regulations, coding protocols, or claim adjudication—creates a rhythm of gradual conquest. Each mastered cluster serves as a building block, leading to cumulative confidence. This incremental approach transforms the colossal mountain of preparation into a series of navigable foothills.
Using Errors as Catalysts for Growth
Mistakes, far from being adversaries, are invaluable instructors. Each incorrect answer in a practice exam or misunderstood regulation signals not failure, but opportunity. By dissecting the root of an error, candidates unearth hidden misconceptions or overlooked details. Such revelations are not setbacks but accelerants, driving refinement of understanding. Those who embrace mistakes as allies inevitably transform weaknesses into fortified strengths.
The Role of Time Management
Success is not dictated solely by knowledge but by the orchestration of time. The exam demands efficiency, and every candidate must learn the rhythm of measured pacing. Allocating time proportionately to questions, resisting the temptation to dwell excessively on difficult items, and reserving moments for review are critical strategies. Time management during preparation—structuring daily study hours, balancing review with practice, and scheduling breaks—mirrors the discipline required on exam day.
Cultivating Mental Resilience
Beyond intellect, psychological fortitude is essential. Anxiety and fatigue can derail even the most prepared candidate. Techniques such as deep breathing, visualization, or brief mindfulness practices can quiet nerves and sharpen focus. Approaching the exam with composure transforms nervous energy into purposeful concentration. Mental resilience not only sustains candidates during study but ensures clarity when faced with the pressure of the timed exam environment.
Integrating Real-World Context
The CPB exam is not an abstract puzzle but a mirror of authentic billing practice. Relating study material to real-world scenarios enriches comprehension. Visualizing how regulations influence patient claims, or how coding decisions impact reimbursement, embeds theoretical knowledge within a practical framework. This contextualization ensures that answers emerge not as memorized fragments but as logical extensions of professional reasoning.
The Significance of Review Cycles
Repetition is the guardian of retention. Establishing cycles of review—revisiting older material periodically rather than abandoning it after initial mastery—prevents knowledge decay. Each review cycle deepens familiarity, transforming once-complex material into second nature. These spirals of repetition reinforce neural pathways, ensuring that even nuanced regulations and procedural codes remain readily accessible.
Balancing Study With Rest
Relentless study without interludes of rest is counterproductive. The mind, like a muscle, requires recovery to consolidate learning. Short breaks during study sessions enhance focus, while adequate nightly sleep consolidates memory and enhances problem-solving capacity. Rest is not wasted time but a vital partner in preparation. Candidates who respect the interplay of effort and restoration cultivate sharper recall and sustained energy.
The Momentum of Self-Reflection
Throughout preparation, pausing to reflect upon progress provides clarity and motivation. Journaling insights, noting persistent challenges, or recording small victories creates a tangible narrative of growth. This record not only reinforces commitment but also highlights areas still requiring attention. Reflection transforms study from a mechanical exercise into a conscious journey, imbuing the process with meaning and direction.
The Culmination of Preparation
When exam day arrives, success is not the product of last-minute cramming but the culmination of deliberate, consistent, and reflective preparation. The candidate who has engaged with the outline, prioritized official resources, practiced diligently, collaborated with peers, and cultivated resilience walks into the exam with calm assurance. Success then becomes not a gamble but a predictable outcome of disciplined preparation.
The CPB examination is designed to probe the subtle depths of billing acumen. It traverses the labyrinthine corridors of healthcare regulations, the multifaceted architecture of coding systems, the intricacies of insurance frameworks, the fine-grained nuances of reimbursement policies, and the precision demanded by documentation standards. The test does not isolate these realms in silos; instead, it intertwines them, mirroring the tangled realities of professional billing, where disparate fragments of knowledge must merge into coherent judgment under pressing time.
Candidates encounter abrupt shifts in focus, almost like an orchestral piece moving from one tempo to another. A question might first demand recognition of the exact code for a given claim transaction, and immediately thereafter pivot into a scenario exploring compliance with fraud-prevention statutes. This oscillation reflects the unpredictable demands placed upon billers, compelling examinees to exhibit agility, analytical sharpness, and intellectual endurance.
Sample questions embody this complexity. One could inquire which coding lexicon best represents medical procedures, with options including ICD-10-CM, CPT, or HCPCS. Another might probe the candidate’s grasp of remittance advice indicators or demand identification of the correct HIPAA electronic transaction format. Each item is more than a static query—it is a miniature simulation of actual billing work, where meticulousness determines whether a claim moves smoothly through the revenue cycle or collapses into denial and delay.
Scoring is calibrated at a threshold of seventy percent, requiring mastery of at least ninety-five questions to secure success. While numerically modest, the diversity of subject matter transforms this target into a formidable hurdle. A candidate cannot indulge in selective preparation; every dimension must be nurtured with equal attention. A deficit in even a single area can cascade into an insufficient overall performance.
The absence of punitive marking offers a small but critical advantage. Guesses, if educated and informed by partial knowledge, may transform into lifesaving points. This detail underscores a tactical reality: one should never abandon a question unanswered, for even a speculative response might provide the margin between triumph and defeat.
The Scope of Regulatory Mastery
Healthcare billing operates under a canopy of stringent regulations. The CPB exam ensures that aspirants are not merely acquainted with statutes but are capable of navigating them as living frameworks. Laws addressing privacy, anti-fraud safeguards, and compliance mandates are interlaced with billing scenarios to examine whether candidates can translate theoretical awareness into functional decision-making.
In this sense, the exam functions almost as a sieve, filtering those who can internalize law into practice from those who treat it as abstract. Questions test recognition of subtle boundaries—when is a claim a clerical misstep, and when does it risk transgressing into fraudulent representation? Such discernment is not trivial; it is the very fulcrum upon which professional integrity pivots.
The Architecture of Coding Systems
Medical coding is the linguistic skeleton of billing. The exam probes knowledge of ICD-10-CM for diagnoses, CPT for procedures, and HCPCS for supplies and services, demanding fluency in their distinct yet interdependent structures. What makes the task daunting is not just rote memorization but the ability to discern which classification applies under specific clinical contexts.
For instance, a question may pose a clinical vignette describing a surgical intervention. The candidate must identify not only the procedural code but also consider modifiers, ancillary supplies, and the associated diagnosis that justifies medical necessity. The cognitive demand here mirrors actual billing practice, where precision can be both the shield against audit and the key to timely reimbursement.
The Mosaic of Insurance Plans
Insurance landscapes are rarely uniform. The CPB exam recognizes this heterogeneity by incorporating questions spanning government-funded programs, commercial policies, managed care organizations, and supplemental coverages. Each plan type imposes its own labyrinth of requirements, and the exam demands recognition of these subtle divergences.
A scenario might involve contrasting reimbursement rules for the same service under two different plans. The candidate must demonstrate the discernment to navigate contractual stipulations, prior authorization demands, and benefit limitations. Such knowledge is indispensable, for real-world billers act as translators between healthcare providers and payers, ensuring that financial communication is both accurate and compliant.
Reimbursement Policies and Revenue Cycles
The lifeblood of medical practice flows through its revenue cycle, and the CPB exam is uncompromising in testing competence here. Questions may dissect the chronology from patient registration through charge capture, claim submission, payment posting, and follow-up on denials. Each phase is vulnerable to disruption, and the candidate must show mastery of identifying, correcting, and preventing those disruptions.
Reimbursement is not merely mechanical; it is influenced by fee schedules, contractual adjustments, and payer-specific protocols. A question may challenge candidates to identify why a claim was underpaid or denied, requiring the application of knowledge across coding, documentation, and insurance contract interpretation. This integrative skill mirrors the daily vigilance demanded in professional billing.
Documentation as a Pillar of Accuracy
Documentation is the anchor that stabilizes the billing process. Without accurate, timely, and comprehensive records, coding collapses into speculation. The exam presses candidates to interpret what constitutes sufficient documentation for different services and to distinguish between acceptable shorthand and inadequate or risky omissions.
For example, an exam item may present a clinical note with ambiguous phrasing and ask which code most accurately reflects the service. This forces candidates to internalize the maxim that documentation dictates billing—not assumptions, not intentions, but the written record. Such rigor protects both provider and patient, shielding against audit findings and ensuring fair compensation.
The Psychological Dimension of Scoring
While the technical domains dominate the content, the scoring system itself influences candidate behavior. Knowing that the passing bar sits at seventy percent shapes strategy. Some candidates pace themselves meticulously, allocating time evenly across all questions, while others lean on instinct and intuition, moving swiftly through familiar territory to conserve energy for more complex scenarios.
The design of the exam acknowledges psychology as much as knowledge. The absence of negative marking encourages risk-taking within reason, reinforcing the principle that educated guessing is preferable to hesitation. This dimension transforms the test from a static evaluation into a dynamic psychological exercise, demanding stamina, composure, and tactical adaptability in addition to intellectual breadth.
Integrative Competence as the True Measure
At its core, the CPB exam does not merely reward isolated pockets of knowledge. Its architecture is intended to measure integration—the seamless weaving together of regulations, codes, reimbursement rules, and documentation into a coherent practice. This integrative competence mirrors reality, where a billing professional cannot compartmentalize tasks but must continuously connect dots under time pressure.
Success, therefore, is not just about memorization but about cultivating the ability to synthesize and apply. It is about transforming disparate fragments of knowledge into a living, breathing professional instinct. Those who achieve this synthesis are the ones who surpass the seventy percent threshold, not merely as test-takers but as practitioners ready to uphold the exacting standards of the profession.
The Broader Implication of Examination Rigor
The CPB exam is not only an assessment but also a safeguard for the integrity of healthcare’s financial infrastructure. By enforcing mastery across all dimensions, it ensures that certified professionals can function as guardians of accuracy, compliance, and efficiency. This rigor elevates not only the individual but the collective trust in the billing process, protecting both institutions and patients.
In this way, the test transcends its immediate role as a certification mechanism. It becomes a gatekeeper of quality, filtering candidates through intellectual pressure to ensure that those who emerge are capable of maintaining the delicate balance between healthcare delivery and financial stewardship.
Conclusion: The Journey Beyond the Score
The CPB exam is a demanding crucible, blending content diversity with psychological challenge. Its structure, questions, and scoring method are all designed to replicate the turbulence of real-world billing practice, where knowledge must be agile, integrative, and precise. Success requires not only technical preparation but also resilience, adaptability, and a willingness to embrace uncertainty as part of the process.
To view the passing score as the sole destination is to misunderstand the essence of the exam. The true journey is one of transformation—shaping candidates into professionals capable of stewarding the revenue cycle with integrity and skill. Passing the exam marks the beginning, not the culmination, of a career where the lessons learned in preparation continue to resonate across every claim filed, every code selected, and every compliance safeguard upheld.
Educational Pathways, Retakes, and Renewal of Certification
Preparation for professional certification does not end with textbooks or exam guides. For many aspirants, the journey begins with structured educational pathways offered through academic institutions or specialized training providers. Certificate programs in medical billing and coding provide not only theoretical instruction but also pragmatic exposure. These courses often integrate internships that allow learners to immerse themselves in real-world scenarios, bridging the divide between classroom concepts and practical application.
Online learning has emerged as a transformative force for working professionals who must balance employment, personal responsibilities, and study. Virtual classrooms, interactive simulations, and flexible timetables enable candidates to refine their expertise without abandoning current obligations. Webinars and live workshops also offer direct engagement with seasoned professionals, who share nuanced insights into evolving billing practices and shifting healthcare regulations. In this way, preparation becomes an ongoing dialogue with a community of practitioners rather than a solitary endeavor.
The possibility of failing an initial attempt should never be interpreted as a final defeat. Exams can be retaken, though candidates must anticipate fees and scheduled waiting periods. Paradoxically, failure often functions as a compass, pointing directly to areas requiring reinforcement. An unsuccessful attempt sharpens focus, fosters resilience, and transforms vague ambition into deliberate action. The road to mastery is rarely linear, and determination often proves more valuable than immediate triumph.
Once success is achieved, certification does not remain static. The credential demands renewal, reflecting the reality that healthcare is in perpetual motion. Knowledge that is adequate today may be obsolete tomorrow. Renewal is structured through Continuing Education Units accumulated over a two-year cycle. Candidates document their participation in seminars, advanced coursework, and workshops before submitting them with the renewal fee. This system ensures that certified professionals remain vigilant stewards of current practices and adaptive interpreters of new regulations.
Renewal should not be seen as a burden but rather as a catalyst for growth. It draws professionals into vibrant networks of educators, practitioners, and innovators. It compels ongoing dialogue with fresh ideas and fosters intellectual agility. Renewal is also an implicit pledge to employers and patients alike: a commitment that the professional is not merely certified but continually evolving, refined, and sharpened by exposure to new knowledge.
The Broader Impact of the CPB Credential
Certification is more than a personal accolade; it reverberates outward, enhancing the credibility of entire healthcare organizations. A certified biller ensures precision in financial operations, minimizing costly errors while safeguarding compliance with regulations. Physicians, nurses, and clinical staff can focus their energies on patient care, secure in the knowledge that claims are accurate, reimbursements optimized, and administrative risks mitigated. In this sense, the credential strengthens not just individuals but entire healthcare ecosystems.
For the individual professional, certification is both a gateway and a shield. It opens avenues to higher salaries, increased recognition, and greater professional autonomy. Employers interpret the CPB credential as a symbol of reliability and expertise, making certified billers especially valuable in a competitive labor market. The credential functions like a seal of trustworthiness, signaling to employers that the holder possesses mastery over complex financial processes and regulatory frameworks.
Yet the significance of certification is not confined to material gains. It carries intangible rewards that ripple across professional and personal spheres. Confidence grows from the recognition that one has conquered a rigorous standard. Identity is strengthened through membership in a community of peers bound by shared discipline and purpose. These intangible benefits cultivate pride, deepen motivation, and instill a profound sense of belonging.
The Certified Professional Biller may remain unseen by patients, but their presence is felt in every functioning clinic and hospital. Each correctly processed claim translates into sustained resources for medical staff, equipment, and patient services. In this way, the biller becomes a silent architect of continuity in healthcare, an unseen partner in the art of healing. The CPB credential thus transcends its immediate financial function, becoming a safeguard for the stability and vitality of entire communities.
Renewal as a Lifelong Journey
The act of renewing certification symbolizes something larger than compliance. It embodies the philosophy of lifelong learning. Healthcare is not static; regulations shift, technologies emerge, and expectations evolve. Those who embrace renewal as a natural rhythm of professional life gain not only relevance but also agility. They become perpetual learners, individuals who do not fear change but rather see it as fertile ground for growth.
Workshops, symposiums, and professional gatherings serve as laboratories of thought. They expose billers to innovations in digital claim processing, updates in insurance laws, and ethical considerations that evolve alongside technology. These settings transform renewal into exploration, where knowledge is refreshed, expanded, and contextualized.
Renewal also has a ripple effect beyond the individual. Certified professionals who pursue advanced learning become mentors for newcomers, transmitters of wisdom to peers, and sources of stability for their organizations. Their pursuit of excellence nourishes the professional culture of their workplace, ensuring that teams are not only compliant but also visionary.
Retakes as Catalysts of Growth
Retaking an exam often carries a stigma, yet in truth it is an invaluable stage of refinement. Few achievements worth pursuing are secured on the first attempt. Retakes grant candidates the opportunity to return with deeper insight, greater precision, and reinforced knowledge. They transform frustration into fuel, showing that endurance can be as crucial as intellect.
In many ways, the act of retaking reshapes character. It teaches patience, resilience, and the discipline of repeated effort. The lessons learned from an unsuccessful attempt often prove more enduring than those from easy victories. When candidates finally achieve certification after one or more retakes, the credential holds a profound personal resonance, symbolizing not just knowledge but tenacity.
Educational Pathways as Bridges
Educational pathways serve as bridges, connecting aspiration with achievement. Structured programs provide scaffolding for learning, ensuring that complex topics are broken down into digestible segments. These courses cultivate both breadth and depth, enabling candidates to see the larger system while mastering intricate details.
Internships embedded within educational pathways infuse realism into theoretical knowledge. By engaging with billing systems, interacting with healthcare teams, and handling live scenarios, students gain tactile experience. This direct exposure accelerates confidence and clarifies abstract principles. When candidates later face certification exams, they carry with them not only memorized information but also a lived familiarity with the discipline.
The diversity of educational pathways also fosters accessibility. Whether through intensive campus programs, part-time evening courses, or flexible online schedules, aspirants from varied backgrounds can find routes tailored to their circumstances. The multiplicity of options reflects the inclusive nature of the profession, inviting individuals with diverse life situations into its fold.
Certification as a Social Contract
Beyond its technical meaning, certification operates as a social contract. It is an implicit promise between the professional and the society they serve. It assures patients that those handling financial documentation are not only skilled but also ethical. It assures employers that certified staff will uphold compliance, accuracy, and integrity.
This contract extends further, symbolizing accountability. By earning and renewing certification, professionals declare their willingness to be evaluated, scrutinized, and held to a standard higher than personal convenience. In this sense, the CPB credential is not merely a qualification but a statement of responsibility.
Preparing for the Certified Professional Biller (CPB) exam is both an intellectual and psychological expedition. It requires more than rote memorization; it demands cultivated strategy, disciplined study habits, and a deep capacity to synthesize knowledge into applied wisdom. To master this exam, candidates must approach preparation as a deliberate process—structured yet flexible, methodical yet adaptable. What follows is an exploration of essential tips and tricks, designed to elevate your preparation journey and maximize the possibility of success.
Crafting a Study Blueprint
The first step in mastering the CPB exam is to design a comprehensive study plan. Wandering aimlessly through books and notes often leads to fragmented learning. A blueprint provides order, transforming the monumental task into manageable sections. Begin by dividing the exam domains into distinct categories such as regulations, coding systems, insurance policies, reimbursement procedures, and documentation standards. Allocate specific weeks to each area, ensuring balanced attention.
A blueprint is not static; it should be adjusted according to personal progress. If you discover weaknesses in coding systems, elongate that section of study. If regulations feel intuitive, redistribute time toward areas where mastery is less secure. In this way, the plan becomes a living document, evolving with your growing competence.
Immersion in Terminology
The CPB exam is steeped in specialized vocabulary. Fluency in this lexicon is non-negotiable. Terms such as “remittance advice,” “capitation,” “modifier,” or “bundling” may seem abstract, yet on the exam they are wielded with precision. Building a robust glossary early in your preparation helps avoid confusion when these terms appear in nuanced questions.
Create flashcards, whether physical or digital, and practice them daily. Speak the words aloud, write them repeatedly, and use them in sentences. The more natural they feel, the faster your recognition will be during the timed exam. This immersion reduces hesitation and increases confidence when confronted with complex scenarios.
Simulated Practice Under Pressure
Studying theory alone is insufficient. The CPB exam challenges not only what you know but how quickly and accurately you can deploy it under time constraints. Thus, regular practice with timed mock exams is indispensable. These simulations recreate the psychological stress of the real test, training your mind to remain steady while navigating shifting topics.
Do not merely score your practice tests—analyze them. Identify patterns in your mistakes. Are you misreading questions? Struggling with specific coding scenarios? Losing time on long passages? Each insight provides an opportunity for refinement. Over time, these mock sessions transform weaknesses into strengths, ensuring you enter the actual exam hall with practiced composure.
Mastery of Regulations and Compliance
A substantial portion of the exam revolves around regulatory frameworks. Laws such as HIPAA, anti-fraud safeguards, and payer compliance rules often appear intertwined with billing scenarios. Candidates must not simply memorize statutes but learn to interpret them in context.
One effective trick is to study regulations through real-world examples. Consider a hypothetical claim scenario and ask: How would HIPAA apply here? What compliance risk might emerge if documentation is incomplete? By embedding the law within lived scenarios, you transform abstract rules into practical instincts, making recall easier during the test.
Navigating Coding Systems with Confidence
The coding sections of the CPB exam are often the most intimidating. ICD-10-CM, CPT, and HCPCS each have distinct structures and uses, yet they overlap in ways that require careful discernment. To master them, candidates must practice not only code identification but also decision-making in context.
One effective method is comparative drilling. Take a single clinical scenario and attempt to code it using all three systems. Which applies, and why? This exercise forces you to distinguish the boundaries of each system while sharpening recognition of subtle details. Over time, this comparative approach develops the mental flexibility to pivot between coding frameworks swiftly—a skill essential for success on the exam.
Understanding the Landscape of Insurance Plans
Insurance diversity is another domain where candidates often stumble. Government-funded programs, commercial carriers, managed care models, and supplemental plans each carry unique billing requirements. A trick to mastering this area is to visualize insurance types as different dialects of the same language. They all share the goal of reimbursement, but their rules, exceptions, and documentation standards vary.
Create flowcharts or diagrams to capture the distinctions between plans. How does Medicaid differ from a managed care organization? What are the documentation expectations for a commercial carrier versus a government payer? By organizing information visually, the complexity becomes less overwhelming and easier to recall under exam pressure.
Precision in Documentation Awareness
Documentation is the silent backbone of billing accuracy. Without adequate notes, no claim can stand. The exam probes whether you understand not just what documentation is required, but also how to identify inadequacies.
To strengthen this skill, practice evaluating mock clinical notes. Search for missing details: Is the diagnosis clearly stated? Does the procedure align with the documented complaint? Are modifiers needed to clarify the service? This exercise develops a meticulous eye, which not only serves exam success but also translates into professional vigilance in real-world billing.
Time Management Strategies
The CPB exam spans a large number of questions, each demanding careful thought. Without disciplined time management, even well-prepared candidates may falter. Begin by setting a target pace—decide how many questions should be completed every half hour. During practice tests, train yourself to adhere to this rhythm.
A useful trick is the “flag-and-move” technique. If a question feels unusually time-consuming, mark it and move on. Preserve time for questions you can answer with certainty, then circle back later to the flagged items. This ensures that you maximize your score potential by securing easy points before grappling with complex problems.
The Power of Educated Guessing
One often-overlooked trick is the strategic use of educated guessing. Since the CPB exam does not penalize incorrect answers, leaving a question blank is always worse than attempting an informed guess. Eliminate clearly wrong options, then weigh the remaining choices logically. Even without complete certainty, this approach significantly increases the chance of landing on the correct answer.
Practice this skill deliberately during mock exams. Train your intuition by analyzing why certain distractors appear plausible yet incorrect. Over time, your educated guesses will become sharper, providing the marginal points that may separate passing from failing.
Building Mental Stamina
The CPB exam is lengthy, and fatigue can erode performance as the hours pass. Preparing your mind and body for endurance is just as important as studying the content. Simulate exam conditions: sit for extended practice sessions without distractions, limit breaks, and cultivate focus for hours at a stretch.
In addition, nourish your body before study and on exam day with foods that sustain concentration rather than spike energy temporarily. Hydration, rest, and regular breaks during preparation all contribute to long-term stamina. A sharp, rested mind retains information more effectively and performs better under pressure.
Harnessing Group Study Dynamics
While solitary study builds concentration, group study sessions can unlock new dimensions of understanding. Engaging with peers exposes you to diverse perspectives, explanations, and problem-solving approaches. Discussing regulations, debating coding choices, or quizzing one another on terminology transforms passive reading into active learning.
However, group study should be strategic. Avoid sessions that devolve into casual conversation. Set specific goals: one session may focus solely on insurance distinctions, another on mock test review. Structured collaboration multiplies retention and strengthens your ability to articulate concepts, which deepens mastery.
The Final Week Before the Exam
The last week of preparation is crucial. This is not the time to learn entirely new material but to consolidate, review, and reinforce. Focus on weak areas identified during earlier practice, revisit glossaries, and run through timed mock exams to sharpen pacing.
Resist the temptation to cram excessively the night before. Instead, prioritize rest, light review, and mental calmness. Entering the exam hall exhausted undermines months of preparation. Confidence emerges not from frantic last-minute memorization but from disciplined consistency leading up to the test.
Transforming Preparation into Mastery
Mastering the CPB exam requires more than knowledge; it requires strategy, adaptability, and resilience. Crafting a study blueprint, immersing in terminology, practicing under timed conditions, and cultivating mental stamina all serve as pillars of success. By weaving these tips and tricks into your preparation, you transform the daunting exam into a navigable challenge.
Success on the CPB exam is not merely the result of intellectual effort but the culmination of structured preparation, psychological readiness, and tactical execution. Those who approach it with this holistic mindset emerge not only with certification but with sharpened skills that resonate far beyond the exam hall—skills that define excellence in the profession of medical billing.
A Silent Pillar of Healthcare
The story of certification, retakes, and renewal is not merely academic but profoundly human. It is the narrative of perseverance in the face of setbacks, of renewal in the midst of change, and of pride in quiet yet essential contributions. The Certified Professional Biller may not stand at the bedside, but their precision ensures that care is funded, sustained, and extended.
Each pathway studied, each retake endured, and each renewal embraced is a thread woven into the larger fabric of healthcare. Collectively, these efforts uphold not only the careers of individuals but also the stability of entire institutions. Certification, therefore, is both personal and communal, both a goal and a journey.
In the end, the CPB credential is not just a mark of competence but a quiet proclamation of dedication, a testimony to the unseen guardianship of healthcare’s financial heartbeat. It embodies preparation, perseverance, and renewal—three pillars upon which the integrity and vitality of modern healthcare firmly rest.
Conclusion
Mastering the CPB exam is not about last-minute memorization but about cultivating steady discipline, strategic planning, and applied understanding. By blending structured study schedules with immersive practice, strengthening familiarity with coding systems and insurance landscapes, and honing skills in documentation and compliance, candidates prepare themselves not only for exam success but for the realities of professional billing. Time management, psychological readiness, and tactical approaches such as educated guessing transform preparation into performance. Ultimately, these study tips and tricks serve as more than tools for passing an exam—they are the foundation of a resilient, knowledgeable, and adaptable professional capable of thriving in the ever-evolving world of healthcare billing.