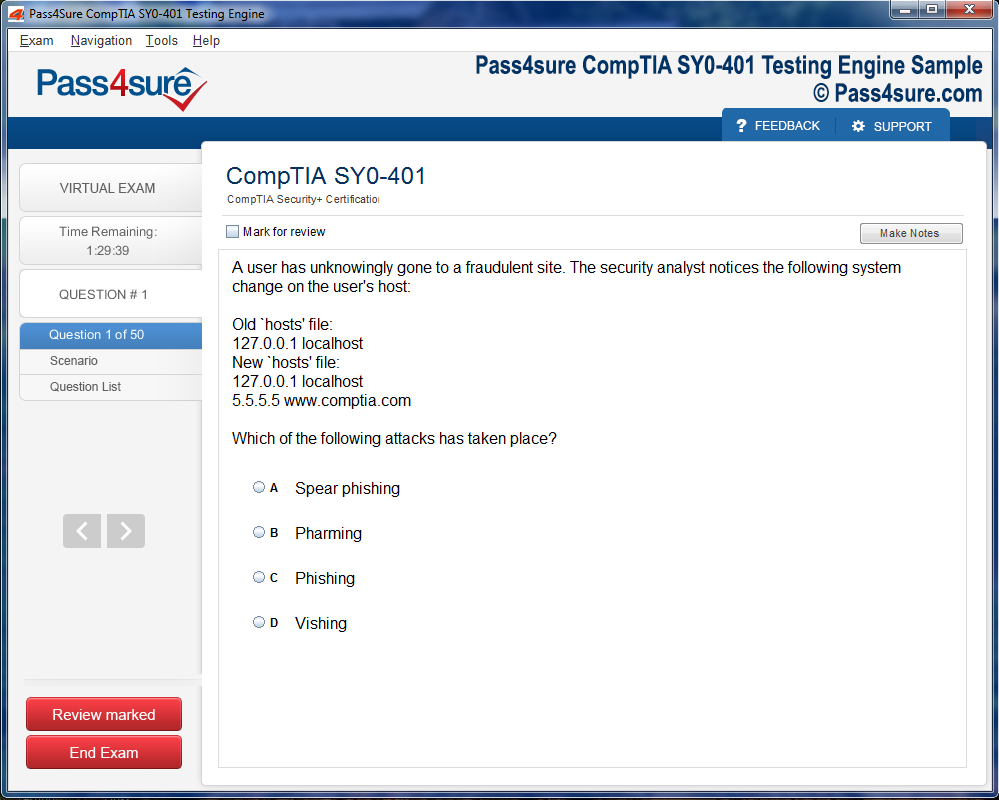
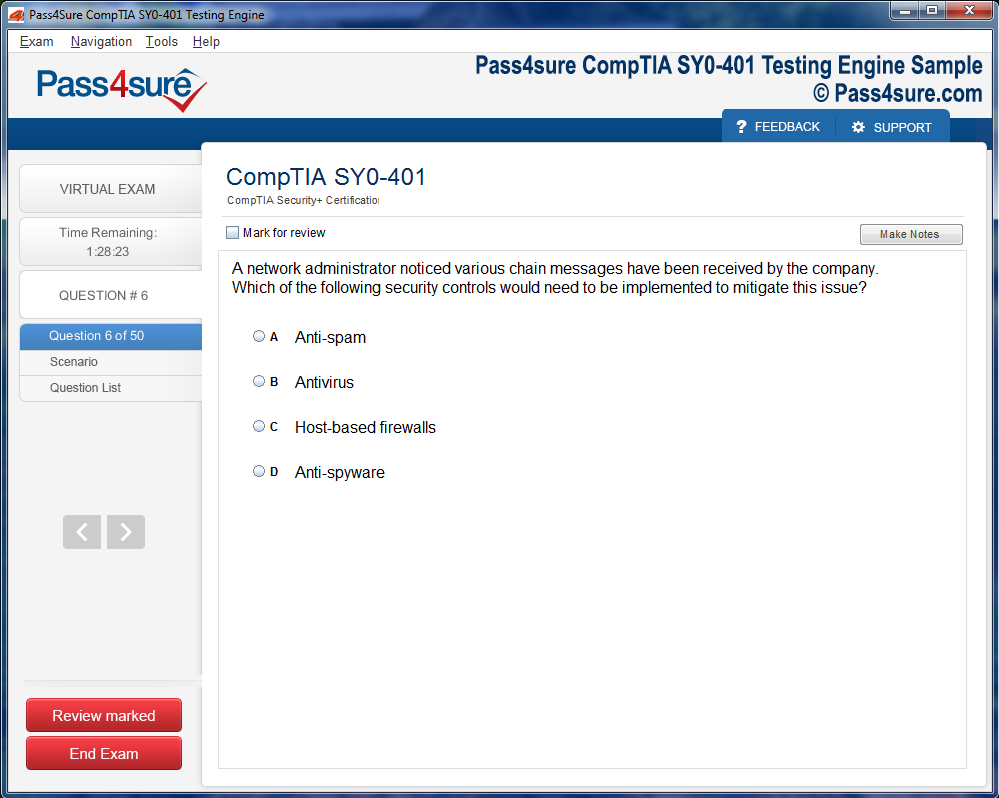
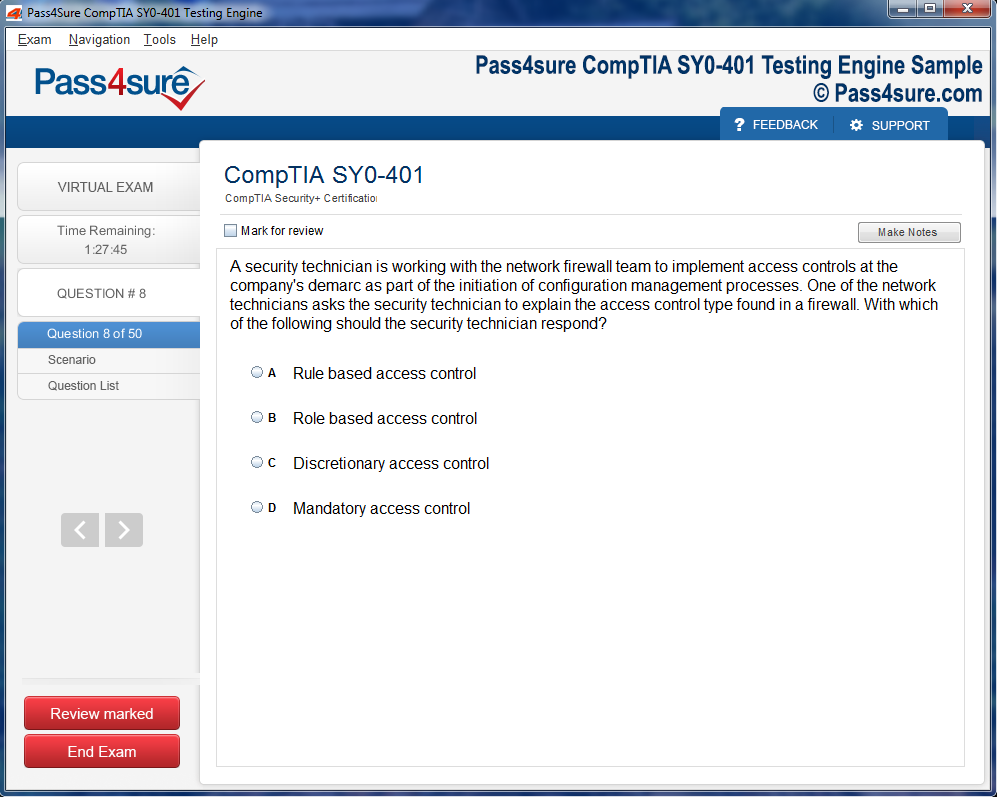
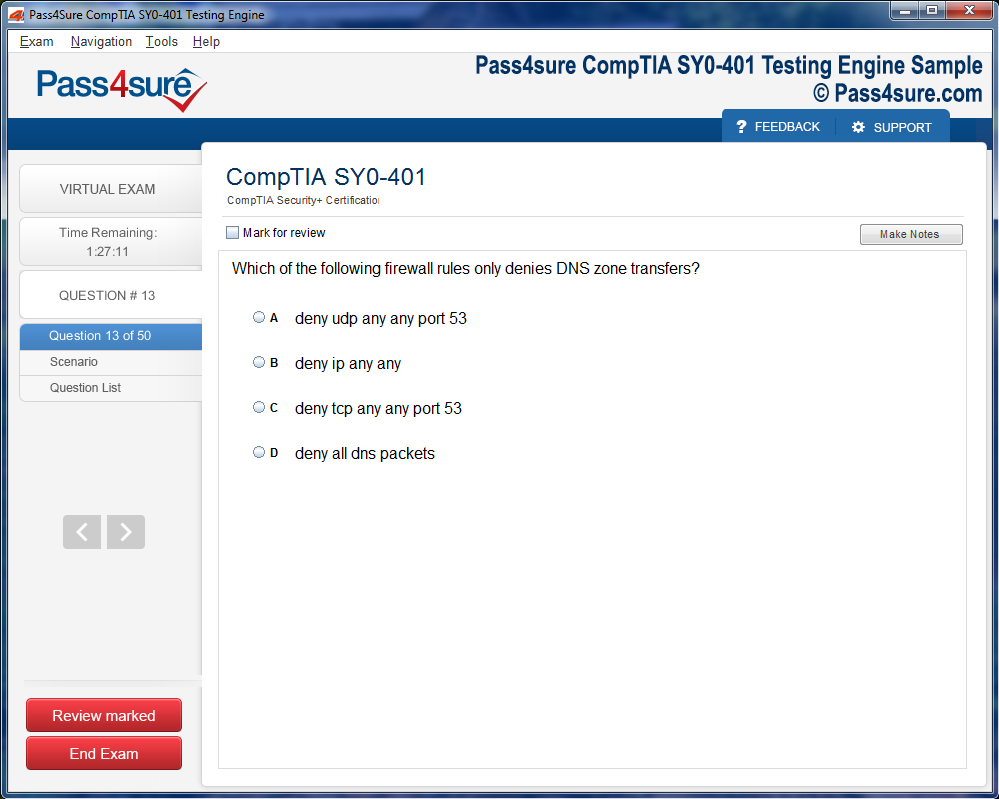
Product Screenshots
Frequently Asked Questions
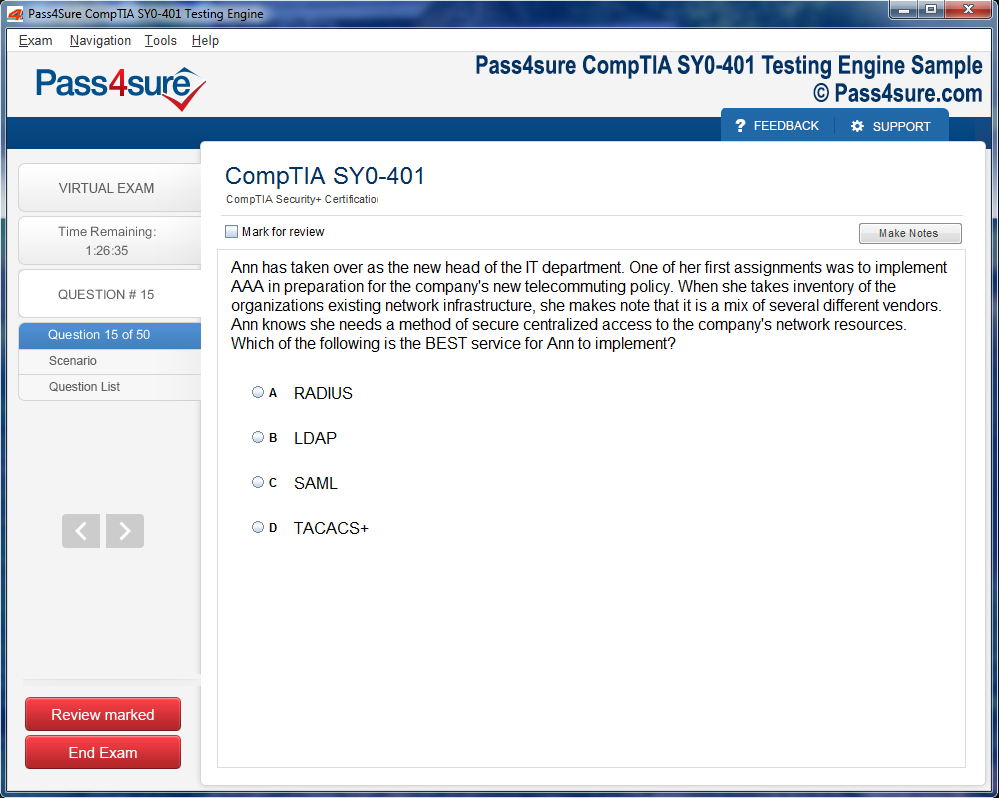
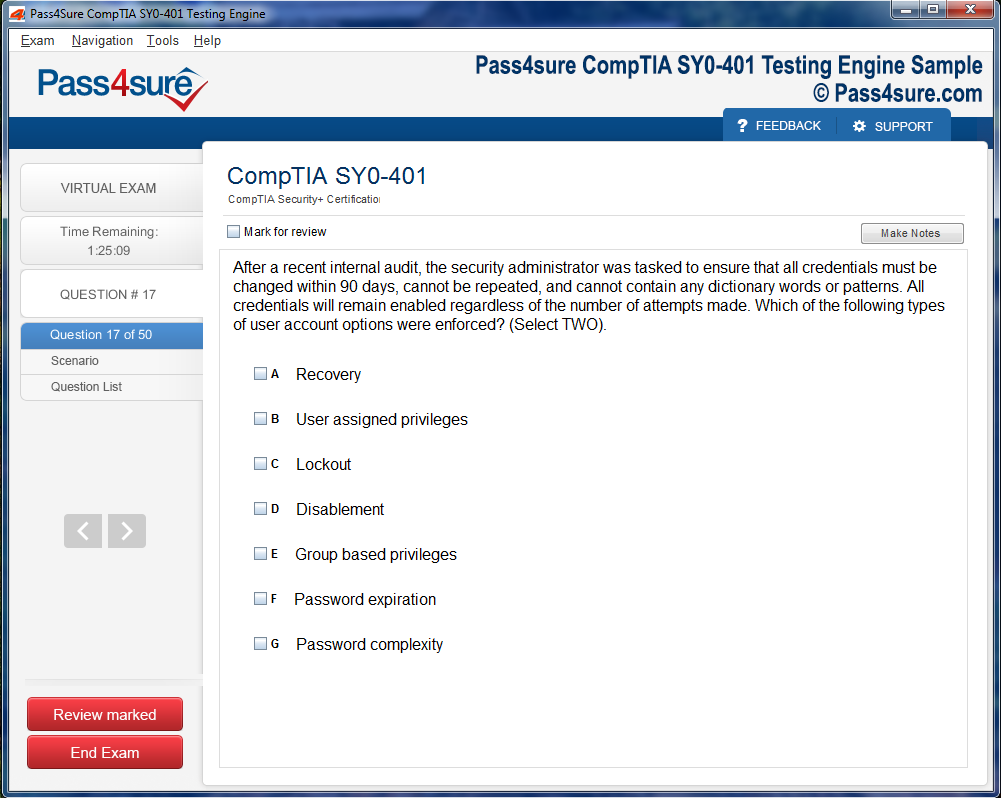
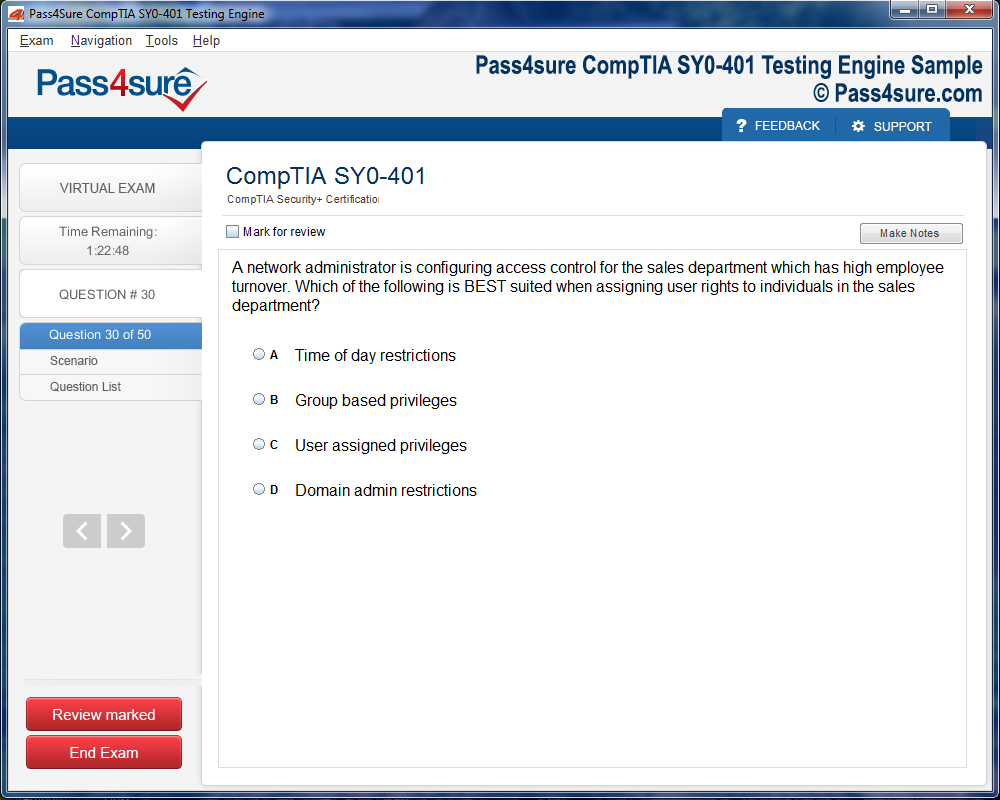
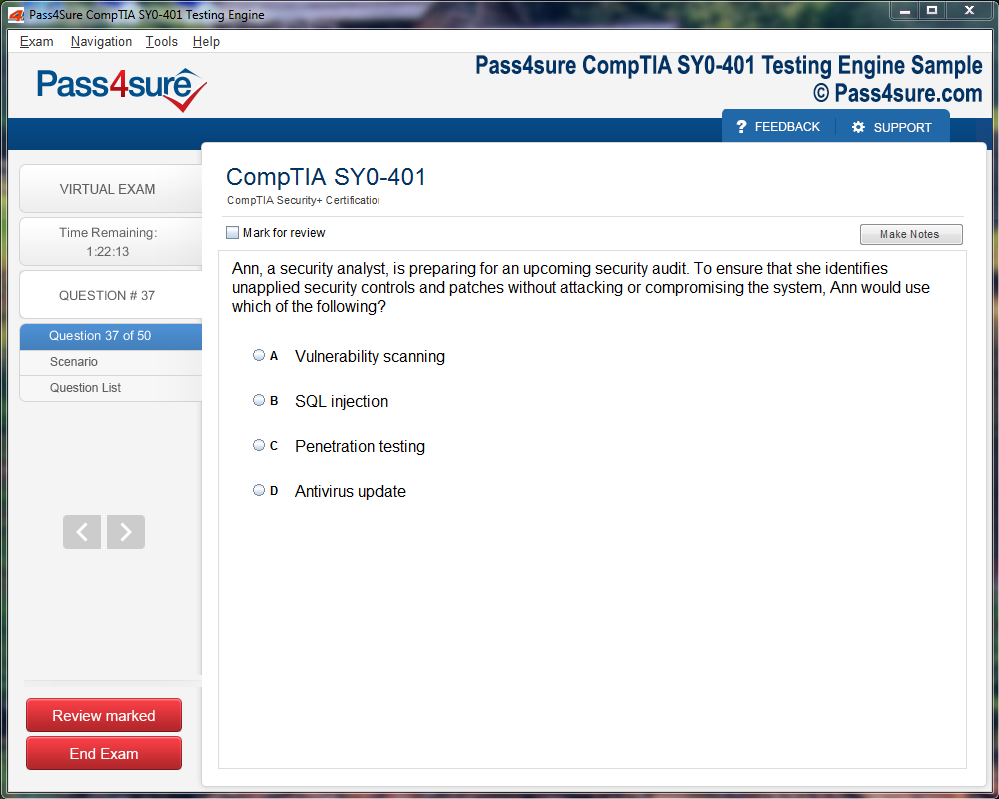
How does your testing engine works?
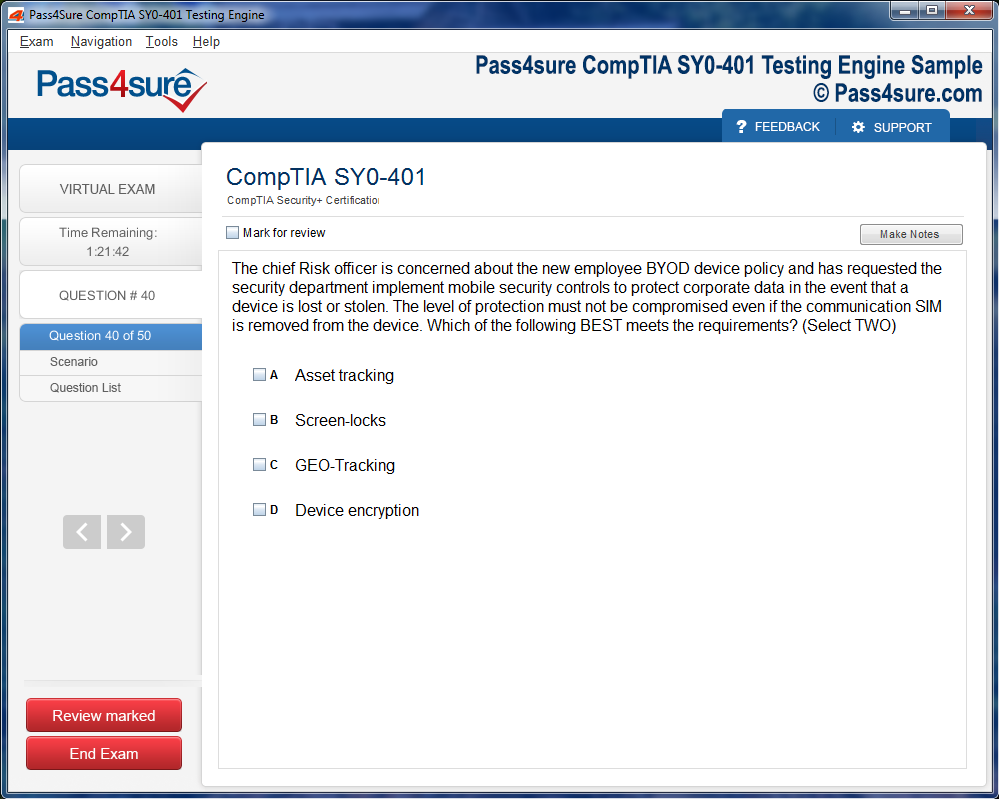
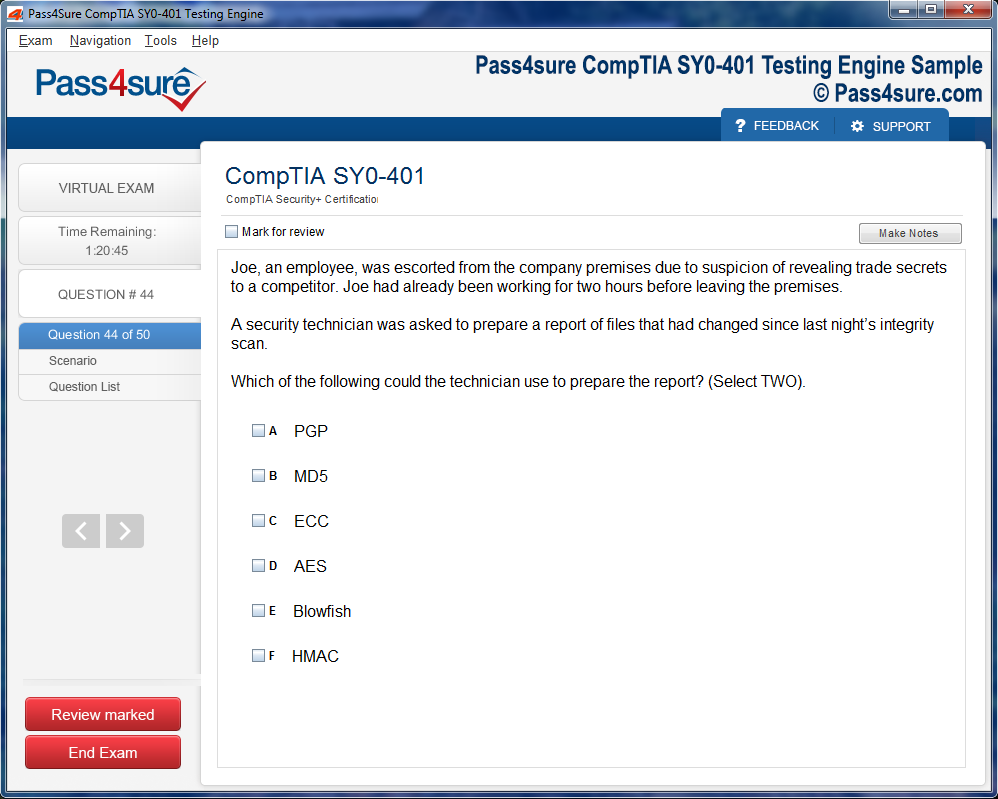
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations.
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.
The Insider’s Guide to First-Time AHIP AHM-250 Success
Navigating the labyrinthine corridors of healthcare payer systems necessitates an erudite comprehension of core principles, coupled with an aptitude for deciphering multifaceted operational mechanisms. At the epicenter of this domain lies health insurance, a discipline interweaving fiscal stewardship, legislative policy, and patient welfare in an intricate symphony. Aspiring candidates approaching the AHIP AHM-250 examination must anchor their preparation in a solid understanding of these foundational concepts, for they constitute the scaffolding upon which advanced insights are constructed. Health insurance, in essence, operates as a sophisticated risk redistribution apparatus, amalgamating contributions from disparate entities to shield individuals and families from potentially catastrophic medical expenditures. Mastery of diverse plan architectures—including comprehensive coverage, high-deductible paradigms, and niche benefit structures—imbues candidates with the dexterity to navigate the examination with both precision and poise. Each plan encapsulates distinctive underwriting doctrines and coverage stipulations, and discerning these subtleties equips candidates to respond to nuanced scenarios with acuity.
Concomitantly, an intimate familiarity with managed care models emerges as an indispensable pillar in healthcare payer literacy. Managed care endeavors to orchestrate equilibrium among cost efficiency, accessibility, and quality outcomes, frequently through intricate provider networks and methodical care delivery protocols. Health maintenance organizations exemplify tightly regulated networks, emphasizing preventative interventions to mitigate long-term morbidity. Preferred provider organizations, conversely, afford broader latitude in provider selection, albeit at a commensurate premium, while point of service plans amalgamate features from both, striking a synthesis between autonomy and cost containment. Accountable care organizations elevate this paradigm further, embedding population health strategies within provider accountability frameworks to optimize both clinical and fiscal outcomes. Proficiency in these operational archetypes enables candidates to appreciate the interplay between healthcare delivery methodologies, expenditure moderation, and policy formulation, a perspective indispensable for navigating real-world applications and examination queries alike.
Regulatory adherence represents another cornerstone of payer competence, characterized by a confluence of federal mandates, state-level directives, and seminal healthcare reforms. These legal frameworks delineate operational boundaries, data stewardship responsibilities, and member protection obligations. For instance, HIPAA enshrines stringent safeguards around sensitive health information, while the Affordable Care Act prescribes coverage obligations and mandates transparency in benefits communication. Understanding these legislative constructs allows candidates to approach both theoretical constructs and pragmatic case studies with a compliance-oriented lens. Beyond mere statutory obedience, apprehending the underlying rationale of regulatory edicts offers strategic insight into organizational policy evolution, facilitating a deeper comprehension of how payer systems adapt in response to shifting legal and sociopolitical landscapes.
Equally salient is the emphasis on member experience, a domain extending well beyond superficial customer service interactions. Member engagement encompasses the full spectrum of touchpoints, including enrollment procedures, claims adjudication, grievance resolution, and proactive health management initiatives. In contemporary healthcare ecosystems, where patient-centric paradigms drive both satisfaction and retention, payers must harmonize operational efficiency with empathetic interaction. Immersing oneself in the intricacies of these interactions equips candidates with a nuanced understanding of how strategic operational decisions influence outcomes, fostering an analytical mindset that is invaluable for both examination scenarios and practical application. Appreciating the subtleties of member communications, from initial onboarding to chronic condition management, cultivates an integrated perspective of healthcare payer responsibilities and operational dynamics.
Strategic preparation for the AHIP AHM-250 examination requires intentionality, blending conceptual study with applied practice. Engaging with official AHIP resources, such as comprehensive study guides, scenario-based case studies, and practice assessments, exposes candidates to content reflective of authentic exam challenges. Simulating examination conditions through timed exercises enhances cognitive endurance, hones decision-making acuity, and fortifies time management capabilities. The synergy of foundational comprehension and practical application fosters a multidimensional understanding of healthcare payer principles, establishing a resilient intellectual framework upon which advanced learning and professional mastery can be scaffolded. By embedding deliberate practice within a structured study regimen, candidates cultivate the dexterity necessary to traverse the complex topography of payer operations and emerge with both confidence and competence.
Health insurance constitutes a labyrinthine ecosystem where policy architecture, fiscal prudence, and member experiences intersect. Understanding this complexity requires an exploration of nuanced paradigms that dictate plan structures, coverage parameters, and risk mitigation mechanisms. Each insurance plan embodies a delicate interplay of deductibles, co-pays, and out-of-pocket ceilings, entwined with provider networks that shape access and affordability. Delving into these intricacies equips aspirants with the acuity to decipher situational questions with precision, cultivating analytical prowess beyond superficial familiarity.
Underwriting, a cornerstone yet often underestimated, orchestrates the evaluation of actuarial risk and the meticulous calibration of benefits. Insurers synthesize demographic patterns, health behaviors, and clinical histories to ascertain premium allocations and eligibility criteria. A keen grasp of these assessments illuminates operational rationales behind coverage determinations, enabling candidates to navigate hypothetical scenarios with judicious reasoning. Mastery of underwriting principles transforms abstract statistical formulations into practical insights, enhancing problem-solving capabilities in real-world exam contexts.
Benefit design occupies a central role in harmonizing cost management with member engagement. Strategically structured plans incentivize preventative care, optimize therapeutic adherence, and attenuate long-term expenditures. Tiered formularies, wellness initiatives, and incentive-based programs illustrate the symbiosis between design choices and health outcomes. Analyzing these models provides candidates with experiential knowledge of how plan architecture influences utilization patterns, retention rates, and clinical efficacy. This dimension underscores the importance of bridging theoretical comprehension with pragmatic healthcare strategies.
Operational proficiency forms the bedrock of sustainable health insurance administration. Enrollment workflows, claims adjudication, and appeals processes exemplify the intricate choreography required to maintain compliance, ensure timeliness, and foster member trust. Simulating these operational sequences during preparation cultivates an intimate understanding of procedural subtleties, enhancing responsiveness to scenario-driven inquiries. This applied orientation transforms procedural knowledge into actionable competence, reinforcing the capacity to navigate both theoretical constructs and practical exigencies.
Integrating underwriting, benefit design, and operational mechanics yields a holistic comprehension of the health insurance landscape. Consistent engagement with case studies, practice examinations, and reflective analyses deepens familiarity with nuanced question formats and thematic complexities. Evaluating errors, dissecting rationales, and iterating on challenging concepts reinforces retention and strategic insight. Candidates embracing this multidimensional methodology cultivate confidence, analytical dexterity, and nuanced problem-solving aptitude, thereby fortifying preparedness for the AHIP AHM-250 examination.
The confluence of these domains highlights the sophistication inherent in health insurance ecosystems. Understanding risk stratification, actuarial calculations, and benefit interplay allows candidates to appreciate the delicate equilibrium between financial sustainability and member-centric care. Each scenario presents an opportunity to translate theoretical knowledge into applied reasoning, demonstrating the tangible impact of informed decision-making on health outcomes and organizational performance.
An awareness of regulatory frameworks further contextualizes health insurance operations. Compliance mandates, reporting obligations, and quality metrics intersect with operational practices, guiding insurer behavior and member interactions. Exam candidates benefit from analyzing these intersections, which illuminate why procedural rigor and policy adherence are indispensable for effective administration. This regulatory lens adds another layer of sophistication to the candidate’s analytical toolkit, enhancing capacity for nuanced reasoning and evidence-based conclusions.
Technological integration, increasingly pivotal, reshapes member experiences and administrative efficiency. Data analytics, predictive modeling, and digital engagement platforms facilitate precise risk assessments, streamlined claims processing, and personalized health interventions. Exam preparation that incorporates an understanding of these innovations equips candidates to address questions reflecting contemporary trends and operational transformations, reinforcing relevance in rapidly evolving healthcare environments.
Equally critical is the comprehension of behavioral economics in influencing member decisions. Copayment structures, tiered benefits, and incentive programs subtly guide adherence patterns and preventative care uptake. Recognizing these psychological underpinnings allows candidates to anticipate the ramifications of design choices, linking theoretical insight to practical impact. This synthesis of human behavior and policy design enriches analytical perspectives and enhances strategic reasoning capabilities in exam scenarios.
The interplay between cost containment and quality optimization remains a persistent theme in health insurance discourse. Candidates must grapple with the delicate balance between financial stewardship and clinical efficacy, considering how network design, formulary management, and utilization review shape both fiscal outcomes and patient health trajectories. Mastery of these interconnections cultivates the ability to respond to scenario-based prompts with depth and nuance, reflecting a sophisticated understanding of the insurer-member dynamic.
Moreover, the longitudinal perspective on member engagement illuminates the cyclical nature of health outcomes and insurance utilization. Preventative initiatives, chronic disease management, and wellness incentives exemplify strategies that foster sustained health improvements while mitigating downstream costs. Evaluating these approaches within exam preparation enhances comprehension of long-term planning, resource allocation, and the broader systemic consequences of policy decisions.
Scenario analysis, a cornerstone of AHIP exam success, benefits from immersive study in simulated operational and clinical contexts. Candidates who dissect real-world cases, trace decision-making pathways, and evaluate outcomes develop a refined capacity to navigate complex situational queries. This iterative approach fosters analytical agility, ensuring that responses are grounded in both conceptual understanding and practical application.
Risk stratification, integral to underwriting and benefit management, demands careful attention. Understanding population health trends, actuarial assumptions, and predictive modeling enables candidates to anticipate cost implications, tailor interventions, and support sustainable plan design. This analytical skill set strengthens the ability to evaluate nuanced questions that probe both operational logic and strategic foresight.
A nuanced appreciation of communication dynamics complements operational and analytical expertise. Clear, transparent member interactions, precise documentation, and empathetic provider engagement constitute essential competencies. Candidates who internalize these principles are better equipped to evaluate scenarios that incorporate human factors, demonstrating an integrated perspective that transcends rote memorization.
The multidimensional complexity of claims adjudication underscores the necessity for precision and consistency. Evaluating documentation, applying policy rules, and navigating exceptions requires attention to detail, regulatory knowledge, and procedural acumen. Exam preparation that simulates these adjudication processes reinforces competence, enhancing confidence and accuracy in scenario-based assessments.
Incorporating lessons from quality measurement initiatives strengthens understanding of value-based care paradigms. Metrics such as HEDIS scores, patient satisfaction indices, and outcome-based performance benchmarks illustrate the tangible impact of policy and operational decisions on health system performance. Candidates benefit from exploring these indicators, connecting data-driven insights with strategic decision-making, and refining analytical reasoning for exam applications.
Understanding the financial architecture of health insurance further amplifies exam readiness. Premium setting, reserve management, risk corridors, and reinsurance arrangements exemplify mechanisms that ensure fiscal viability while maintaining coverage integrity. Candidates who grasp these principles can better interpret scenario-based questions involving plan sustainability, risk allocation, and cost management strategies.
Member segmentation, a strategic component of benefit design and underwriting, highlights the heterogeneity of healthcare needs. Tailoring interventions, incentives, and communication strategies according to demographic, clinical, and behavioral characteristics enhances both engagement and cost-effectiveness. An appreciation of segmentation principles equips candidates with the analytical lens necessary to tackle complex situational questions with precision.
The integration of digital health solutions continues to redefine engagement and efficiency. Telehealth platforms, remote monitoring devices, and personalized health portals offer novel avenues for preventive care, chronic disease management, and operational streamlining. Familiarity with these technologies enriches understanding of contemporary health insurance paradigms and enhances candidates’ capacity to contextualize scenarios within modern operational realities.
Finally, cultivating a reflective and iterative approach to exam preparation consolidates knowledge and builds confidence. Reviewing practice questions, analyzing reasoning pathways, and revisiting challenging concepts foster cognitive reinforcement. Candidates who embrace this strategy develop both strategic foresight and analytical resilience, ensuring preparedness for the multifaceted demands of the AHIP AHM-250 examination.
The synthesis of operational precision, strategic insight, behavioral understanding, and technological awareness forms a robust foundation for navigating health insurance complexity. Candidates equipped with this multidimensional perspective are poised to interpret, analyze, and resolve the nuanced challenges presented in exam scenarios, translating comprehensive knowledge into demonstrable exam success.
Mastering Managed Care and Operational Dynamics
Managed care manifests as a confluence of clinical acumen, fiscal stewardship, and member-centric orchestration. It privileges coordinated interventions, anticipatory health strategies, and judicious resource allocation. For aspirants of the AHIP AHM-250 examination, grasping the subtle demarcations among health maintenance organizations, preferred provider organizations, point of service arrangements, and accountable care consortia is imperative. Each archetype harbors singular operational protocols, network geometries, and incentive architectures, collectively influencing both clinical efficacy and organizational alacrity.
Health maintenance organizations exemplify an ethos of preventive vigilance, embedding provider oversight within circumscribed networks. The paradigm enforces gatekeeping, wherein primary care stewards modulate specialist ingress, safeguarding cost-effectiveness while nurturing clinical prudence. Conversely, preferred provider organizations venerate expansive access and operational elasticity, though they frequently entail augmented expenditures, necessitating nuanced management to harmonize member gratification with financial equilibrium. Point of service constructs synthesize these modalities, engendering hybrid mechanisms that demand dexterity in coordination, communication, and procedural adaptability. Familiarity with these dynamics equips candidates to prognosticate operational impediments and navigate complex scenario-based interrogatives with aplomb.
Accountable care organizations inject a strategic lens, entwining population health stewardship with provider accountability. Such entities valorize outcome-oriented frameworks, risk-sharing matrices, and streamlined care pathways. Proficiency in population health analytics, quality indicators, and cost-containment stratagems is indispensable for candidates aspiring to demonstrate operational mastery. Engaging with pragmatic illustrations—ranging from performance dashboards to incentive realignment—illuminates the evolving topography of managed care, revealing how efficiency, quality, and satisfaction coalesce.
Operational excellence transcends mere plan taxonomy. Precision in claims adjudication, sagacity in provider contracting, and acumen in utilization management remain cardinal. Candidates benefit from dissecting workflows, scrutinizing key performance metrics, and internalizing best practices that uphold regulatory fidelity while optimizing member experience. Experiential modalities—simulations, case vignettes, and applied exercises—transmute theoretical constructs into operational fluency.
Parallel to operational comprehension is the imperative understanding of the regulatory scaffold enveloping managed care. Federal mandates, state statutes, HIPAA imperatives, and ACA provisions sculpt plan design, reporting protocols, and member communication channels. Mastery of these frameworks is crucial not only for exam excellence but for pragmatic application, where noncompliance carries tangible consequences. By synthesizing operational dexterity, strategic insight, and regulatory literacy, candidates cultivate a comprehensive command of managed care, equipping them to navigate both didactic and scenario-oriented assessments adeptly.
The intricacies of provider network architecture further underscore the necessity for strategic foresight. Network optimization entails balancing breadth of access with cost containment, assessing provider quality metrics, and negotiating contractual levers that incentivize adherence to evidence-based guidelines. Advanced candidates must discern subtle variations in network tiering, referral protocols, and credentialing benchmarks, recognizing that even marginal adjustments in these parameters can reverberate through clinical outcomes and financial performance.
Financial stewardship in managed care is equally nuanced. Prospective payment models, capitation schemes, and value-based reimbursement structures demand a sophisticated understanding of actuarial assumptions, risk corridors, and performance-linked compensation. Candidates adept in these constructs can anticipate fiscal pressures, recommend mitigation strategies, and align operational tactics with overarching organizational imperatives. The interplay between financial incentives and clinical behavior underpins the efficacy of managed care, rendering analytical acuity indispensable for aspiring professionals.
Population health analytics represents a frontier in managed care sophistication. Integrating epidemiologic data, predictive modeling, and social determinants of health facilitates proactive interventions, reducing avoidable morbidity and optimizing resource utilization. Candidates who internalize these paradigms cultivate the ability to propose targeted strategies, interpret quality measures, and translate analytics into actionable operational directives. This competency bridges the chasm between abstract policy objectives and tangible member outcomes.
Equally vital is the cultivation of member engagement strategies. High-performing organizations employ multifaceted communication channels, digital portals, and personalized outreach to foster adherence, satisfaction, and loyalty. Understanding behavioral health motivators, cultural competency, and health literacy nuances empowers candidates to anticipate barriers, enhance participation, and evaluate program effectiveness. The synthesis of engagement tactics with clinical and operational strategies epitomizes the holistic mastery expected of advanced practitioners.
Technological integration underpins operational innovation in managed care. Electronic health records, claims adjudication platforms, and predictive analytics engines streamline workflows, enhance data fidelity, and enable real-time monitoring of clinical and financial indicators. Mastery of these tools, coupled with an appreciation of interoperability and cybersecurity imperatives, positions candidates to navigate the digital transformation landscape with agility and precision.
Strategic quality management remains a keystone of operational excellence. Employing evidence-based protocols, continuous improvement methodologies, and rigorous performance benchmarking ensures alignment with regulatory expectations and member-centric objectives. Candidates benefit from examining case studies, analyzing quality improvement initiatives, and understanding the mechanisms of corrective action plans, thereby internalizing a culture of accountability and precision.
Finally, cultivating adaptive leadership skills enhances effectiveness in managed care environments. Decision-making under uncertainty, negotiation acumen, and conflict resolution capabilities are essential for orchestrating complex networks of providers, stakeholders, and members. Candidates who appreciate the symbiotic relationship between leadership, operational efficacy, and member outcomes demonstrate a level of sophistication that extends beyond technical knowledge, underscoring their readiness to excel in both examination contexts and real-world applications.
Regulatory Compliance and Ethical Considerations
Compliance and ethics constitute the bedrock of resilient and credible healthcare payer operations, establishing a framework in which legality, accountability, and moral stewardship converge. Regulatory adherence is not merely a bureaucratic requirement; it functions as a safeguard that ensures plans operate within lawful parameters, protect the welfare of members, and uphold industry-wide standards. For aspirants preparing for the AHIP AHM-250 examination, cultivating an intricate understanding of federal mandates, state-specific directives, privacy protocols, and healthcare reform statutes is indispensable. HIPAA, the Affordable Care Act, alongside myriad localized requirements, serves as cardinal pillars that inform operational choices, data governance practices, and member engagement strategies.
The Health Insurance Portability and Accountability Act (HIPAA) dictates rigorous procedures for managing sensitive health information. It mandates protocols for secure data storage, controlled access, and judicious information sharing, underscoring the necessity for meticulous operational discipline. Candidates must appreciate how these compliance architectures permeate routine activities, influencing claims adjudication, communication with members, and coordination with healthcare providers. Simultaneously, the Affordable Care Act enunciates minimum essential coverage stipulations, transparency obligations regarding benefits, and mechanisms for risk adjustment, all of which shape the strategic architecture of payer operations. Proficiency in these domains empowers candidates to navigate scenario-based inquiries, merging statutory knowledge with pragmatic reasoning.
Ethical paradigms transcend mere regulatory conformity, embedding principles of fairness, transparency, and member advocacy into the organizational ethos. Healthcare payers navigate the delicate equilibrium between operational efficiency and a member-centric ethos, ensuring that procedural expediency does not compromise equitable access or optimal health outcomes. For examination aspirants, immersing oneself in ethical quandaries, illustrative case studies, and practical scenarios where regulatory adherence intersects with moral duty fosters nuanced critical thinking. This dual lens enables candidates to weigh competing imperatives and devise solutions that harmonize legal compliance with ethical integrity.
Mastery of compliance frameworks also fortifies strategic acumen. Regulatory instruments often mirror broader policy objectives such as cost containment, quality enhancement, and population health stewardship. Awareness of these underlying intentions equips candidates to anticipate systemic challenges, refine plan architecture, and orchestrate initiatives that cohere with both regulatory expectations and organizational goals. Internalizing the symbiosis of compliance and ethics demonstrates a sophisticated understanding of healthcare payer responsibilities—a competency that is rigorously evaluated on the AHIP exam and valued in professional practice.
Navigating the intricate labyrinth of healthcare regulation necessitates an appreciation for both prescriptive rules and discretionary interpretation. The interplay between statutory mandates and organizational policy produces scenarios that demand judicious decision-making, wherein operational protocols must align with legal imperatives while remaining adaptable to emergent challenges. HIPAA compliance, for instance, extends beyond static adherence; it requires dynamic risk assessment, incident response readiness, and continuous staff education to preclude inadvertent breaches. Such proactive engagement cultivates a culture of vigilance, reducing the likelihood of violations and fostering member trust.
Ethical stewardship within healthcare payer operations is equally nuanced. It encompasses transparent communication, equitable resource allocation, and advocacy for vulnerable populations. Candidates benefit from examining hypothetical dilemmas that juxtapose cost efficiency against clinical necessity, revealing the tensions inherent in operational decision-making. By dissecting these scenarios, aspirants develop the capacity to formulate resolutions that honor both statutory constraints and moral imperatives, thereby cultivating a holistic ethical lens indispensable for long-term professional efficacy.
The regulatory landscape is continuously evolving, shaped by policy reforms, judicial interpretations, and emerging public health priorities. Candidates preparing for the AHIP AHM-250 must remain attuned to shifts in legislation, such as modifications to HIPAA rules, ACA provisions, or state-specific health insurance mandates. Continuous engagement with these developments ensures that compliance strategies remain contemporaneous, safeguarding both operational integrity and member interests. This adaptability is a hallmark of exemplary payer management, reflecting not only regulatory literacy but also strategic foresight.
Integrating compliance and ethics into operational planning enhances organizational resilience. Risk mitigation strategies, internal audits, and performance monitoring are informed by a dual commitment to legal adherence and ethical accountability. For instance, when designing claims adjudication workflows, organizations must ensure accuracy and timeliness while safeguarding member confidentiality and maintaining transparency in decision rationale. This integrative approach fosters stakeholder confidence, strengthens regulatory positioning, and reinforces the moral credibility of the payer.
Regulatory compliance also functions as a catalyst for innovation within healthcare operations. Understanding the legislative impetus behind rules—whether incentivizing preventive care, enhancing data interoperability, or promoting population health management—allows payers to implement creative solutions that exceed mere legal obligations. By embracing this interpretive perspective, candidates cultivate the ability to envision operational models that not only comply with statutory standards but also deliver superior value to members, providers, and the broader healthcare ecosystem.
Ethical considerations underpin member interactions at every touchpoint. Communication, enrollment, benefits explanation, and grievance resolution must reflect a principled commitment to clarity, fairness, and responsiveness. Candidates benefit from exploring scenarios that challenge conventional decision-making, such as balancing limited resources against emergent member needs or negotiating provider agreements that optimize access without compromising quality. Mastery of these principles engenders a moral compass capable of guiding complex organizational choices.
Healthcare compliance is inextricably linked to data governance. Beyond HIPAA, payers must manage electronic health records, claims datasets, and actuarial information with precision, ensuring that privacy and security protocols are rigorously maintained. Candidates should appreciate the multidimensional nature of data stewardship, which encompasses risk assessment, encryption, audit trails, and breach notification procedures. A nuanced understanding of these mechanisms demonstrates an advanced operational literacy essential for both examination success and professional practice.
Ethics and compliance converge in strategic risk management. Organizations must anticipate potential pitfalls, ranging from regulatory infractions to reputational damage, and implement policies that preempt adverse outcomes. This proactive posture entails embedding ethical considerations into decision-making matrices, auditing mechanisms, and quality assurance protocols. By internalizing these principles, candidates acquire the capacity to champion initiatives that harmonize legal adherence, ethical integrity, and operational efficiency.
Ultimately, regulatory compliance and ethical responsibility are not discrete competencies but interdependent dimensions of effective healthcare payer management. HIPAA, the ACA, and state-specific mandates provide the structural framework within which ethical reasoning flourishes, guiding operational decisions that are legally sound, morally defensible, and strategically coherent. For AHIP AHM-250 candidates, a comprehensive grasp of these principles equips them to navigate multifaceted scenarios with confidence, ensuring that both examination performance and professional practice reflect an elevated standard of competence.
The dynamic interplay between regulatory statutes and ethical norms underscores the necessity of continuous learning and reflective practice. Candidates are encouraged to analyze emerging case law, policy updates, and industry innovations, thereby cultivating a mindset attuned to evolving standards of accountability. This sustained engagement fosters not only compliance proficiency but also the ethical discernment essential for navigating complex organizational landscapes.
In conclusion, compliance and ethics form the fulcrum upon which sustainable and credible healthcare payer operations pivot. Mastery of regulatory frameworks, coupled with nuanced ethical reasoning, empowers candidates to navigate the intricate terrain of healthcare administration, balancing statutory obligations, moral imperatives, and operational exigencies. For those preparing for the AHIP AHM-250 examination, internalizing these principles ensures both academic success and the cultivation of professional gravitas, positioning them as adept, conscientious stewards of healthcare resources.
Practical Application, Exam Strategy, and Time Management
Success in the AHIP AHM-250 examination necessitates a multifaceted approach, intertwining cognitive acquisition with tactical deployment and temporal orchestration. The transformation of abstract comprehension into operative acumen is pivotal, as candidates must traverse labyrinthine question structures and nuanced scenarios that mirror the exigencies of healthcare payer operations. Immersive exercises, such as case dissection, interactive simulations, and praxis-oriented workshops, serve as crucibles in which theoretical constructs are transmuted into functional proficiency. These engagements reinforce the symbiotic relationships among policy architecture, operational mechanics, and member outcomes, engendering a holistic grasp of systemic interdependencies.
Immersive Learning and Experiential Integration
Experiential engagement facilitates deep cognitive embedding, surpassing rote memorization by engendering contextual understanding. Candidates who immerse themselves in scenario-based exercises cultivate an intuitive discernment of policy intricacies, risk stratification, and operational contingencies. By navigating complex situational matrices, learners internalize decision-making heuristics, which are indispensable when confronting multifarious question typologies in the AHIP examination. This method fosters metacognition, allowing individuals to reflect upon their reasoning pathways, identify cognitive biases, and refine analytic precision. The iterative feedback from these exercises accelerates conceptual consolidation and enhances the agility with which candidates can traverse interrelated domains.
Timed Practice and Cognitive Endurance
The deployment of timed practice assessments is a sine qua non for cultivating exam endurance and decisional alacrity. Structured time constraints compel candidates to prioritize information, evaluate alternatives expeditiously, and mitigate the paralytic effects of cognitive overload. Strategic temporal allocation—discerning when to linger on complex items versus progressing through straightforward queries—optimizes overall performance. Review of incorrect responses is equally critical, providing insights into latent misunderstandings and reinforcing accurate cognitive schemata. Familiarity with multiple-choice constructs, scenario-based interrogatives, and application-oriented prompts further hones precision under temporal duress, ensuring a balance between speed and accuracy that is imperative for first-attempt success.
Strategic Domain Prioritization
Navigating the AHIP curriculum with judicious prioritization enhances retention and maximizes the efficacy of study hours. Candidates benefit from an analytical audit of domain weightage, identifying high-yield topics for concentrated focus while maintaining sufficient exposure to peripheral content. This hierarchical approach mitigates cognitive fatigue and fortifies long-term memory retention. Furthermore, adaptive strategies—wherein revision emphasis is modulated according to performance trends on practice exercises—cultivate an iterative feedback loop, reinforcing weak nodes while sustaining mastery of previously consolidated material. By orchestrating study sessions with deliberate intent, candidates can traverse the expanse of content with efficiency and strategic precision.
Active Recall and Cognitive Reinforcement
The cognitive architecture underpinning mastery is reinforced through active recall methodologies, which stimulate synaptic connectivity and enhance retrieval fluency. Techniques such as self-quizzing, scenario reconstruction, and mnemonic scaffolding engender durable memory traces that endure beyond superficial familiarity. Coupled with spaced repetition, these strategies mitigate the forgetting curve and cement complex interrelations between regulatory frameworks, operational protocols, and member-centric processes. Candidates who consistently engage in reflective practice not only solidify conceptual understanding but also cultivate an adaptive mindset capable of transposing knowledge to unforeseen problem contexts.
Scenario-Based Synthesis
Integrative synthesis of multifaceted scenarios is a hallmark of high-caliber preparation. By juxtaposing policy stipulations with operational exigencies, candidates develop an evaluative lens that discerns subtle interdependencies and emergent patterns. Case-based discussions—either peer-facilitated or self-directed—offer fertile ground for cultivating analytical dexterity and strategic reasoning. The extrapolation of outcomes from hypothetical operational interventions fosters anticipatory thinking, allowing candidates to preemptively assess consequences and devise robust solutions. This form of praxis not only enhances exam performance but also equips individuals with actionable insights applicable to professional environments.
Interdisciplinary Integration
Holistic mastery demands interdisciplinary integration, wherein candidates synthesize health insurance principles with managed care dynamics, compliance imperatives, and member services considerations. Such synthesis engenders a panoramic understanding of healthcare ecosystems, enabling nuanced responses to composite questions that traverse multiple knowledge domains. Interdisciplinary engagement cultivates cognitive elasticity, allowing candidates to traverse conceptual boundaries and construct coherent frameworks for complex problem-solving. By embracing this integrative mindset, learners cultivate both strategic insight and operational fluency, hallmarks of exam readiness and professional competence.
Revision Architecture and Methodical Reinforcement
Effective revision transcends perfunctory review, requiring methodical structuring and strategic focus. Candidates benefit from a layered approach, wherein foundational concepts are revisited, followed by targeted interrogation of areas exhibiting knowledge fragility. This scaffolding approach reinforces cognitive hierarchies, ensuring that elemental principles underpin more advanced analytic constructs. Additionally, embedding reflective exercises within revision routines fosters meta-analytical awareness, enabling learners to monitor progress, adjust tactics, and internalize feedback. By cultivating disciplined repetition and strategic exploration, candidates reinforce conceptual networks, bridging the divide between rote memorization and applied understanding.
Cognitive Mapping and Conceptual Architecture
Constructing cognitive maps enhances structural retention and conceptual clarity. Visualization techniques, flowcharting, and relational diagrams assist candidates in apprehending systemic interactions and operational hierarchies within healthcare payer frameworks. Cognitive mapping transforms abstract information into tangible schemas, facilitating rapid retrieval and adaptive application during the examination. By externalizing mental models, candidates gain the ability to traverse interlinked concepts with agility, fostering both analytical efficiency and strategic foresight. This visual-spatial approach complements traditional study methods, reinforcing learning pathways and enabling holistic assimilation of intricate material.
Anxiety Mitigation and Psychological Resilience
Examination success is as contingent upon psychological fortitude as it is upon intellectual mastery. Stress management strategies—such as mindfulness, controlled breathing, and cognitive reframing—mitigate performance-impairing anxiety, fostering composure under evaluative pressure. Temporal discipline, coupled with preparatory rigor, cultivates confidence, reducing cognitive load and enhancing decision-making acuity. Candidates who proactively address psychological variables are better equipped to sustain focus, allocate attention judiciously, and navigate complex scenarios without succumbing to cognitive paralysis. Psychological resilience thus becomes an integral component of strategic preparation, complementing content mastery with operational poise.
Integration of Official Resources
Leveraging official AHIP resources provides a structured foundation for content acquisition and assessment familiarization. These materials offer authoritative guidance on curriculum scope, question typology, and regulatory context, ensuring alignment between study efforts and examination expectations. Candidates who systematically integrate these resources into study routines reinforce conceptual accuracy, familiarize themselves with evaluative paradigms, and reduce uncertainty regarding content emphasis. Effective utilization of these materials, in conjunction with experiential exercises and practice assessments, establishes a robust preparatory ecosystem that bridges theoretical knowledge and applied competence.
Time Allocation and Prioritization Strategies
Meticulous time management is instrumental in navigating both preparatory and examination phases. Candidates should establish temporal hierarchies, allocating intensive focus to high-yield domains while maintaining distributed review of ancillary topics. Structured schedules, incorporating interleaved practice and reflective intervals, optimize cognitive retention and mitigate burnout. During the examination, candidates benefit from triaging items based on difficulty, ensuring efficient progression while reserving cognitive resources for complex scenarios. This disciplined approach harmonizes study efficacy with exam execution, maximizing both accuracy and speed.
Reflection and Iterative Learning
Reflective practice amplifies cognitive consolidation, enabling learners to interrogate reasoning processes, identify knowledge lacunae, and refine strategic approaches. Iterative learning—characterized by cyclic engagement with content, feedback assimilation, and adaptive recalibration—fosters continuous improvement and intellectual agility. By embedding reflective exercises within preparatory routines, candidates cultivate self-regulatory capacities, enhance metacognitive awareness, and optimize learning trajectories. This iterative methodology transforms preparation from linear content absorption into dynamic cognitive engagement, producing durable mastery and adaptive proficiency.
Bridging Theory and Practice
The interstice between theoretical comprehension and practical application is navigated through deliberate praxis. Candidates who engage in applied exercises, scenario enactments, and policy simulations develop functional fluency, translating abstract principles into actionable insights. This bridging process enhances analytic rigor, promotes operational understanding, and equips learners to address emergent challenges with dexterity. By contextualizing knowledge within realistic frameworks, candidates cultivate a nuanced appreciation of healthcare payer systems, fortifying both examination performance and professional capability.
Continuous Improvement and Performance Analytics
Systematic evaluation of performance metrics fosters continuous improvement and strategic refinement. Candidates who track practice assessment results, analyze error patterns, and adjust study interventions cultivate a data-driven approach to preparation. This analytical rigor enables targeted remediation, optimizes cognitive resource allocation, and enhances overall readiness. By embracing performance analytics, learners transform preparation into a feedback-informed process, ensuring iterative enhancement and sustained proficiency across all examination domains.
Professional Competence and Strategic Insight
Mastery of the AHIP curriculum transcends examination success, extending into professional competence and strategic insight. Candidates who internalize operational principles, regulatory frameworks, and member-centric strategies are equipped to navigate complex organizational landscapes with acumen. The integration of applied knowledge, analytic reasoning, and systemic understanding cultivates a professional persona characterized by credibility, foresight, and operational dexterity. Examination preparation thus becomes both an evaluative exercise and a developmental journey, reinforcing expertise and strategic perspective.
Applied Learning as a Catalyst for Certification
Deliberate application of knowledge accelerates the trajectory toward certification. Experiential engagement, scenario-based practice, and integrative synthesis transform passive learning into active mastery, enabling candidates to approach the AHIP AHM-250 examination with confidence. Applied learning reinforces theoretical constructs, hones decision-making skills, and cultivates the cognitive flexibility necessary to navigate complex evaluative landscapes. Through sustained praxis, candidates consolidate understanding, optimize exam performance, and secure the professional validation that accompanies successful certification.
Sustaining Focus and Cognitive Vigilance
Longitudinal success requires sustained attention and cognitive vigilance. Candidates benefit from structured study intervals, periodic reassessment of knowledge gaps, and the maintenance of strategic objectives. Cognitive endurance, coupled with methodical reinforcement, ensures resilience against fatigue, distractions, and performance fluctuations. By sustaining disciplined focus, learners navigate the multifaceted demands of examination preparation with composure, maximizing both retention and application of acquired knowledge.
Holistic Preparation and Integrative Competence
Ultimately, holistic preparation synthesizes content mastery, applied practice, strategic revision, and psychological readiness into an integrative competence framework. Candidates who harmonize these dimensions cultivate a robust skill set, encompassing analytical agility, operational understanding, and regulatory fluency. This integrated approach facilitates adaptive problem-solving, effective time management, and confident navigation of examination challenges. Holistic preparation positions learners not merely for assessment success but also for enduring professional efficacy within the evolving healthcare payer environment.
First-Attempt Success and Deliberate Mastery
Achieving first-attempt success on the AHIP AHM-250 examination is contingent upon deliberate mastery, strategic engagement, and disciplined execution. Candidates who synthesize theoretical understanding, applied practice, targeted revision, and reflective learning optimize both cognitive readiness and exam performance. By embracing an integrated approach that balances knowledge acquisition with practical application, learners cultivate the proficiency, confidence, and insight necessary to excel. First-attempt success is thus attainable through methodical preparation, iterative refinement, and unwavering focus on the intersection of content mastery and practical competence.
Embarking on the journey toward first-time success in the AHIP AHM-250 exam requires more than rote memorization; it demands strategic preparation, nuanced comprehension, and an appreciation for the underlying principles governing healthcare payer operations. This exam is not merely a test of knowledge—it is a demonstration of applied reasoning, regulatory acumen, and ethical insight. For first-time candidates, understanding the intricate balance between theoretical concepts and practical scenarios is essential.
The AHIP AHM-250 is designed to evaluate candidates on their proficiency across multiple domains, including regulatory compliance, healthcare plan design, risk management, quality improvement, and member engagement. Each of these areas requires careful attention, as questions often intertwine statutory knowledge with operational decision-making. To excel, candidates must cultivate a multidimensional understanding, blending analytical acuity with scenario-based judgment.
Strategic Study Planning
Success begins with a meticulously crafted study plan. First-time candidates often underestimate the breadth and depth of the exam, leading to fragmented preparation. An effective plan segments study materials into manageable domains, allocating time based on personal strengths and weaknesses. Utilizing active learning techniques, such as self-quizzing, scenario simulation, and concept mapping, reinforces retention far more effectively than passive reading.
An initial diagnostic assessment is invaluable. By identifying gaps in knowledge early, candidates can prioritize areas requiring deeper focus. For instance, a candidate comfortable with quality improvement metrics may need to devote additional attention to regulatory intricacies, such as HIPAA stipulations or risk adjustment mechanisms. Strategic planning ensures that preparation time is optimized and reduces the cognitive load associated with last-minute cramming.
Deep Dive into Regulatory Frameworks
Regulatory knowledge forms the backbone of AHIP AHM-250 success. Candidates must develop an intricate understanding of HIPAA, the Affordable Care Act, and pertinent state-specific regulations. Mastery of HIPAA requires familiarity with privacy and security rules, consent protocols, and breach notification procedures. It is insufficient to memorize statutes; candidates must contextualize how these regulations impact claims processing, member communications, and provider interactions.
The Affordable Care Act introduces additional layers of complexity, such as minimum essential coverage requirements, risk adjustment processes, and benefit transparency standards. First-time examinees benefit from analyzing case studies illustrating real-world applications, which deepen comprehension and foster critical thinking. Recognizing the intent behind regulatory mandates—whether promoting equitable access, cost containment, or quality improvement—enhances the ability to navigate scenario-based questions with confidence.
Ethical Considerations and Decision-Making
Ethics permeates every facet of healthcare payer operations. Beyond legal compliance, candidates must appreciate the moral imperatives guiding member advocacy, equitable access, and transparency. Ethical reasoning is particularly relevant in scenarios where operational efficiency conflicts with member-centered care. First-time candidates often encounter questions requiring nuanced judgment, where adherence to policy must be balanced against fairness and patient outcomes.
Engaging with hypothetical ethical dilemmas cultivates decision-making agility. By simulating scenarios in which resource allocation, provider negotiations, or benefit determinations pose moral conflicts, candidates enhance their capacity to propose solutions that are both legally compliant and ethically sound. This skill set is invaluable not only for exam success but for professional practice in a complex healthcare environment.
Mastering Quality Improvement Concepts
Quality improvement (QI) is another pillar of the AHIP AHM-250. Candidates must understand performance measurement, process optimization, and continuous improvement methodologies. Key concepts include HEDIS measures, patient satisfaction metrics, and population health initiatives. A robust grasp of QI allows candidates to evaluate organizational strategies, identify performance gaps, and recommend interventions that improve outcomes while maintaining regulatory compliance.
First-time examinees benefit from connecting QI concepts to practical applications. For example, understanding how risk stratification informs preventive care interventions or how performance metrics drive incentive programs enhances both comprehension and retention. Integrating theory with operational context ensures readiness for scenario-driven questions, which often require synthesis rather than simple recall.
Effective Study Techniques
High engagement in study sessions is crucial for retention. Techniques such as spaced repetition, active recall, and concept interleaving have demonstrated efficacy in long-term memory consolidation. Candidates should create visual aids, including flowcharts, diagrams, and tables, to distill complex processes into digestible formats. Additionally, forming study groups or discussion forums facilitates peer-to-peer learning, exposing candidates to diverse perspectives and interpretations.
Simulation exercises, including timed practice exams, are particularly valuable. They mimic the cognitive demands of the AHIP AHM-250, fostering time management skills and familiarizing candidates with question formats. Reviewing rationales for correct and incorrect answers reinforces conceptual understanding, allowing first-time candidates to internalize both substantive knowledge and the exam’s evaluative logic.
Understanding Healthcare Plan Design
Plan design comprehension is central to AHIP success. Candidates must grasp the intricacies of plan types, benefit structures, provider networks, and formulary management. Knowledge of how different designs impact member choice, cost-sharing, and population health outcomes is essential. Scenario-based questions often require candidates to evaluate trade-offs between plan efficiency and member satisfaction, necessitating analytical agility.
Understanding network adequacy, provider reimbursement methodologies, and value-based care arrangements enhances strategic awareness. Candidates who can integrate these elements into operational decision-making demonstrate a sophisticated grasp of healthcare payer management, a skill set that the AHIP AHM-250 seeks to evaluate rigorously.
Risk Management and Compliance Integration
Risk management is inherently intertwined with regulatory compliance. Candidates must appreciate how proactive risk mitigation protects both organizational integrity and member interests. Key areas include claims accuracy, fraud prevention, operational audits, and data governance. First-time examinees benefit from exploring examples where risk management intersects with compliance, such as detecting anomalies in claims data that could indicate fraud or operational inefficiency.
Integrating compliance and risk awareness requires analytical thinking and attention to detail. Understanding how policies, procedures, and monitoring mechanisms reduce organizational exposure while enhancing member trust is a hallmark of high-performing candidates. Scenario questions frequently assess this integrated perspective, challenging examinees to propose solutions that harmonize regulatory, operational, and ethical considerations.
Exam Day Strategies
Success on exam day hinges on both preparation and psychological readiness. First-time candidates should approach the AHIP AHM-250 with a structured plan for pacing, question triage, and stress management. Time allocation is critical, particularly for scenario-based questions that demand thorough analysis. Candidates should practice reading prompts carefully, identifying key information, and eliminating distractors before selecting responses.
Mental resilience is equally important. Techniques such as visualization, mindfulness, and strategic breathing exercises reduce anxiety and improve cognitive clarity. Adequate rest, nutrition, and hydration in the days leading up to the exam further optimize performance, ensuring that candidates can apply their knowledge with precision and focus.
Leveraging Available Resources
Numerous preparatory resources enhance first-time success, including official AHIP study guides, practice exams, and topic-specific webinars. Candidates should use these tools to reinforce understanding, identify knowledge gaps, and develop test-taking strategies. Importantly, resources should be integrated thoughtfully into a broader study plan rather than consumed haphazardly, ensuring maximum efficacy.
Supplementing structured materials with practical applications—such as analyzing case studies, engaging in discussion forums, or reviewing organizational policies—deepens comprehension. This approach encourages active learning, bridging the gap between theoretical knowledge and operational reality.
The Role of Reflective Practice
Reflective practice is a powerful, often underutilized tool in exam preparation. Candidates should periodically evaluate their study progress, identify patterns of misunderstanding, and adjust strategies accordingly. Reflection also fosters deeper conceptual integration, allowing examinees to connect discrete topics into a cohesive mental framework. For first-time AHIP candidates, reflective practice enhances not only exam readiness but also long-term professional competence.
Building Confidence and Motivation
Confidence is as critical as knowledge for first-time success. Candidates benefit from celebrating incremental progress, maintaining a positive mindset, and visualizing successful outcomes. Motivation can be sustained by linking exam preparation to broader career goals, emphasizing the value of AHIP certification in professional development. A confident, motivated mindset enhances cognitive performance and ensures that knowledge can be applied effectively under exam conditions.
Scenario-Based Mastery
Scenario-based questions are a distinctive feature of the AHIP AHM-250. First-time candidates must practice applying knowledge in realistic contexts, evaluating trade-offs, and justifying decisions. This skill requires both conceptual clarity and analytical agility. By dissecting scenarios methodically—identifying stakeholders, regulatory implications, ethical considerations, and operational outcomes—candidates cultivate the ability to respond accurately and efficiently.
Repeated exposure to scenario exercises also enhances pattern recognition, allowing examinees to anticipate common question types and streamline decision-making. This preparation reduces cognitive load during the exam, enabling candidates to allocate attention to higher-order analysis rather than recall alone.
Continuous Knowledge Reinforcement
Sustaining knowledge through continuous reinforcement is critical for first-time success. Candidates should revisit challenging topics regularly, integrate practice questions into study routines, and actively summarize key concepts. Techniques such as teaching concepts to peers, creating mnemonic devices, and generating illustrative examples promote deeper understanding and long-term retention.
Post-Study Self-Assessment
Regular self-assessment is a cornerstone of effective preparation. Candidates should periodically simulate full-length exams under timed conditions, analyze performance metrics, and adjust study plans accordingly. Reviewing incorrect answers in depth, understanding the rationale behind correct choices, and documenting insights ensures that mistakes are transformed into learning opportunities.
Conclusion
First-time AHIP AHM-250 candidates face a rigorous but navigable path to success. Strategic study planning, regulatory mastery, ethical reasoning, scenario-based proficiency, and psychological preparedness collectively form the foundation for achieving high performance. By integrating structured preparation, active learning, and reflective practice, candidates can approach the exam with confidence, clarity, and competence.
Success is not merely the result of memorizing facts but of cultivating a comprehensive understanding of healthcare payer operations, regulatory compliance, and ethical stewardship. First-time candidates who internalize these principles, practice diligently, and maintain focus on strategic objectives are well-positioned to excel. Achieving AHIP AHM-250 certification for the first time is a testament not only to knowledge but to perseverance, analytical acumen, and professional integrity, setting the stage for a distinguished career in healthcare management.