Product Screenshots
Frequently Asked Questions
How does your testing engine works?
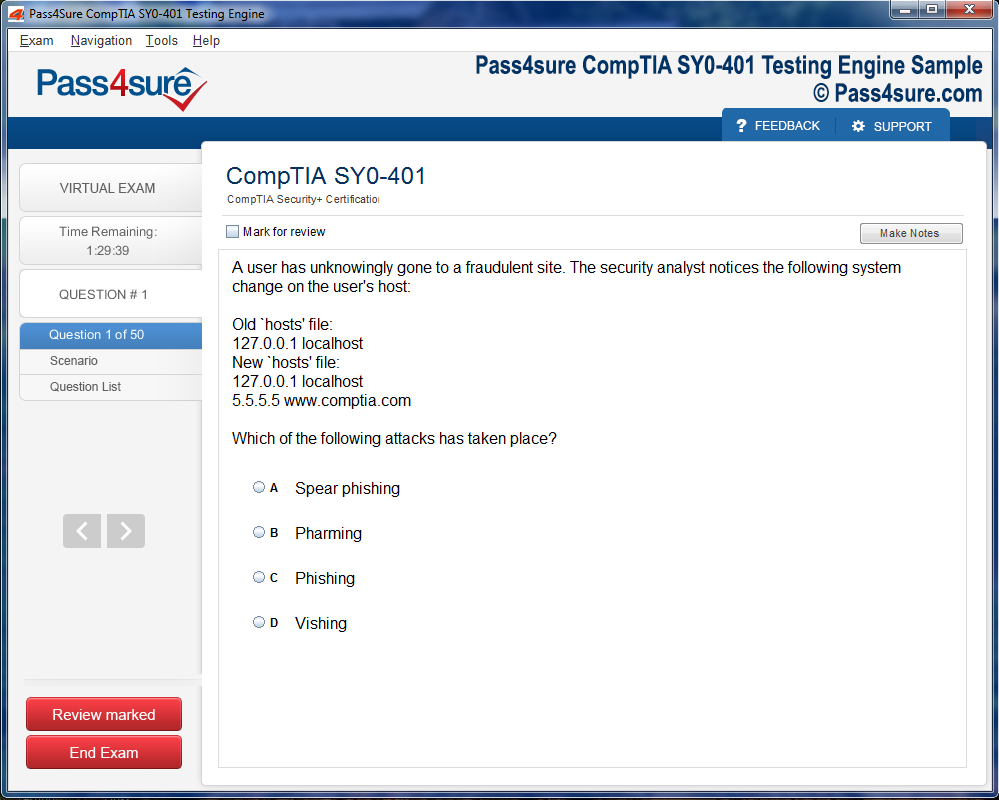
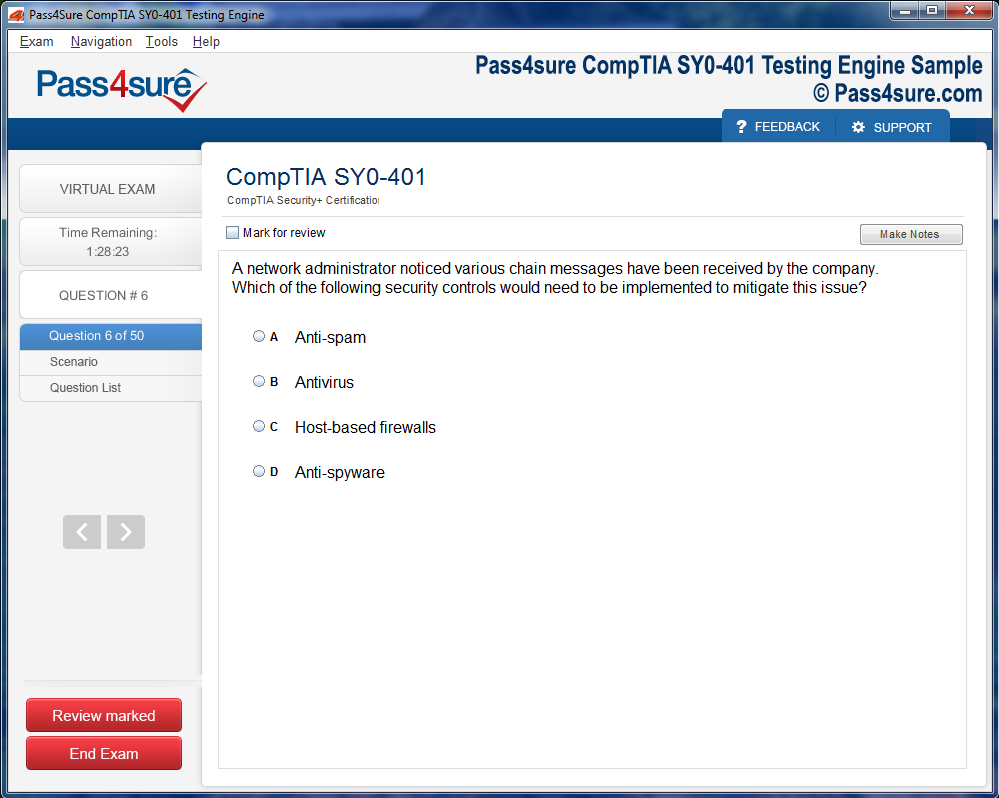
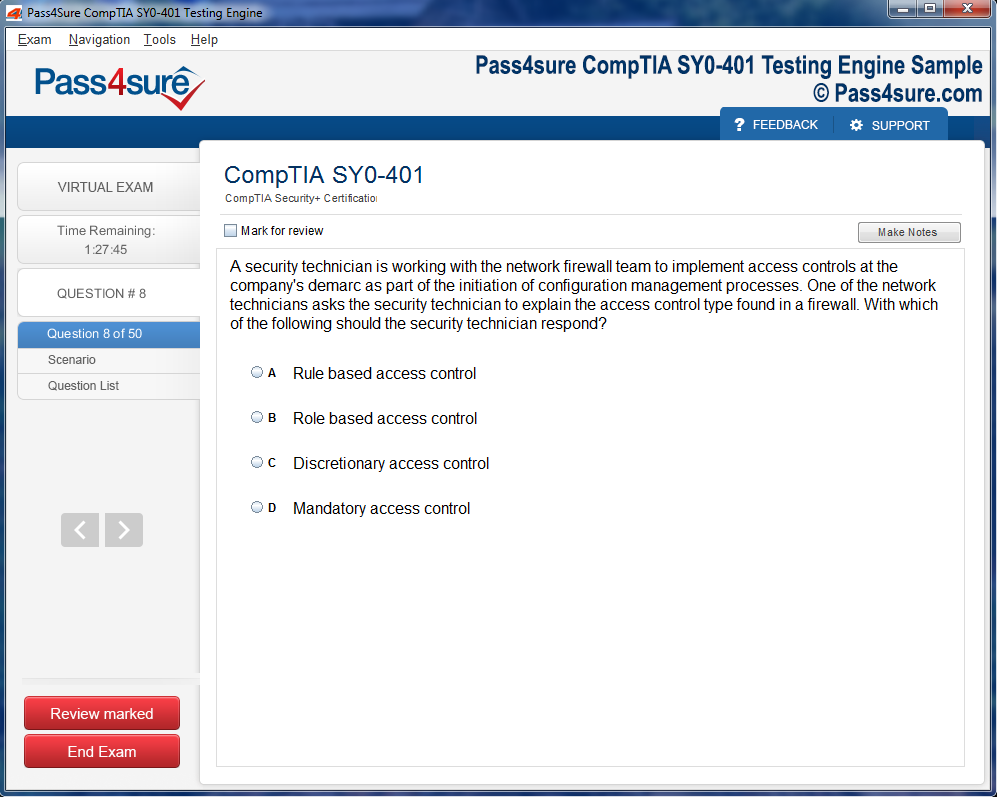
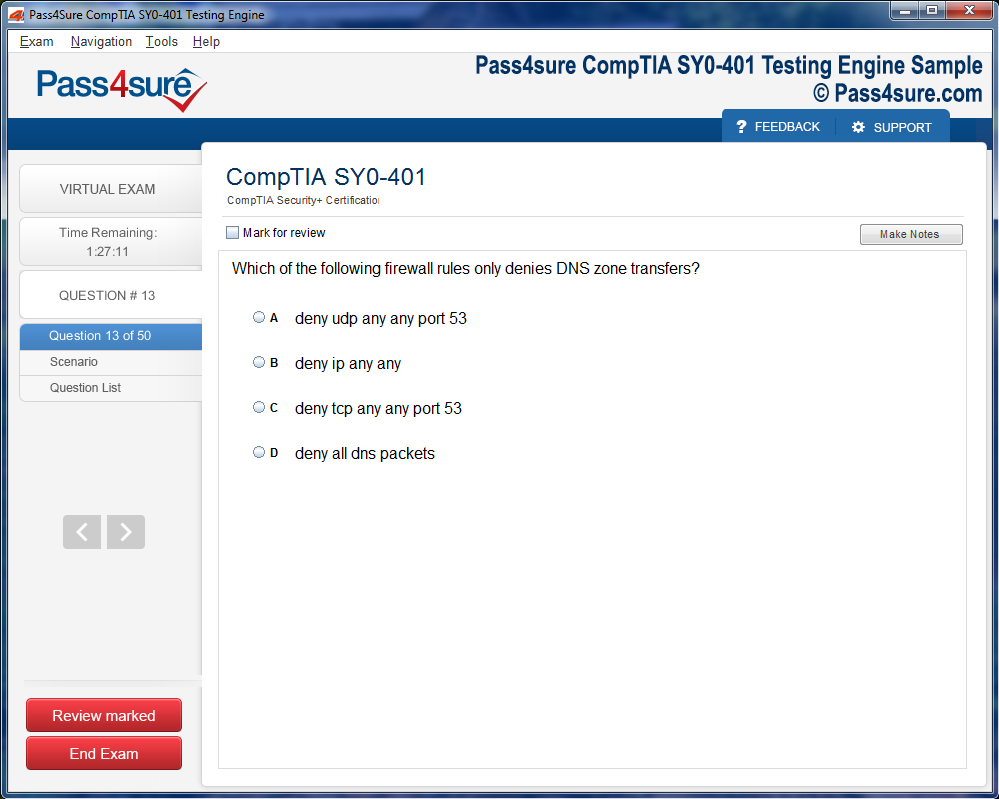
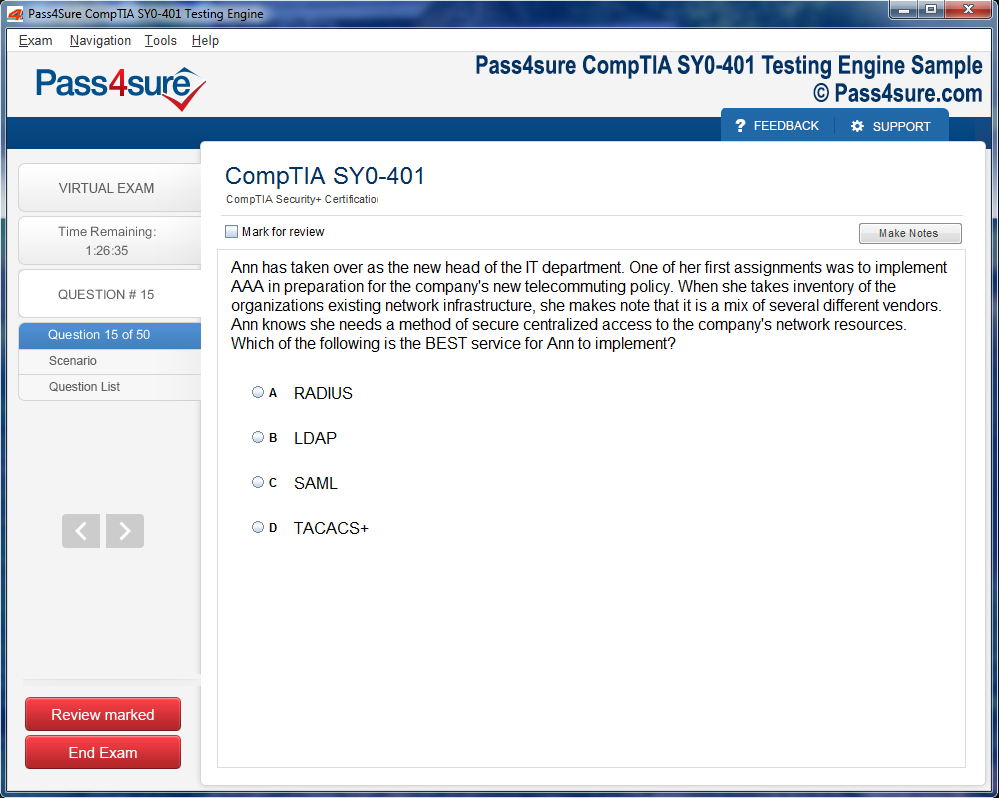
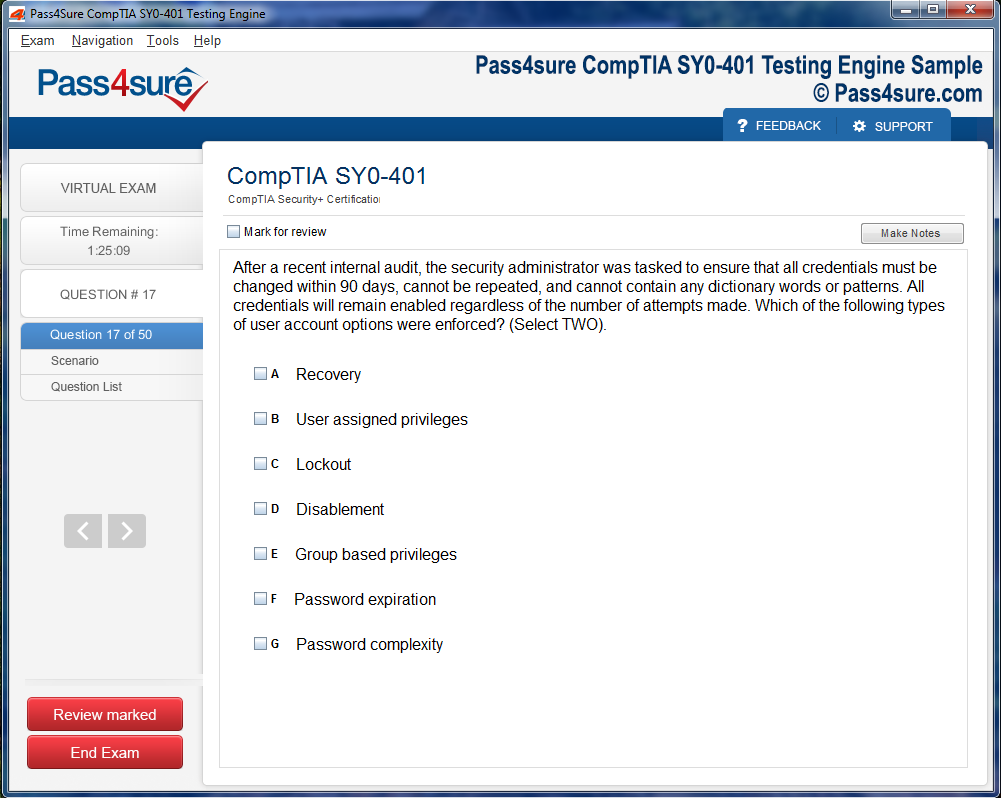
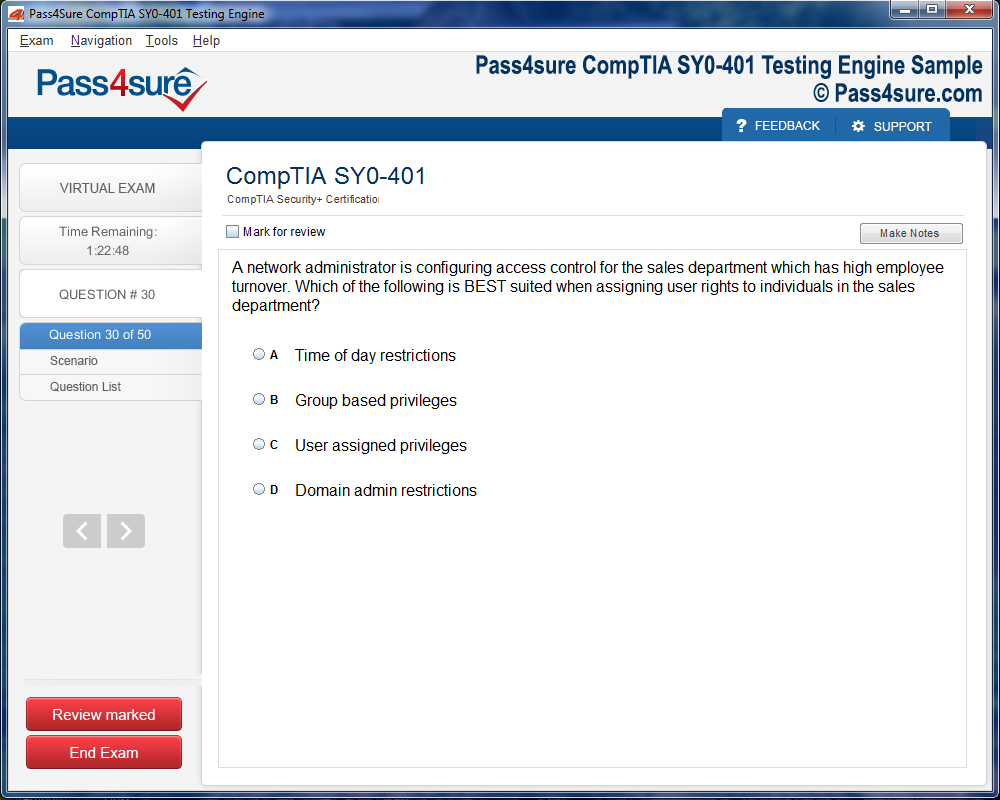
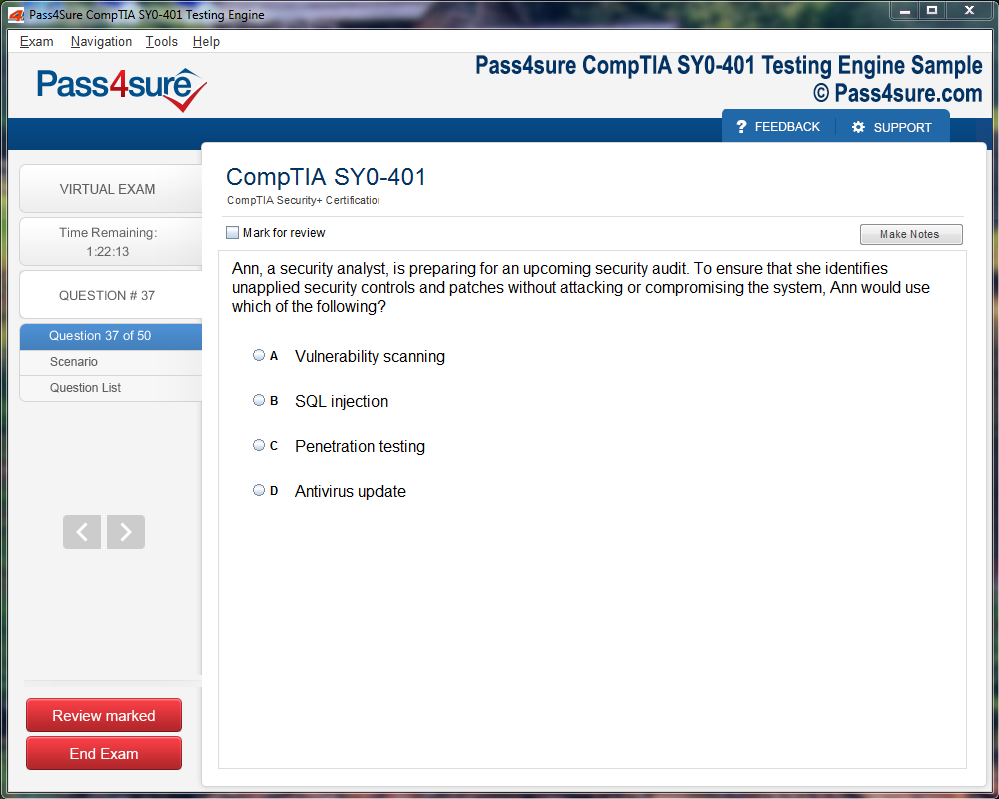
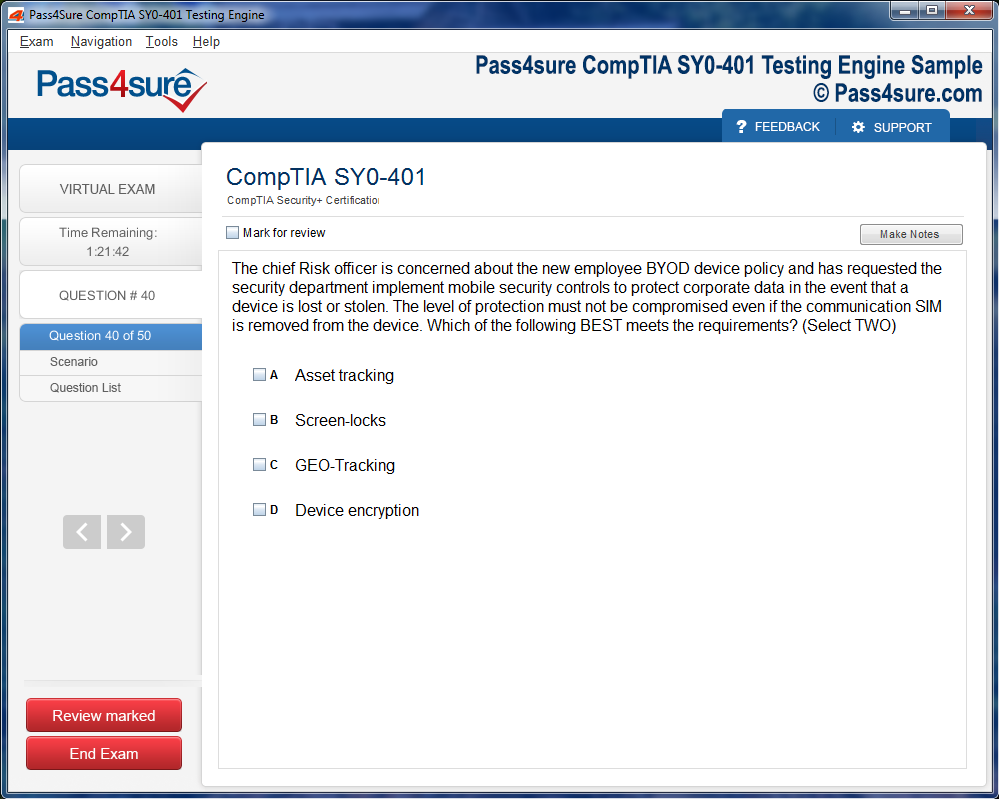
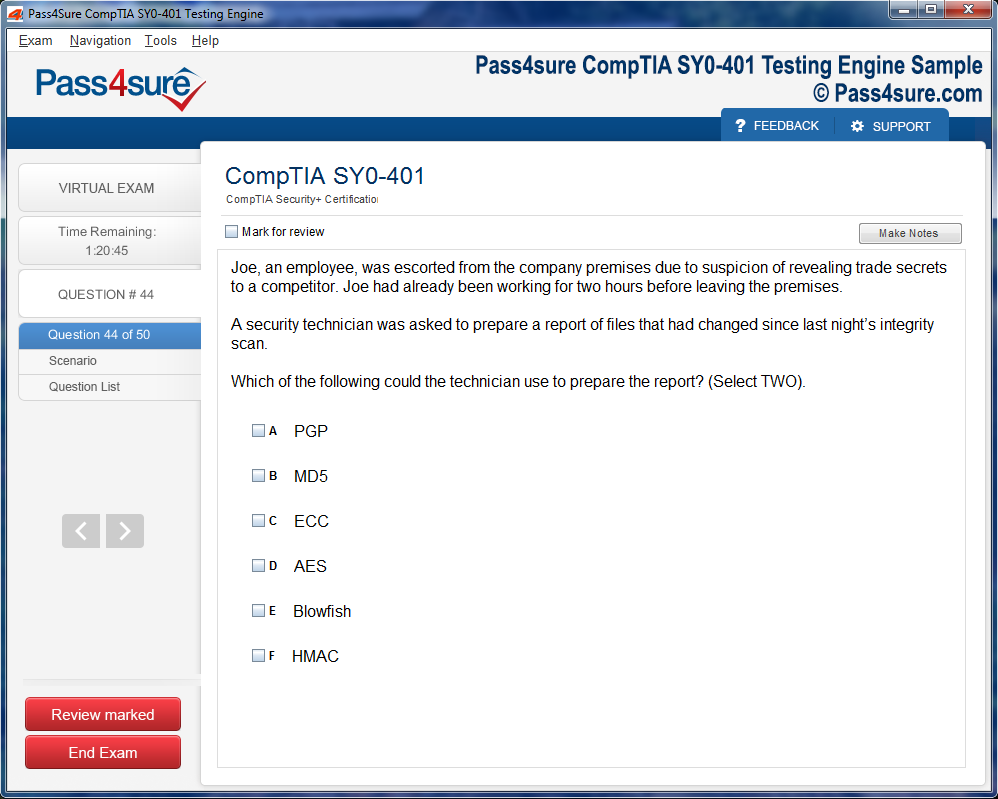
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations.
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.
AHIP AHM-530 Made Simple: Step-by-Step Preparation Guide
Healthcare is not a monolithic structure but a labyrinthine tapestry of interconnected entities. The metamorphosis of healthcare networks reflects broader societal, technological, and economic shifts. Hospitals, outpatient clinics, insurance carriers, and myriad ancillary service providers interlace to form intricate constellations that dictate patient trajectories. These networks are not merely operational constructs; they embody philosophical underpinnings regarding access, equity, and the very definition of wellness. Understanding this dynamic landscape necessitates an appreciation for the historical contingencies that have shaped contemporary healthcare delivery, including policy revolutions, demographic transitions, and emergent epidemiological challenges.
Decoding the Architecture of Healthcare Delivery Systems
Healthcare delivery systems function as multifaceted ecosystems, where interdependence and specialization converge. Public institutions coexist alongside private enterprises, each operating under unique fiscal schemas that influence service provision. The interplay of reimbursement models, from capitation to fee-for-service, shapes both provider behavior and patient experience. Within these systems, subtle variations in governance and administration can yield profound differences in efficiency, patient satisfaction, and clinical outcomes. Professionals engaging with these structures must cultivate a granular understanding of organizational architecture, stakeholder incentives, and the interstitial dynamics that underpin care continuity.
Navigating Managed Care Paradigms
The domain of managed care presents a spectrum of operational philosophies, each balancing cost containment with quality imperatives. Health Maintenance Organizations prioritize preventive interventions, incentivizing longitudinal patient engagement while constraining expenditures. Preferred Provider Organizations, by contrast, offer a liberalized provider selection framework, often incurring elevated costs but enhancing patient autonomy. Point-of-Service plans endeavor to synthesize these paradigms, enabling moderated flexibility without forsaking cost efficiency. Mastery of these models is indispensable for professionals seeking to optimize network design, contractual arrangements, and patient navigation pathways, ensuring that care delivery remains both economically viable and clinically robust.
Regulatory Underpinnings in Healthcare Networks
The legal architecture governing healthcare networks is both complex and evolving. Federal mandates, such as HIPAA and the ACA, establish foundational requirements for privacy, coverage, and operational transparency. Yet, state-level statutes frequently impose idiosyncratic obligations, introducing additional layers of compliance complexity. Network managers must demonstrate an acuity for deciphering regulatory nuance, preemptively mitigating risk while preserving operational fluidity. This regulatory literacy is not merely bureaucratic; it informs quality assurance, patient safety protocols, and ethical stewardship, anchoring network functionality within a legally defensible and morally coherent framework.
The Pivotal Role of Healthcare Analytics
In contemporary network management, data is both compass and map. Claims adjudication, demographic profiling, utilization analysis, and outcome metrics converge to illuminate the contours of care delivery. Analytical proficiency enables network managers to detect latent inefficiencies, anticipate patient demand, and stratify risk across populations. Sophisticated visualization techniques and predictive algorithms empower decision-makers to allocate resources judiciously, tailor interventions, and enhance overall system responsiveness. Beyond operational optimization, analytics undergird strategic foresight, enabling network architects to anticipate emergent health trends, regulatory shifts, and technological disruptions.
Strategic Integration of Stakeholder Perspectives
Healthcare networks are sustained through delicate negotiation among diverse stakeholders. Clinicians, administrators, insurers, and patients each bring unique perspectives, priorities, and constraints. Effective network management necessitates the orchestration of these voices into a coherent operational symphony. Transparent communication channels, equitable incentive structures, and participatory decision-making processes foster collaborative environments conducive to innovation and continuous improvement. By cultivating relational dexterity, professionals can harmonize stakeholder objectives, mitigate conflicts, and enhance both provider satisfaction and patient experience, creating resilient networks capable of withstanding systemic shocks.
Optimizing Patient Access and Continuity of Care
A paramount objective of network management is ensuring seamless patient access across the continuum of care. Fragmentation of services often results in inefficiencies, duplicative procedures, and adverse clinical outcomes. Network strategists employ methods such as care coordination frameworks, patient navigation programs, and integrated electronic health records to bridge these gaps. Attention to sociocultural determinants, geographic distribution, and socioeconomic barriers further refines access optimization. By embedding patient-centric principles into network design, managers can cultivate continuity, reduce avoidable hospitalizations, and enhance longitudinal health trajectories.
Financial Stewardship and Cost Containment
Sustainable network operation requires meticulous financial stewardship. Capitation contracts, bundled payments, and risk-sharing arrangements serve as instruments for balancing cost containment with quality imperatives. Network managers must possess both quantitative acumen and strategic foresight, leveraging fiscal data to anticipate resource constraints and identify high-impact interventions. Econometric modeling and sensitivity analyses inform budget allocation, while scenario planning mitigates vulnerability to policy shifts, market fluctuations, and emergent public health crises. Financial prudence is thus inseparable from clinical efficacy, forming the substrate upon which resilient networks are constructed.
Quality Improvement and Performance Metrics
The pursuit of excellence in healthcare networks is inseparable from rigorous quality improvement initiatives. Metrics spanning patient satisfaction, readmission rates, clinical outcomes, and process efficiency provide critical feedback loops. Continuous performance monitoring enables iterative refinement, promoting adaptive strategies in response to emergent challenges. Incorporation of evidence-based best practices, sentinel event analyses, and benchmarking against peer institutions fosters an ethos of accountability and continuous learning. Network managers who excel in this domain translate data insights into actionable interventions, ensuring that patient care is both safe and efficacious.
Leveraging Technology for Network Efficacy
Technological innovation has become an indispensable fulcrum for network efficiency. Electronic health records, telehealth platforms, predictive analytics engines, and AI-driven diagnostic tools enhance both operational agility and patient engagement. Integration of interoperable systems reduces redundancy, streamlines workflows, and supports informed clinical decision-making. Moreover, technology facilitates proactive population health management, enabling targeted interventions that preempt disease exacerbation. Network leaders must therefore maintain fluency in emerging digital solutions, balancing implementation costs with potential clinical and operational dividends.
Risk Management and Contingency Planning
Healthcare networks operate under perpetual uncertainty, from epidemiological volatility to regulatory flux. Risk management frameworks, encompassing both clinical and financial dimensions, are essential for safeguarding network integrity. Predictive modeling, scenario simulations, and contingency protocols empower leaders to preempt adverse events, maintain continuity of care, and protect fiscal solvency. Embedding resilience within organizational culture ensures adaptive capacity, enabling networks to respond rapidly to crises, whether natural disasters, cyber threats, or public health emergencies.
Human Capital and Workforce Optimization
The effectiveness of healthcare networks is inextricably linked to workforce proficiency. Recruitment, retention, and professional development strategies shape organizational capability and morale. Interdisciplinary collaboration, competency-based training, and leadership cultivation foster a workforce equipped to navigate complex care landscapes. Attention to occupational well-being, burnout mitigation, and role satisfaction enhances productivity and sustains high-quality care. Network managers who prioritize human capital cultivate an engaged, resilient, and adaptive workforce, ensuring operational continuity and superior patient outcomes.
Ethical Considerations in Network Governance
Ethical stewardship underpins every dimension of network management. Balancing cost constraints with equitable access, patient autonomy with population-level priorities, and innovation with risk mitigation requires nuanced judgment. Ethical frameworks guide decision-making, informing policies on resource allocation, clinical trial participation, data privacy, and end-of-life care. Professionals attuned to moral imperatives navigate dilemmas with integrity, fostering trust among stakeholders and reinforcing the social contract that legitimizes healthcare networks.
Cultivating Leadership and Strategic Vision
Network management transcends operational competence; it demands visionary leadership. Articulating a strategic vision, aligning stakeholders with organizational goals, and championing transformative initiatives are critical for sustaining competitive advantage. Adaptive leadership fosters innovation, resilience, and responsiveness to evolving healthcare paradigms. By cultivating foresight, emotional intelligence, and persuasive communication, leaders orchestrate complex systems, inspire collective effort, and embed a culture of continuous improvement.
Preparing for AHM-530 Network Management Certification
Success in professional certification, such as AHM-530, is contingent upon both theoretical mastery and applied insight. Candidates must internalize the interplay between regulatory frameworks, care delivery models, analytics, financial stewardship, and ethical considerations. Practice with case studies, simulation exercises, and data interpretation challenges enhances cognitive agility, enabling candidates to translate conceptual knowledge into operational decision-making. Holistic preparation ensures readiness not only for examination performance but for real-world application in dynamic healthcare ecosystems.
The Symbiosis of Innovation and Tradition
Healthcare networks thrive at the nexus of innovation and tradition. While emergent technologies and contemporary management strategies offer novel avenues for efficiency, traditional clinical wisdom, interpersonal rapport, and historical insight remain indispensable. Effective network management synthesizes these dimensions, harmonizing evidence-based interventions with contextual awareness, fostering care models that are simultaneously cutting-edge and patient-centered.
Global Perspectives and Comparative Analysis
Examining healthcare networks through a global lens elucidates diverse operational philosophies and policy architectures. Comparative analysis highlights best practices, pitfalls, and context-specific adaptations, enriching domestic network management strategies. Understanding international models of universal coverage, private-public partnerships, and decentralized governance informs evidence-based innovation and encourages cross-pollination of ideas. Global awareness cultivates adaptive thinking, enabling professionals to navigate both local and transnational challenges.
Continuous Learning and Professional Development
In a landscape characterized by perpetual change, continuous learning is imperative. Participation in professional forums, engagement with academic literature, and mastery of emerging analytic methodologies ensure sustained competence. Reflective practice, mentorship, and experiential learning further enhance expertise, enabling professionals to anticipate trends, integrate novel approaches, and maintain relevance within the field. Lifelong intellectual engagement is therefore both a personal imperative and a professional necessity.
Synthesizing Knowledge for Impact
Effective healthcare network management demands synthesis of diverse competencies: strategic vision, regulatory literacy, financial acumen, ethical discernment, technological fluency, and analytic rigor. Professionals who cultivate these capacities navigate complexity with dexterity, optimize patient outcomes, and foster resilient, adaptable networks. Mastery of these domains, coupled with continuous professional development, positions candidates not merely to succeed in certification but to drive transformative impact in healthcare delivery, ensuring networks that are efficient, equitable, and enduring.
Conceptual Foundations of Healthcare Networks
Healthcare networks are not static constructs; they are dynamic ecosystems that thrive on meticulous orchestration and strategic foresight. These networks encompass multifaceted interactions among providers, patients, insurers, and regulatory authorities, each contributing to the intricate tapestry of healthcare delivery. The foundation of network efficacy resides in discerning population health requirements and mapping them against available services. This alignment demands a sophisticated comprehension of demographic intricacies, geographic dispersion, and clinical specialties to ensure equitable access while preserving financial sustainability. Beyond mere logistics, the architecture of healthcare networks necessitates a symbiotic blend of analytical precision and imaginative foresight. Professionals navigating this landscape must anticipate emergent challenges, integrate novel technologies, and harmonize operational imperatives with patient-centric philosophies.
Strategic Network Design
Designing a healthcare network transcends conventional operational planning. It requires a confluence of quantitative analytics and qualitative intuition to construct a framework capable of withstanding both fiscal pressures and fluctuating patient demands. Essential to this process is the identification of critical service gaps, which involves rigorous data synthesis and pattern recognition. Geographic mapping, service capacity assessment, and provider availability analyses converge to inform decisions that optimize network density and distribution. Network designers must also consider contingency planning, ensuring resilience against emergent crises, including pandemics, infrastructure failures, or regulatory shifts. The resultant design is not merely a schematic of providers but a living blueprint that balances accessibility, quality, and sustainability, embodying a nuanced understanding of healthcare dynamics.
Provider Relations and Collaborative Dynamics
The vitality of healthcare networks is inextricably linked to the quality of provider relationships. Physicians, hospitals, and ancillary services function as interconnected nodes, whose collaborative efficiency directly influences patient outcomes. Cultivating robust provider relations entails proactive engagement, transparent communication, and the judicious negotiation of contractual terms. Professionals must decode the motivations and incentives of diverse stakeholders, aligning them with organizational objectives to foster synergy. Effective relationship management minimizes operational friction, enhances morale, and promotes adherence to best practices. Additionally, case analyses of successful network management illuminate the subtle equilibrium between rigidity in contractual compliance and adaptive flexibility in service delivery. The capacity to navigate this equilibrium is a hallmark of expert network managers, demonstrating both strategic acuity and interpersonal finesse.
Contractual Mastery and Negotiation
Contracts within healthcare networks serve as both governance mechanisms and instruments of operational clarity. Mastery of contractual design necessitates a granular understanding of legal frameworks, reimbursement models, and risk-sharing arrangements. Professionals must anticipate potential disputes, institute performance benchmarks, and integrate incentive structures that reward quality and efficiency. Negotiation skills are paramount; they require the ability to reconcile divergent priorities, mediate conflicts, and construct agreements that sustain long-term collaboration. The subtleties of contractual alignment extend beyond monetary considerations, encompassing ethical standards, regulatory compliance, and patient safety imperatives. By internalizing these principles, professionals cultivate networks that are both legally robust and operationally resilient.
Metrics, Monitoring, and Analytical Insight
Evaluating the performance of a healthcare network demands the establishment of sophisticated metrics that capture both qualitative and quantitative dimensions. Patient satisfaction, clinical outcomes, financial viability, and operational efficiency constitute essential indicators of network health. Implementing advanced reporting systems enables the collection of actionable data, facilitating trend analysis and proactive intervention. Analytical proficiency is critical in identifying performance anomalies, benchmarking against industry standards, and devising targeted corrective measures. Quality improvement initiatives, anchored in evidence-based methodologies, reinforce the pursuit of excellence. This data-centric approach fosters continuous learning, ensures regulatory compliance, and solidifies the credibility of network management frameworks.
Patient-Centric Orientation
Central to effective network management is an unwavering commitment to patient-centered care. Networks flourish when the design, operations, and oversight mechanisms prioritize patient experiences, outcomes, and safety. This orientation necessitates the integration of feedback loops, personalized care pathways, and proactive communication strategies. By embedding patient perspectives into decision-making processes, networks cultivate trust, enhance adherence to treatment plans, and improve population health metrics. Professionals must balance clinical imperatives with psychosocial considerations, ensuring that accessibility, cultural sensitivity, and equity remain foundational pillars. The synergy between operational efficiency and patient satisfaction is a decisive determinant of network sustainability and reputation.
Stakeholder Engagement and Multidimensional Collaboration
Healthcare networks function as ecosystems of diverse stakeholders, each wielding influence over outcomes and strategic trajectories. Engaging these actors requires adept communication, negotiation, and consensus-building. Professionals must navigate the intersecting interests of patients, providers, payers, and regulators while fostering shared accountability and cooperative problem-solving. Simulations of stakeholder interactions, including conflict resolution exercises and collaborative workshops, enhance practical competence in real-world scenarios. By cultivating stakeholder trust and alignment, networks achieve coherent governance, reduce operational discord, and accelerate the implementation of strategic initiatives. The art of engagement extends beyond formal communication, encompassing cultural intelligence, empathy, and anticipatory foresight.
Performance Optimization Through Data-Driven Interventions
Optimizing network performance is an iterative process predicated on the judicious application of data insights. Predictive analytics, risk stratification, and utilization review methodologies enable managers to anticipate demand, allocate resources efficiently, and mitigate clinical and financial risk. Interventions are most effective when informed by comprehensive analyses that integrate historical trends, demographic patterns, and epidemiological projections. Continuous monitoring, coupled with adaptive strategies, ensures that networks remain agile and responsive to emergent challenges. Data-driven approaches also reinforce transparency and accountability, allowing stakeholders to visualize impact, assess progress, and make evidence-informed decisions.
Integration of Managed Care Principles
The architecture of contemporary healthcare networks is profoundly shaped by managed care paradigms. Principles such as capitation, bundled payments, and risk-sharing arrangements influence network configuration, provider incentives, and patient pathways. Professionals must comprehend the intricate balance between cost containment and quality assurance, leveraging managed care insights to inform network design and operational policy. Mastery of these principles enables the alignment of financial stewardship with patient-centered imperatives, ensuring both economic viability and clinical excellence. Integration of managed care strategies fosters a proactive stance toward preventive care, chronic disease management, and population health optimization, creating a virtuous cycle of efficiency and effectiveness.
Regulatory Navigation and Compliance
Healthcare networks operate within a labyrinthine regulatory landscape, encompassing federal mandates, state statutes, and professional standards. Compliance is not merely a procedural requirement but a strategic necessity that safeguards operational integrity, patient safety, and organizational reputation. Professionals must interpret regulatory texts, anticipate enforcement trends, and implement robust compliance frameworks. Audits, reporting protocols, and risk assessments constitute essential mechanisms to ensure adherence. Beyond regulatory conformity, proactive engagement with policy evolution enables networks to influence emerging standards, anticipate operational impacts, and maintain competitive advantage. Competence in regulatory navigation reflects both strategic foresight and ethical stewardship.
Technological Enablement and Innovation
Advances in healthcare technology catalyze transformative improvements in network efficiency, coordination, and quality of care. Electronic health records, telemedicine platforms, predictive analytics, and interoperability solutions constitute critical enablers of modern network functionality. Professionals must not only adopt these technologies but integrate them strategically, ensuring that innovation aligns with clinical goals, patient needs, and operational imperatives. The judicious deployment of technology enhances decision-making, streamlines workflows, and facilitates data-driven interventions. Network managers must also anticipate cybersecurity challenges, safeguard sensitive information, and cultivate digital literacy among providers to maximize technological impact.
Continuous Learning and Adaptive Leadership
The dynamism of healthcare ecosystems necessitates continuous learning and adaptive leadership. Professionals must cultivate intellectual curiosity, remain abreast of clinical innovations, and anticipate shifts in population health trends. Leadership in network management involves fostering a culture of inquiry, empowering teams to implement evidence-based improvements, and embracing change as a catalyst for growth. Mentorship, professional development programs, and cross-functional collaboration reinforce these objectives, ensuring that networks evolve responsively and sustainably. Adaptive leaders balance strategic vision with operational pragmatism, navigating complexity while inspiring confidence and cohesion among stakeholders.
Risk Management and Resilience
Risk management constitutes a core pillar of effective network stewardship. Identifying, quantifying, and mitigating clinical, operational, and financial risks is essential to sustaining network viability. Contingency planning, scenario analysis, and proactive intervention frameworks enhance resilience against unpredictable disruptions. By embedding risk awareness into organizational culture, networks cultivate proactive vigilance, enhance patient safety, and protect institutional reputation. Resilient networks demonstrate flexibility, responsiveness, and capacity for rapid recovery, embodying both operational robustness and strategic foresight.
Ethical Imperatives and Professional Accountability
Ethics permeates all dimensions of network management, guiding decisions that impact patients, providers, and communities. Professionals must navigate complex moral landscapes, balancing efficiency, equity, and compassion. Transparency, informed consent, confidentiality, and equitable resource allocation constitute fundamental ethical principles that underpin network operations. Accountability mechanisms, including performance audits, peer review, and stakeholder feedback, reinforce adherence to these principles. By embedding ethical rigor into operational and strategic processes, networks cultivate trust, enhance legitimacy, and ensure that organizational success is consonant with societal expectations.
Strategic Foresight and Long-Term Planning
Sustaining healthcare networks demands a forward-looking orientation that anticipates demographic shifts, technological innovations, and policy evolution. Strategic foresight involves scenario planning, horizon scanning, and the identification of emerging risks and opportunities. Long-term planning encompasses resource allocation, capacity development, and alignment of organizational vision with community health needs. Professionals equipped with these capabilities navigate uncertainty with confidence, ensuring that networks remain relevant, resilient, and responsive to evolving healthcare landscapes. Strategic foresight fosters proactive adaptation, positioning networks to seize opportunities while mitigating potential threats.
The Intersection of Theory and Practice
Healthcare network management thrives at the nexus of theoretical knowledge and practical application. Professionals must translate conceptual insights into actionable strategies, bridging the gap between academic understanding and operational reality. This translation requires analytical rigor, innovative problem-solving, and meticulous implementation planning. By integrating principles of network design, provider engagement, performance evaluation, regulatory compliance, and stakeholder collaboration, managers cultivate comprehensive, high-functioning networks. The iterative refinement of practice, informed by reflective learning and empirical evidence, reinforces effectiveness and enhances both patient outcomes and organizational sustainability.
Cultivating Leadership Competence
Leadership competence in healthcare network management encompasses strategic vision, operational acumen, and relational intelligence. Professionals must inspire collective effort, mediate conflicts, and align diverse stakeholders toward shared objectives. Leadership extends beyond directive functions to encompass mentorship, capacity-building, and the promotion of a collaborative culture. Competent leaders balance innovation with stability, guiding networks through periods of transformation while safeguarding core values. By exemplifying ethical stewardship, evidence-informed decision-making, and adaptive resilience, leaders foster high-performance networks capable of delivering superior patient care and sustainable operational results.
Future Trajectories in Network Management
The trajectory of healthcare networks is shaped by technological advancements, demographic evolution, and policy innovation. Emerging trends, including precision medicine, value-based care, and integrated delivery systems, redefine network expectations and operational paradigms. Professionals must anticipate these shifts, cultivating agility, foresight, and innovation capacity. The successful network manager navigates complexity with strategic insight, leveraging emerging tools and practices to optimize performance. By embracing continuous evolution, networks achieve sustainability, excellence, and relevance, ensuring that the delivery of care remains both effective and equitable across diverse populations.
Healthcare networks, as living entities, demand strategic vision, analytical rigor, and relational dexterity. Effective management integrates network design, provider engagement, performance optimization, stakeholder collaboration, regulatory compliance, technological enablement, ethical stewardship, and adaptive leadership. Professionals equipped with these competencies navigate the intricacies of healthcare systems with confidence, enhancing patient outcomes, operational efficiency, and organizational resilience. Continuous learning, foresight, and ethical accountability reinforce the enduring vitality of healthcare networks, ensuring their capacity to adapt, thrive, and sustain high-quality care in a rapidly evolving landscape.
The Primacy of Data in Healthcare Networks
Data serves as the quintessential lifeblood within contemporary healthcare networks, underpinning every operational and strategic decision. Its salience transcends mere record-keeping, transforming into an analytical catalyst that informs the orchestration of care delivery. Healthcare professionals must engage with diverse datasets, ranging from claims data and electronic health records to patient-reported outcomes and operational metrics, to distill actionable intelligence. The interpretive process necessitates a discerning eye capable of recognizing subtle patterns and anomalies that could influence patient outcomes or operational efficacy. Mastery of these analytical skills is pivotal for candidates navigating the intricacies of the AHM-530 Network Management exam, where scenario-based questions frequently demand nuanced comprehension of multifaceted data constructs.
Discerning Patterns Through Analytical Acumen
The analytical endeavor within healthcare networks extends beyond mere tabulation; it requires the cultivation of cognitive dexterity to extract meaning from complex datasets. Professionals must identify latent trends, correlations, and deviations that may elude superficial observation. Such insights facilitate strategic interventions, whether in augmenting provider performance, optimizing resource allocation, or addressing care delivery inefficiencies. The synthesis of these analytical discoveries forms a cognitive lattice upon which informed decisions are scaffolded, empowering network managers to anticipate challenges rather than merely react. Candidates preparing for the AHM-530 examination must internalize these methodologies, as the ability to extrapolate from nuanced datasets is often a differentiating factor in both examination performance and practical efficacy.
The Convergence of Risk Management and Data Analysis
Risk management within healthcare networks is inextricably intertwined with meticulous data analysis. Identification of potential vulnerabilities, whether financial, operational, or clinical, necessitates a proactive stance informed by empirical evidence. Network managers must leverage predictive models and trend analyses to preemptively address areas of concern, mitigating the likelihood of adverse outcomes. Such interventions may encompass recalibration of provider contracts, strategic reconfiguration of service delivery pathways, or the implementation of robust quality improvement initiatives. A sophisticated understanding of these interdependencies enables professionals to approach network management holistically, a competency that is rigorously assessed in the AHM-530 examination framework.
Harnessing Technology for Network Optimization
Technology represents an unparalleled enabler within healthcare networks, facilitating real-time access to critical information and expediting decision-making processes. Electronic health records, telemedicine platforms, and population health management systems constitute pivotal tools that transform the accessibility and utility of data. Network managers must adeptly integrate these technologies to enhance care coordination, monitor performance metrics, and ensure compliance with evolving regulatory mandates. Mastery of digital tools not only undergirds operational efficiency but also mirrors the technologically immersive scenarios frequently encountered in the AHM-530 assessment, where candidates are challenged to apply theoretical knowledge within pragmatic, digitally mediated contexts.
Data-Driven Risk Mitigation Strategies
The operational efficacy of healthcare networks is contingent upon the symbiosis of data analysis and risk mitigation. By interrogating historical performance metrics, network managers can identify patterns indicative of potential vulnerabilities. These insights inform strategic interventions designed to curtail financial exposure, optimize patient safety, and bolster service reliability. For instance, recalibrating contract structures or redesigning patient flow processes may alleviate bottlenecks and reduce systemic inefficiencies. An advanced comprehension of these interrelations ensures that candidates can navigate the complex interplay of risk and performance, a competency integral to both AHM-530 success and the operational stewardship of healthcare networks.
Collaborative Dynamics in Healthcare Network Management
Healthcare network management is inherently collaborative, necessitating the integration of diverse expertise across clinical, administrative, and strategic domains. Professionals must translate analytical insights and technological capabilities into actionable strategies through cohesive teamwork. Interdisciplinary collaboration ensures that improvement initiatives are not only conceptually sound but operationally viable, harmonizing the contributions of clinicians, administrators, and external stakeholders. Candidates preparing for the AHM-530 exam benefit from cultivating scenario-based experiences that simulate these collaborative dynamics, enhancing their capacity to orchestrate complex projects and communicate effectively within multifaceted organizational structures.
Strategic Application of Predictive Analytics
Predictive analytics occupies a central role in the proactive management of healthcare networks. By leveraging historical data and sophisticated modeling techniques, professionals can forecast trends in patient utilization, resource allocation, and clinical outcomes. These projections enable network managers to anticipate emergent challenges, implement preemptive interventions, and optimize system efficiency. The ability to translate predictive insights into tangible operational strategies is both a hallmark of effective network management and a critical competency evaluated in the AHM-530 examination. Candidates must develop fluency in interpreting predictive outputs, ensuring that analytical insights are not merely theoretical but operationally actionable.
Enhancing Patient Outcomes Through Informed Decision-Making
At its core, healthcare network management revolves around the enhancement of patient outcomes. Data analysis, risk assessment, and technological integration converge to create a decision-making ecosystem that prioritizes quality, safety, and accessibility of care. Network managers must continuously evaluate performance metrics, monitor provider adherence to best practices, and implement targeted interventions that address care gaps. The iterative refinement of these processes ensures that network operations remain agile and responsive to evolving patient needs. Candidates for the AHM-530 exam must internalize this patient-centered ethos, recognizing that operational proficiency is inextricably linked to the improvement of clinical outcomes.
Regulatory Acumen and Compliance Management
Navigating the regulatory landscape constitutes an indispensable component of healthcare network management. Professionals must possess a nuanced understanding of federal, state, and local mandates, ensuring that network operations align with statutory and accreditation requirements. Compliance management is intricately connected to data stewardship, risk mitigation, and technological deployment, creating a multidimensional framework within which network managers operate. Candidates preparing for the AHM-530 examination must cultivate an awareness of regulatory imperatives, appreciating the subtleties of compliance as both a legal obligation and a strategic instrument for safeguarding organizational integrity.
Operational Efficiency Through Resource Optimization
Resource optimization lies at the heart of effective network management, requiring a meticulous balance between fiscal stewardship and service quality. Data-driven insights inform decisions regarding staffing, facility utilization, and supply chain management, enabling network managers to maximize operational efficacy. By identifying redundancies, forecasting demand, and aligning resources with strategic priorities, professionals ensure that networks operate at peak efficiency while maintaining high standards of patient care. Mastery of these operational principles is essential for candidates navigating the AHM-530 examination, where scenario-based questions frequently challenge the application of resource optimization strategies.
The Integration of Continuous Quality Improvement
Continuous quality improvement constitutes a perpetual imperative within healthcare networks, fostering an ethos of iterative enhancement and organizational learning. Network managers must deploy data analytics, stakeholder feedback, and performance metrics to identify opportunities for refinement across clinical, operational, and administrative domains. Initiatives may include process redesign, staff training programs, or technological enhancements, each contributing to a holistic elevation of network performance. For candidates pursuing AHM-530 certification, proficiency in continuous quality improvement principles demonstrates both conceptual understanding and practical readiness for real-world network stewardship.
Cultivating Interdisciplinary Communication Skills
Effective network management necessitates adept communication across diverse professional spheres. Clinicians, administrators, and external partners each contribute unique perspectives and expertise, requiring network managers to translate complex data and strategic imperatives into accessible, actionable guidance. Scenario-based exercises that simulate stakeholder interactions provide candidates with practical experience in negotiation, presentation, and collaborative problem-solving. These skills are critical not only for AHM-530 examination success but for the real-world orchestration of interdisciplinary initiatives that drive network performance and patient-centered care.
Leveraging Population Health Management
Population health management represents a paradigm shift in healthcare, emphasizing proactive, community-centered strategies over reactive, episodic interventions. Network managers must utilize data analytics, predictive modeling, and technological platforms to monitor population trends, stratify risk, and implement targeted interventions. By anticipating population needs and allocating resources strategically, professionals can reduce preventable morbidity, optimize healthcare utilization, and enhance system-wide efficiency. Candidates for the AHM-530 exam benefit from understanding the nexus between population health strategies and network management, as this knowledge underpins scenario-based questions requiring integrated, systemic thinking.
Strategic Leadership in Healthcare Networks
Leadership within healthcare networks entails more than administrative oversight; it encompasses vision-setting, change management, and strategic orchestration of complex systems. Network managers must harmonize data analytics, technological adoption, risk mitigation, and collaborative processes to achieve sustainable improvements. Strategic leadership requires foresight, adaptability, and the ability to galvanize interdisciplinary teams around shared objectives. Candidates preparing for the AHM-530 examination should cultivate these leadership competencies through scenario-based exercises and reflective practice, ensuring that they are prepared to navigate both exam challenges and the multifaceted demands of professional network management.
Synthesizing Knowledge Across Domains
Success in network management demands the synthesis of knowledge across multiple domains, including healthcare delivery systems, managed care models, regulatory frameworks, data analytics, risk management, technological integration, and stakeholder engagement. Candidates must demonstrate the capacity to connect discrete areas of expertise into cohesive strategies that drive operational and clinical excellence. The AHM-530 examination tests this integrative capability, requiring candidates to apply theoretical knowledge to practical, real-world scenarios. Mastery of domain synthesis not only facilitates certification success but also positions professionals to exert meaningful influence within the evolving landscape of healthcare networks.
Future Directions in Network Management
The future of healthcare network management is characterized by accelerating technological innovation, heightened regulatory scrutiny, and evolving patient expectations. Network managers must remain agile, continuously updating their knowledge and skill sets to respond to emergent trends. Artificial intelligence, predictive analytics, and integrated care platforms are poised to redefine operational paradigms, demanding that professionals cultivate both technical acumen and strategic foresight. Candidates for the AHM-530 examination who anticipate these developments and incorporate them into their preparation are likely to achieve both exam success and enduring professional relevance in the dynamic healthcare ecosystem.
Ethical Stewardship in Healthcare Networks
Ethical stewardship constitutes a foundational principle in healthcare network management, guiding decisions that balance organizational objectives with patient welfare. Network managers must navigate complex moral landscapes, ensuring that data utilization, resource allocation, and care delivery practices adhere to principles of equity, transparency, and accountability. Candidates preparing for the AHM-530 exam must internalize these ethical imperatives, recognizing that effective network management is not solely a technical endeavor but also a commitment to principled, patient-centered leadership. Ethical acumen enhances credibility, fosters trust among stakeholders, and ensures that operational excellence is aligned with societal expectations.
Concluding Perspectives on Network Mastery
Mastery of healthcare network management emerges from the convergence of analytical rigor, technological proficiency, risk mitigation, collaborative skill, and ethical stewardship. Candidates who cultivate these competencies are well-positioned to navigate the complexities of modern healthcare systems, achieve AHM-530 certification, and effect tangible improvements in patient outcomes and operational efficiency. The interplay of data, technology, and human insight forms the bedrock of effective network management, empowering professionals to anticipate challenges, optimize resources, and lead interdisciplinary initiatives with confidence. In essence, the art and science of network management lie in the ability to synthesize knowledge, embrace innovation, and translate insights into impactful, sustainable practice.
The Fluid Dynamics of Healthcare Network Management
Healthcare network management is an intricate ecosystem, perpetually in flux, demanding adaptive cognition and anticipatory dexterity. The domain is neither static nor linear; rather, it oscillates between regulatory shifts, technological revolutions, and mercurial market forces. Professionals navigating this landscape must cultivate a perennial appetite for learning, leveraging workshops, symposia, and digital knowledge repositories to maintain acuity. This continuous edification ensures proficiency in the pillars of network design, quality optimization, and multifaceted stakeholder engagement, aligning theoretical acumen with operational pragmatism.
Regulatory Oscillations and Compliance Paradigms
The regulatory framework governing healthcare networks is labyrinthine, with statutory nuances varying across jurisdictions and temporal contexts. Compliance is an iterative process, requiring professionals to decode convoluted mandates and embed them seamlessly within operational workflows. Vigilance is essential to forestall sanctions and enhance systemic integrity. Mastery of this terrain entails an understanding of licensure stipulations, accreditation protocols, and reporting imperatives, necessitating a mindset attuned to both precision and foresight.
Technological Inflection Points and Digital Integration
Technological innovation operates as a centrifugal force in healthcare management, catalyzing efficiency yet complicating legacy systems. Network managers must navigate electronic health records, telemedicine platforms, predictive analytics, and cybersecurity imperatives with alacrity. Assimilation of these tools is not merely technical but strategic, as each integration reshapes patient flow, data interoperability, and resource allocation. Continuous immersion in digital fluency elevates managerial proficiency, enabling agile responses to emergent clinical and administrative exigencies.
Financial Acumen as a Strategic Lever
Financial literacy constitutes a sine qua non of network stewardship. Beyond mere arithmetic, it encompasses an intricate understanding of reimbursement schemas, capitation models, bundled payments, and cost-containment stratagems. Professionals must scrutinize the fiscal implications of clinical decisions, negotiate provider contracts with perspicacity, and implement operational efficiencies without compromising care quality. Analytical dexterity in interpreting balance sheets, cash flow statements, and variance reports transforms financial knowledge into actionable insight, fortifying network sustainability.
Patient-Centric Network Architecture
The zenith of healthcare network management is the orchestration of patient-centered care. Networks must be designed to facilitate seamless access, continuity, and optimal outcomes while integrating patient feedback, clinical metrics, and operational intelligence. This holistic orientation requires balancing individualized care imperatives with systemic efficiency, ensuring regulatory compliance and resource stewardship. Thoughtful alignment of care pathways, referral mechanisms, and outcome monitoring fosters networks that deliver tangible value and measurable satisfaction.
Interdisciplinary Collaboration and Stakeholder Synergy
Effective network management thrives on the confluence of diverse expertise. Stakeholders encompass physicians, payers, administrators, patients, and ancillary service providers, each with distinct incentives and priorities. Cultivating synergetic collaboration necessitates nuanced negotiation, conflict resolution, and empathetic communication. Managers must architect forums for dialogue, establish consensus-building frameworks, and reconcile competing interests without compromising organizational integrity. The dexterity to harmonize these interactions is a hallmark of superior leadership in healthcare networks.
Data-Driven Decision-Making and Analytical Rigor
Decision-making in contemporary network management is increasingly predicated on empirical evidence. Leveraging big data, predictive modeling, and performance dashboards allows managers to anticipate trends, optimize resource allocation, and mitigate operational bottlenecks. Analytical rigor extends beyond mere statistical interpretation; it encompasses pattern recognition, scenario planning, and probabilistic reasoning. Professionals adept in these competencies transform raw data into strategic insights, enhancing both clinical efficacy and organizational resilience.
Quality Improvement and Continuous Optimization
Quality assurance is an iterative journey rather than a discrete endpoint. Network managers are tasked with implementing continuous improvement frameworks, auditing clinical outcomes, and embedding corrective actions into systemic workflows. Methodologies such as Lean, Six Sigma, and Plan-Do-Study-Act cycles provide structured mechanisms for elevating performance while reducing inefficiencies. Mastery of these paradigms requires both conceptual understanding and practical dexterity, ensuring that networks evolve in response to emerging evidence and stakeholder feedback.
Leadership Archetypes and Organizational Influence
Leadership within healthcare networks extends beyond positional authority, encompassing the ability to inspire, mentor, and galvanize teams toward shared objectives. Effective leaders exhibit cognitive empathy, strategic foresight, and adaptability in the face of uncertainty. They cultivate organizational cultures that valorize accountability, innovation, and patient-centered values. Scenario-based training, reflective practice, and mentorship can enhance leadership acuity, fostering managers who navigate complexity with poise and decisiveness.
Communication as a Strategic Imperative
Communication in network management transcends mere information exchange; it functions as a strategic conduit for alignment, motivation, and negotiation. Managers must articulate complex regulatory, clinical, and financial concepts with clarity, tailoring messaging to diverse audiences. Active listening, persuasive reasoning, and diplomatic engagement reinforce collaboration and mitigate conflict. The synthesis of verbal, non-verbal, and written communication strategies is integral to sustaining cohesive, high-functioning networks.
Scenario-Based Competency and Experiential Learning
Experiential learning, through scenario-based simulations and case analyses, augments traditional didactic approaches. Managers are tested on their ability to apply theoretical knowledge in dynamic, often ambiguous contexts. This pedagogy fosters adaptive thinking, ethical reasoning, and operational dexterity. Engaging in these exercises cultivates confidence, enabling professionals to navigate real-world challenges with both rigor and creativity, bridging the gap between academic preparation and practical execution.
Ethical Stewardship and Moral Imperatives
Ethics are inextricable from network management, as decisions reverberate through patient lives, organizational culture, and societal trust. Ethical stewardship demands adherence to principles of beneficence, justice, and transparency, particularly when resource constraints or conflicting interests arise. Managers must reconcile competing imperatives, balancing financial sustainability with equitable access and clinical quality. Cultivating moral discernment and integrity fortifies both individual credibility and systemic legitimacy.
Innovation Ecosystems and Strategic Foresight
Innovation is a pivotal vector in sustaining competitive and clinically robust networks. Managers must anticipate emerging technologies, care delivery models, and policy shifts, cultivating an anticipatory stance that preempts disruption. Strategic foresight involves horizon scanning, trend extrapolation, and investment in transformative initiatives. Embedding a culture of innovation encourages experimentation, cross-pollination of ideas, and iterative refinement, fostering resilient networks capable of thriving amid uncertainty.
Integrating Clinical Insight with Operational Strategy
Healthcare network managers occupy a liminal space between clinical imperatives and operational exigencies. Integrating evidence-based medicine with resource allocation, workforce planning, and process optimization requires both domain-specific knowledge and systemic thinking. Managers translate clinical insight into actionable strategies, ensuring that care pathways are efficient, patient-centered, and compliant with regulatory standards. This integration enhances both care quality and organizational agility.
Cultivating a Learning Organization
Networks that thrive are characterized by continuous learning at both individual and organizational levels. Managers must foster environments where knowledge is disseminated, best practices are institutionalized, and errors serve as opportunities for refinement. Knowledge management systems, reflective practice, and interdepartmental learning initiatives reinforce collective competence. A learning organization is resilient, adaptable, and capable of sustaining high-quality care amid shifting landscapes.
Risk Management and Contingency Planning
Healthcare networks are inherently exposed to multifactorial risks, including clinical errors, financial volatility, and regulatory noncompliance. Effective managers implement robust risk management frameworks, encompassing hazard identification, mitigation strategies, and contingency protocols. Scenario planning, stress testing, and crisis simulations ensure preparedness, enabling networks to respond to exigencies with agility and composure. Proactive risk stewardship preserves both patient safety and organizational continuity.
Cultural Competency and Inclusive Practices
Diversity and cultural sensitivity are essential to optimizing network operations and patient satisfaction. Managers must recognize and accommodate linguistic, socioeconomic, and cultural variances, embedding inclusivity into policies, protocols, and care pathways. Culturally competent leadership enhances patient trust, staff engagement, and system efficacy. It also strengthens compliance with equity mandates and supports the ethical imperative of providing universally accessible, high-quality care.
Sustainability and Resource Optimization
Sustainability is increasingly central to network management, encompassing environmental, financial, and operational dimensions. Managers must optimize resource utilization, minimize waste, and integrate eco-conscious practices into procurement, logistics, and care delivery. Fiscal prudence and environmental stewardship are mutually reinforcing, ensuring long-term viability and social responsibility. Strategic planning that incorporates sustainability principles fortifies networks against future challenges.
Evaluating Performance Metrics and Outcomes
Performance evaluation is multidimensional, encompassing clinical outcomes, operational efficiency, financial performance, and patient satisfaction. Managers employ both quantitative and qualitative metrics, utilizing dashboards, benchmarking, and key performance indicators to track progress and inform decision-making. Continuous evaluation fosters accountability, drives improvement initiatives, and validates strategic investments, reinforcing the network’s capacity to deliver high-value care.
Harmonizing Innovation with Regulatory Adherence
Balancing cutting-edge innovation with stringent regulatory adherence is a delicate endeavor. Managers must navigate the tension between experimental interventions and compliance mandates, ensuring patient safety while embracing transformative potential. Structured governance, iterative piloting, and stakeholder engagement mitigate risk, enabling networks to integrate novel approaches responsibly. This equilibrium enhances reputation, mitigates liability, and fosters a culture of measured innovation.
Strategic Networking and Professional Alliances
The cultivation of professional networks amplifies managerial effectiveness, offering access to emergent knowledge, collaborative opportunities, and peer mentorship. Strategic alliances with academic institutions, professional associations, and industry consortia facilitate continuous learning and resource sharing. Networking extends beyond information exchange, fostering symbiotic relationships that enhance operational insight, leadership capacity, and strategic influence.
The Multidimensional Competence Imperative
Excellence in healthcare network management is inherently multidimensional, requiring harmonization of regulatory acumen, technological proficiency, financial literacy, patient-centered design, and leadership dexterity. Competence emerges from deliberate practice, reflective learning, and scenario-based application, bridging theoretical knowledge with operational execution. Professionals who cultivate this integrative expertise are poised to navigate the complexity of modern healthcare networks, delivering value, quality, and sustainability while demonstrating resilience amid perpetual change.
The Intricacies of Network Management Certification
The odyssey toward achieving certification in network management transcends rote memorization, demanding a synthesis of cognitive dexterity, analytical acumen, and pragmatic application. The AHM-530 Network Management exam epitomizes this holistic approach, requiring candidates to navigate the labyrinthine corridors of healthcare IT infrastructure, regulatory frameworks, and performance optimization. Mastery of this domain necessitates an immersive engagement with scenarios that mimic the volatility and intricacy of real-world networks, where decision-making carries immediate and tangible consequences.
Immersive Learning Environments
Interactive pedagogical environments serve as crucibles for honing expertise. Simulation-based exercises allow aspirants to grapple with network anomalies, troubleshoot cascading failures, and recalibrate systems dynamically. This experiential learning cultivates reflexive thinking, enabling candidates to anticipate complications, evaluate multifactorial outcomes, and implement corrective measures with precision. Such environments emulate the open-book ethos of the AHM-530 examination, emphasizing the ability to extract, interpret, and deploy information adeptly rather than relying solely on memorized doctrines.
The Power of Collaborative Networks
Engagement with mentors and peers is pivotal in crystallizing conceptual understanding. Knowledge exchanges through case studies, discussion forums, and cooperative projects expose candidates to eclectic problem-solving paradigms. This collective intellectual scaffolding fosters meta-cognition, encouraging learners to scrutinize assumptions, juxtapose methodologies, and extrapolate lessons from diverse operational contexts. Through these synergies, candidates cultivate a nuanced comprehension of network dynamics, fortifying their capability to respond judiciously to complex exam scenarios.
Case Studies as Cognitive Catalysts
Delving into empirical case studies elucidates the interplay between theoretical constructs and pragmatic exigencies. Analyzing documented network failures, performance bottlenecks, or regulatory breaches imparts invaluable insights into causality, mitigation strategies, and contingency planning. Candidates learn to discern subtle patterns, identify latent risks, and formulate robust solutions, thereby internalizing a repertoire of strategies that extend beyond exam preparation to tangible professional efficacy.
Time Management and Cognitive Economy
The temporal parameters of the AHM-530 exam, with 100 multiple-choice queries condensed into a two-hour window, necessitate strategic time management. Candidates must cultivate cognitive economy, parsing questions rapidly, prioritizing complex items, and deploying knowledge efficiently. Practicing under simulated timed conditions attenuates performance anxiety, accelerates information retrieval, and enhances decision-making acuity. Familiarity with canonical reference texts further amplifies efficiency, allowing swift corroboration of answers while conserving precious cognitive bandwidth.
Analytical Prowess and Strategic Acumen
The examination evaluates not only factual recall but also analytical prowess and strategic discernment. Candidates must interpret multifaceted scenarios, synthesize cross-domain information, and devise optimal interventions. This entails a sophisticated understanding of healthcare delivery systems, managed care paradigms, and regulatory landscapes. Equally essential is the capacity to analyze performance metrics, optimize network design, and ensure system resilience. Cultivating these competencies fosters a strategic mindset, positioning candidates to navigate both exam challenges and professional exigencies with poise.
Simulation and Practice as Pedagogical Pillars
Repeated exposure to digital test simulations engenders familiarity with question typologies and enhances tactical responses. Simulated assessments provide immediate feedback, highlighting knowledge gaps and reinforcing retention through iterative practice. Such experiential cycles emulate real-world network troubleshooting, wherein iterative testing, monitoring, and adjustment are indispensable. By internalizing these practices, candidates fortify their operational dexterity, bridging the chasm between theoretical comprehension and applied expertise.
Regulatory Literacy and Compliance Competence
A sophisticated grasp of regulatory imperatives is indispensable in network management within healthcare contexts. Candidates must navigate complex statutes, accreditation standards, and data privacy protocols, integrating compliance mandates into operational workflows. This literacy ensures networks are not only functional but also legally defensible, mitigating risks associated with breaches or lapses in governance. Understanding these frameworks enhances exam performance while underscoring professional accountability in real-world network stewardship.
Data-Driven Decision Making
Proficiency in network management necessitates a fluency in data analytics. Candidates must interpret performance metrics, assess traffic flows, and evaluate system health through quantitative lenses. Data-driven insights facilitate predictive maintenance, resource allocation, and optimization of patient care delivery. Engaging with analytical tools and dashboards during preparation familiarizes aspirants with the empirical rigor required to manage intricate networks, translating statistical literacy into actionable strategy.
Network Design and Optimization Strategies
Effective network management hinges upon architectural foresight and operational dexterity. Candidates must master principles of topology, redundancy, scalability, and latency mitigation. Strategic design decisions influence system resilience, operational efficiency, and end-user satisfaction. By dissecting exemplar networks and constructing hypothetical architectures, aspirants internalize the nuances of design trade-offs, fostering a capacity to devise robust, high-performing infrastructures under both exam and professional pressures.
Performance Management and Monitoring
Sustaining network efficacy requires meticulous performance oversight. Candidates are expected to monitor throughput, detect anomalies, and implement corrective protocols. Real-time analysis, coupled with predictive algorithms, underpins proactive management, enabling preemptive interventions that avert systemic failures. Preparation through practical exercises equips candidates with an intuitive understanding of network behavior, reinforcing both analytical acuity and procedural competence.
Enhancing Cognitive Flexibility
Success in network management is predicated on adaptability and cognitive flexibility. Candidates encounter dynamically shifting variables, from emergent security threats to fluctuating patient data loads. Preparing for these contingencies cultivates resilience, encouraging mental agility and strategic foresight. By simulating variable-rich environments, aspirants learn to pivot strategies fluidly, integrate emergent information, and maintain operational equilibrium under stress.
Leadership in Network Management
Certification transcends technical proficiency, emphasizing leadership and decision-making gravitas. Candidates must orchestrate multidisciplinary teams, allocate resources judiciously, and mediate operational conflicts. Cultivating leadership acumen through mentorship, scenario exercises, and reflective practice enables professionals to exert influence effectively, drive performance, and foster a culture of accountability. Leadership competencies complement technical mastery, ensuring network managers contribute meaningfully to organizational outcomes.
Cognitive Retention Through Iterative Practice
Iterative learning reinforces retention, ensuring conceptual frameworks remain accessible under examination conditions. Repetition across diverse contexts embeds knowledge, transforming rote information into applied expertise. Candidates benefit from cyclical engagement with exercises, simulations, and case analyses, enhancing both recall speed and accuracy. This iterative approach mirrors professional practice, where continuous engagement with evolving networks consolidates skill and judgment.
Professional Recognition and Career Advancement
Passing the AHM-530 exam signals a profound mastery of network management competencies. Certified professionals are recognized for their capacity to optimize healthcare networks, improve patient outcomes, and uphold compliance standards. This credential facilitates career mobility, opening pathways to leadership roles, strategic positions, and competitive remuneration. The certification distinguishes individuals in a competitive field, signaling both technical mastery and strategic insight to prospective employers.
Integrating Theory and Practice
The confluence of theoretical understanding and practical execution defines excellence in network management. Candidates must not only comprehend abstract constructs but also translate them into actionable strategies. This synthesis enhances problem-solving efficacy, equips aspirants to navigate unanticipated challenges, and reinforces the interconnectedness of knowledge domains. Structured study programs that emphasize applied exercises bridge the gap between conceptual learning and operational competency.
Cognitive Resilience and Stress Management
Examination preparation cultivates not only technical knowledge but also psychological resilience. Candidates must navigate high-pressure scenarios, manage time constraints, and maintain composure under evaluative scrutiny. Techniques such as mindfulness, strategic pacing, and scenario rehearsal fortify resilience, reducing cognitive load and enhancing performance. By integrating stress management into preparation, aspirants ensure their analytical faculties remain sharp and decision-making remains sound.
The Role of Mentorship in Mastery
Mentorship accelerates competency development by providing experiential insights and contextual guidance. Experienced network managers offer perspectives that transcend textbook knowledge, illuminating best practices, common pitfalls, and strategic heuristics. Engaging with mentors fosters reflective learning, encourages adaptive thinking, and cultivates professional networks that persist beyond the examination horizon. This relational dimension enhances both preparedness and long-term career development.
Holistic Network Management
Excellence in network management encompasses technical, regulatory, analytical, and interpersonal dimensions. Candidates must harmonize these elements to orchestrate seamless, resilient networks that meet operational and patient-centered objectives. Holistic preparation involves cultivating proficiency across hardware and software management, data governance, compliance adherence, performance monitoring, and strategic leadership. Such multidimensional expertise positions candidates to effect tangible improvements in healthcare delivery systems.
Strategic Resource Allocation
Effective network management demands judicious allocation of resources, balancing technological capacity with human expertise. Candidates must prioritize interventions, deploy monitoring tools strategically, and optimize system throughput while minimizing latency and downtime. Engaging with simulation exercises and hypothetical scenarios hones decision-making under resource constraints, reinforcing an ability to maximize impact while mitigating operational inefficiencies.
Continuous Learning and Knowledge Evolution
The dynamic landscape of network management necessitates lifelong learning. Candidates must remain abreast of emerging technologies, evolving regulatory mandates, and innovative management frameworks. Engaging with professional literature, attending workshops, and participating in knowledge-sharing communities ensures sustained competence. Cultivating a mindset oriented toward continuous learning fortifies adaptability, ensuring certified professionals retain relevance in an ever-evolving domain.
Ethical and Patient-Centric Considerations
Network management in healthcare is intrinsically linked to ethical imperatives and patient welfare. Candidates must integrate privacy considerations, data integrity, and equitable access into operational decision-making. Ethical discernment complements technical skill, ensuring networks enhance patient outcomes while safeguarding sensitive information. By internalizing these principles during preparation, candidates align professional practice with the moral and legal responsibilities inherent in healthcare management.
Conclusion
AHM-530 certification transcends academic achievement; it constitutes a transformation of cognitive, technical, and strategic capacities. Candidates emerge equipped to navigate complexity, make informed decisions, and lead network initiatives with confidence. Mastery in this realm signifies readiness to influence healthcare delivery positively, ensuring networks remain resilient, compliant, and patient-centered. By investing in comprehensive preparation, immersive practice, and strategic mentorship, aspirants secure not only certification but the tools to shape the future of healthcare network management.