Exam Code: CDIP
Exam Name: Certified Documentation Integrity Practitioner
Certification Provider: AHIMA
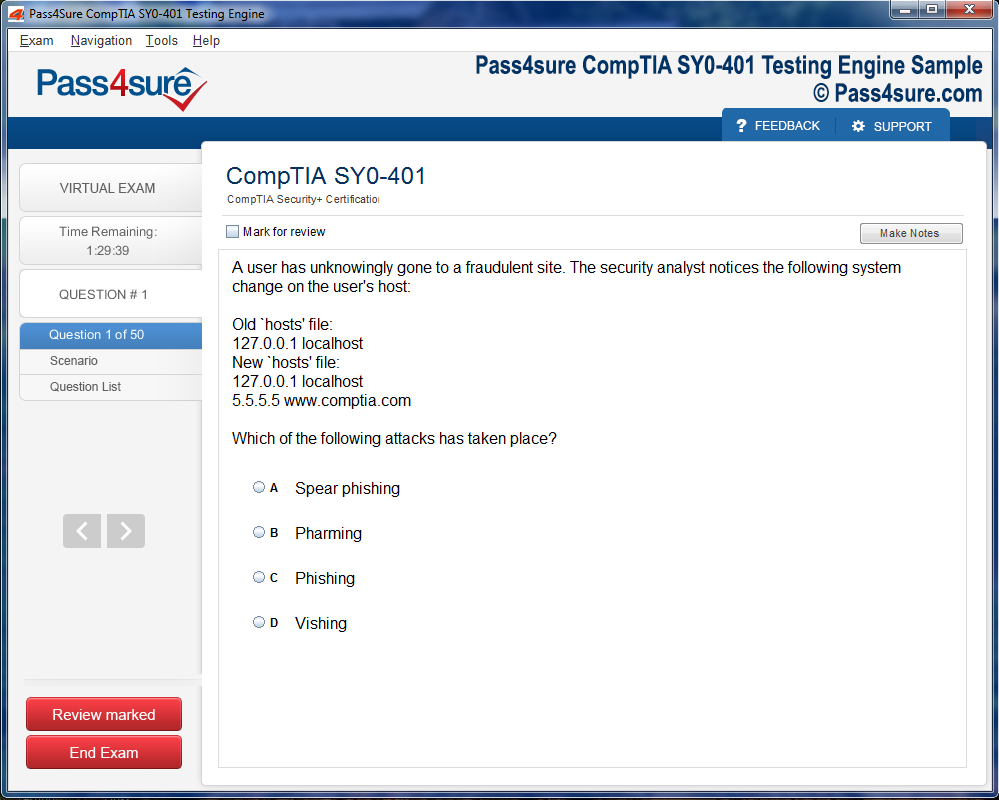
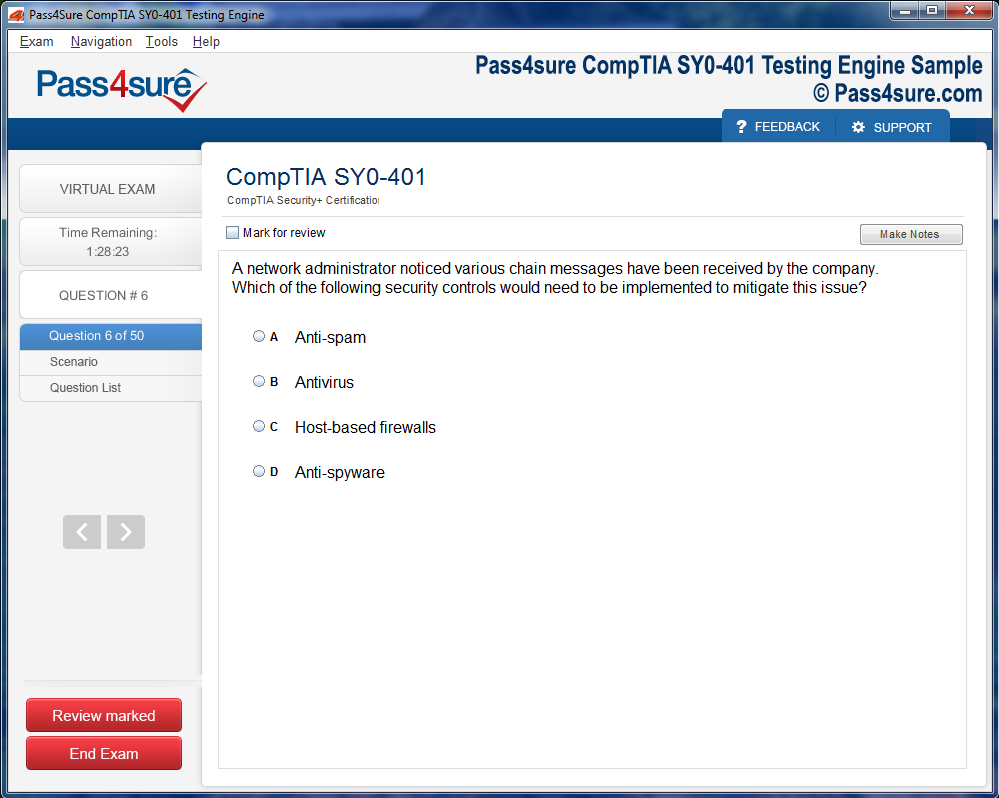
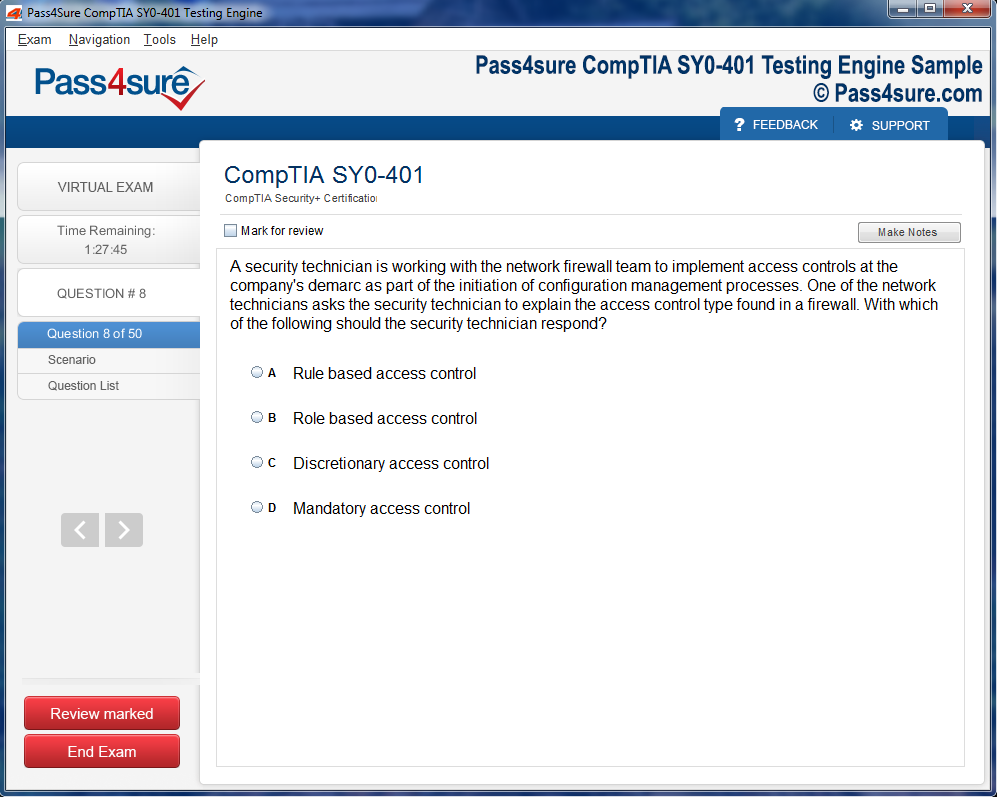
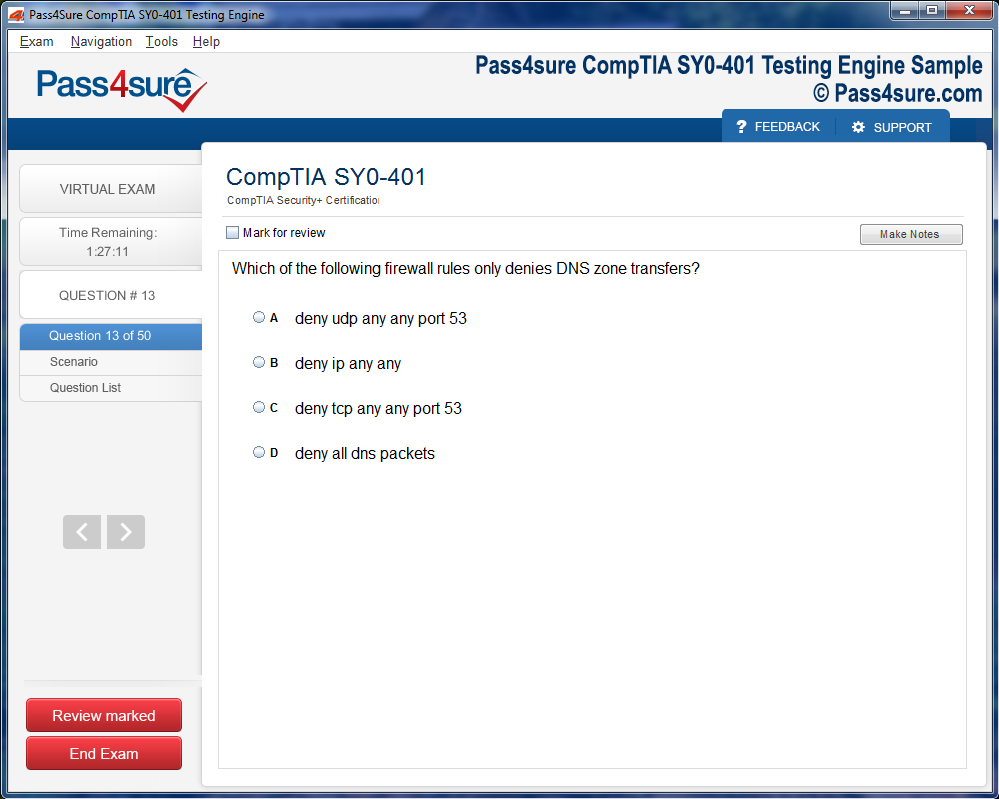
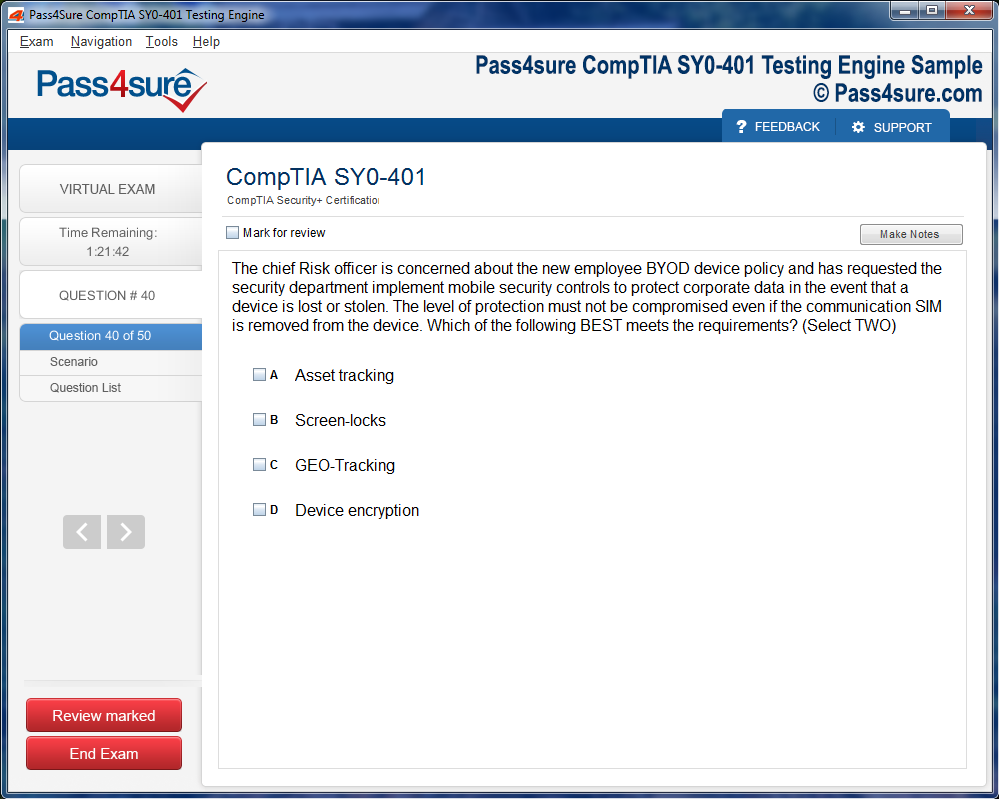
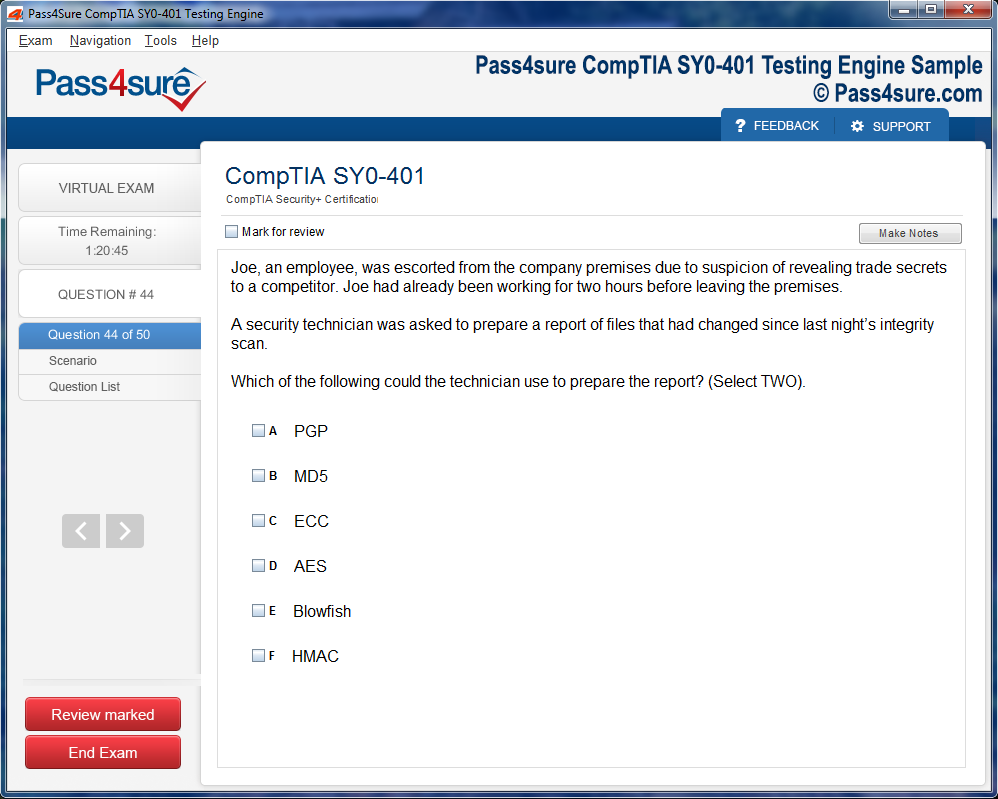
Product Screenshots
Frequently Asked Questions
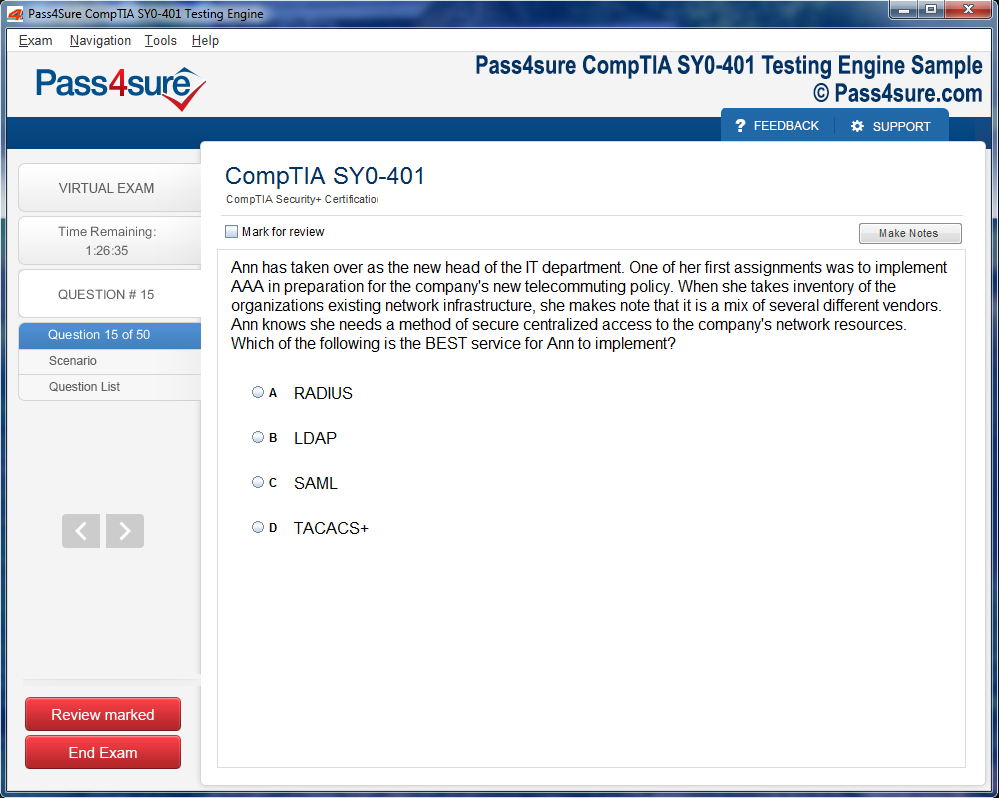
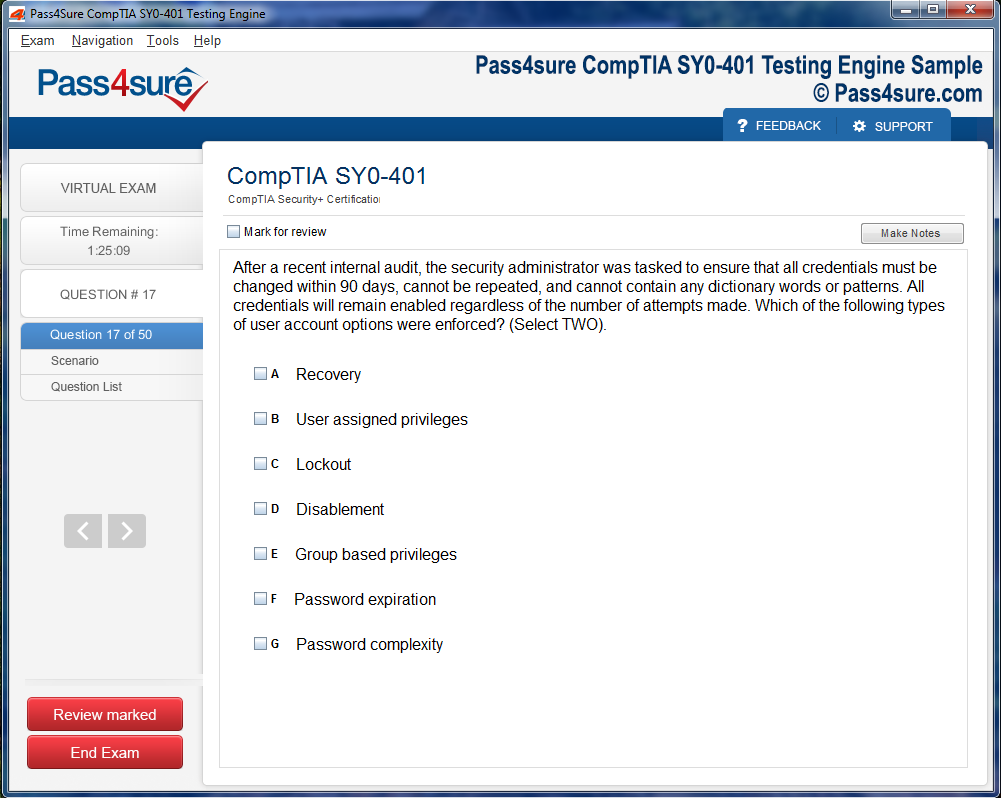
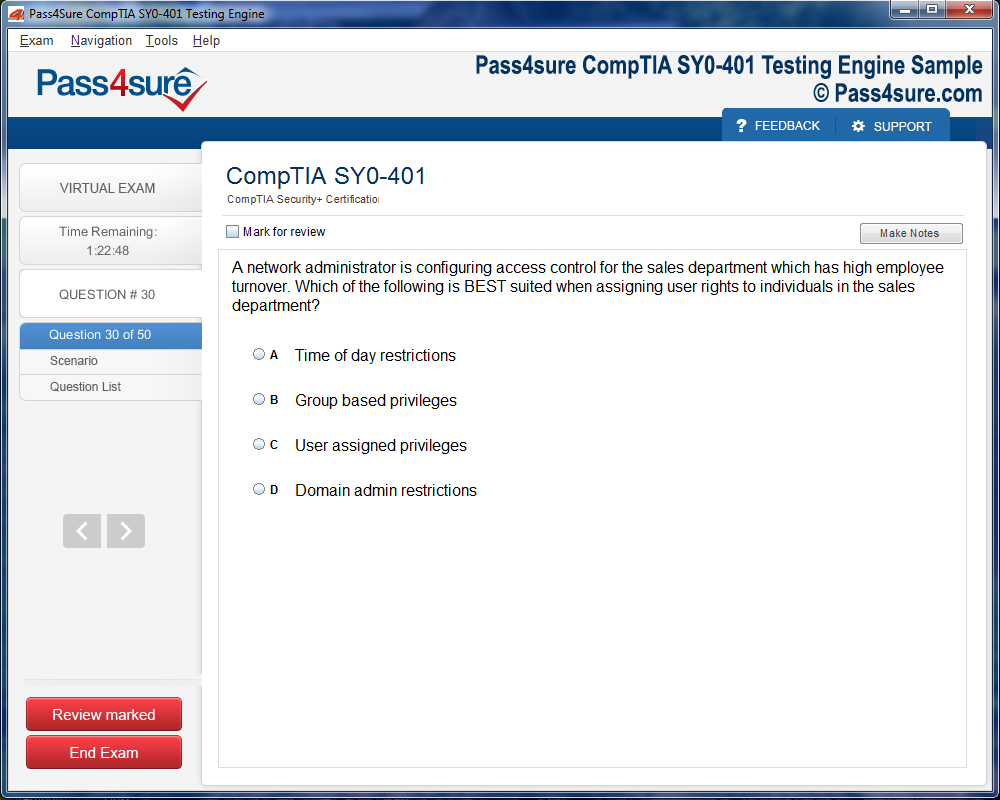
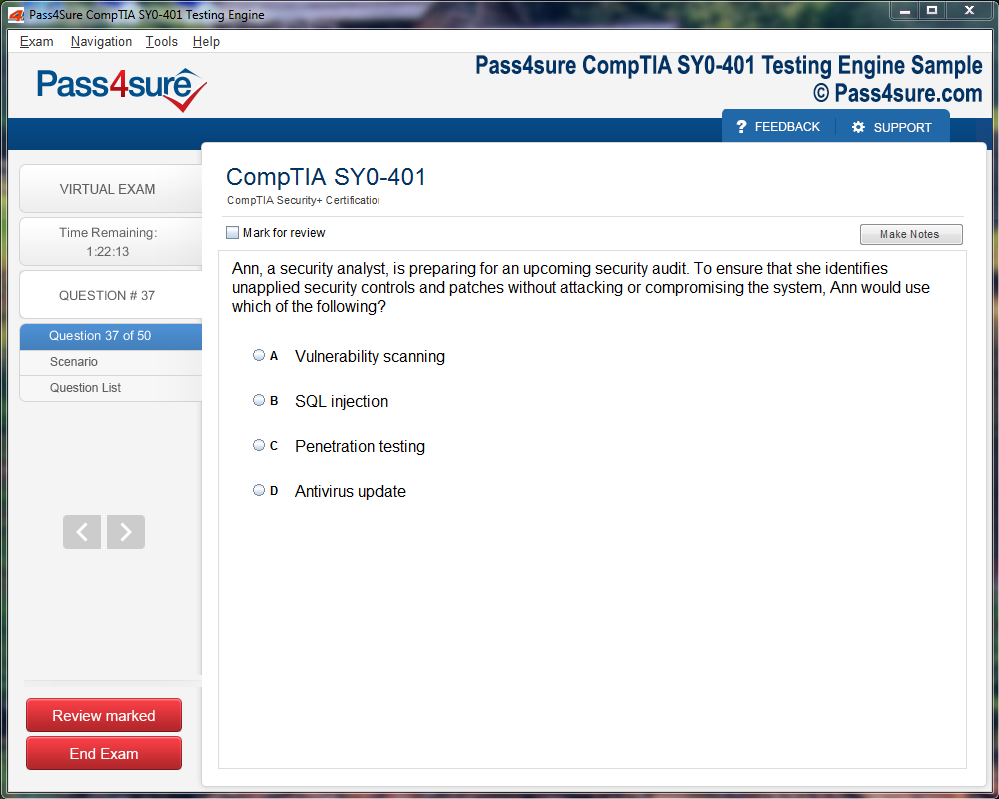
How does your testing engine works?
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations.
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.
How CDIP Certification Elevates Clinical Documentation and Coding Compliance
In the contemporary panorama of healthcare, clinical documentation has metamorphosed into more than a perfunctory administrative chore; it now embodies a linchpin in the architecture of patient safety, fiscal sustainability, and overarching care quality. Each clinical encounter begets a profusion of data—an intricate tapestry of observations, interventions, and outcomes. The fidelity of this documentation determines the degree to which healthcare institutions can both interpret and leverage patient histories, ultimately shaping therapeutic trajectories. Errors or omissions in clinical records are not merely clerical inconveniences; they can precipitate diagnostic ambiguities, compromise treatment efficacy, and engender fiscal ramifications through coding misalignments or reimbursement inaccuracies.
The regulatory landscape compounds this complexity, presenting a formidable matrix of statutory obligations. Compliance with privacy mandates such as HIPAA converges with the labyrinthine stipulations of Medicare’s Inpatient Prospective Payment System, creating an environment where documentation precision is not optional but imperative. Daily, hospitals generate monumental quantities of data—measured in petabytes—rendering even minor inaccuracies potentially consequential. Alarmingly, empirical analyses indicate that administrative inefficiencies, rather than clinical misjudgments, constitute the predominant source of documentation errors. This reality underscores the criticality of structured, auditable processes in maintaining clinical documentation integrity, thereby fortifying both the operational and care-delivery facets of healthcare institutions.
Robust documentation programs transcend mere compliance; they are instrumental in engendering organizational resilience. By cultivating clinician proficiency in nuanced documentation standards, healthcare organizations mitigate the risk of financial discrepancies and regulatory sanctions. CDIP-certified professionals exemplify the apex of this expertise, harmonizing theoretical acumen with pragmatic proficiency. They operate not solely as data stewards but as cultural catalysts, fostering environments where meticulous documentation is synonymous with clinical excellence. Through their stewardship, the chasm between administrative precision and patient-centered care narrows, producing records that are both reflective and predictive of healthcare quality.
Beyond financial and regulatory imperatives, high-caliber clinical documentation catalyzes knowledge dissemination and continuity of care. Detailed, structured records empower multidisciplinary teams to access patient histories with unerring clarity, facilitating informed decision-making and reducing the likelihood of medical misadventures. When documentation captures subtle clinical nuances—ranging from atypical symptomology to psychosocial factors—it enables clinicians to anticipate complications and tailor interventions with granularity. This predictive capacity is amplified in longitudinal care settings, where comprehensive records inform both acute interventions and chronic disease management strategies.
Technological integration has further accentuated the role of documentation, as electronic health records (EHRs) provide both a repository and an analytic platform. Sophisticated EHRs enable real-time data capture, automated prompts for clinical guidelines, and seamless interoperability across care settings. However, technology is only as effective as the underlying documentation ethos. Systems cannot compensate for incomplete, inaccurate, or ambiguously recorded information. Hence, the cultivation of a documentation-conscious workforce remains paramount, ensuring that technological tools augment rather than supplant clinical judgment.
The interrelationship between documentation and revenue integrity is equally profound. Accurate documentation underpins coding accuracy, which in turn dictates reimbursement levels. Inadequate records can precipitate underpayments, delayed claims, and audits, undermining financial viability. Conversely, precise, comprehensive documentation safeguards revenue streams, ensuring that institutions are compensated in alignment with the services rendered. Beyond fiscal implications, documentation quality influences public reporting metrics and institutional reputation, which are increasingly tied to patient choice and competitive positioning within healthcare markets.
From a clinical perspective, documentation is the narrative spine of patient care. It chronicles the trajectory of disease, the rationale for interventions, and the response to therapy. This narrative continuity is crucial not only for immediate care decisions but also for post-treatment evaluation and research. Aggregated, high-fidelity documentation provides a substrate for outcomes research, quality improvement initiatives, and the development of predictive analytics. In essence, the rigor of clinical documentation reverberates far beyond the bedside, informing the evolution of evidence-based medicine.
Human factors remain a significant determinant in documentation quality. Clinician workload, cognitive fatigue, and varying levels of documentation literacy all influence the completeness and accuracy of records. Addressing these human factors requires targeted training, workflow optimization, and a cultural shift that elevates documentation from a bureaucratic obligation to an intrinsic component of professional responsibility. Institutions that prioritize documentation education and mentorship observe measurable improvements in both data quality and clinical outcomes, demonstrating that investment in human capital is as consequential as technological infrastructure.
Moreover, documentation serves a medico-legal function, providing a verifiable record of care in scenarios of dispute or litigation. Comprehensive, contemporaneous records offer protection to both patients and providers, ensuring that clinical decisions are transparent and defensible. This dual protective role reinforces the notion that documentation integrity is not ancillary but foundational to professional accountability.
The pursuit of excellence in clinical documentation also intersects with patient engagement. Transparent, well-maintained records facilitate communication with patients, empowering them to participate actively in their care. When patients have access to accurate and comprehensible documentation, they are better positioned to adhere to treatment plans, report changes in condition, and make informed decisions regarding their health trajectory. Thus, documentation serves not only the administrative and clinical imperatives but also the ethical imperative of patient autonomy.
In summation, clinical documentation has evolved into a multifaceted linchpin of modern healthcare, encompassing regulatory compliance, financial stewardship, patient safety, and knowledge propagation. Its impact is pervasive, influencing organizational resilience, clinical decision-making, and patient engagement. By fostering expertise in documentation practices, healthcare institutions can bridge the perennial gap between administrative exactitude and therapeutic excellence, ensuring that every patient encounter is recorded with precision, integrity, and foresight. Investment in clinical documentation proficiency is therefore not merely a strategic initiative; it is an ethical imperative that underwrites the very quality and sustainability of contemporary healthcare systems.
The Emergence of CDIP Certification in Healthcare Paradigms
The Certified Documentation Integrity Practitioner credential has evolved into a fulcrum for healthcare operational excellence, transcending mere professional recognition. It epitomizes an individual's adroitness in navigating the labyrinthine intricacies of clinical documentation, which is foundational to revenue integrity, regulatory compliance, and quality patient care. Possessing a CDIP certification signals an elevated capacity to synthesize multifarious clinical data, decipher nuanced physician narratives, and harmonize codified information with payer mandates. Consequently, healthcare organizations that integrate CDIP-certified practitioners into their operational framework often experience augmented accuracy in documentation, a reduction in compliance vulnerabilities, and enhanced revenue streams.
Core Competencies and Cognitive Rigor in CDIP Certification
Achieving CDIP certification necessitates mastery across multiple domains, ranging from clinical coding acumen to the subtleties of federal regulatory adherence. Candidates are evaluated on their capacity to navigate semantic ambiguities in medical records, reconcile discordant entries, and institute systematic strategies for data integrity enhancement. Eligibility is predicated upon both scholastic attainment and experiential competence, ensuring that certified individuals possess the amalgam of theoretical rigor and pragmatic insight required to thrive in complex healthcare ecosystems. The certification process itself is both exacting and multidimensional, probing candidates’ analytical reasoning, ethical judgment, and capacity for meticulous scrutiny of clinical narratives.
Fiscal Implications of Documentation Precision
The financial ramifications of exemplary documentation practices are both profound and quantifiable. Accurate clinical records enhance Case Mix Index calculations, which subsequently influence reimbursement under prospective payment systems and value-based care models. By mitigating under-coding and over-coding, CDIP-certified practitioners serve as guardians of revenue integrity, safeguarding institutions from potential financial attrition while optimizing reimbursement. Their interventions are not merely reactive but strategic, encompassing workflow redesign, documentation audits, and interdepartmental education to foster a pervasive culture of precision and accountability.
Integration of CDIP Expertise in Organizational Strategy
Embedding CDIP-certified professionals into healthcare organizational structures facilitates operational efficiency, risk mitigation, and clinical fidelity. Beyond revenue optimization, these practitioners are instrumental in orchestrating educational initiatives that elevate documentation standards across multidisciplinary teams. They act as liaisons between administrative leadership, clinical personnel, and compliance officers, translating intricate regulatory expectations into actionable operational policies. Their presence signals an organizational commitment to meticulous record-keeping, ethical practice, and continuous process improvement, thereby reinforcing both institutional credibility and patient trust.
Technological Synergy with Documentation Integrity
The confluence of technology and documentation integrity represents an emergent frontier in healthcare operations. CDIP-certified practitioners often spearhead the deployment of electronic health record enhancements, clinical decision support tools, and automated coding verification systems. By leveraging such technological adjuncts, they streamline documentation workflows, minimize human error, and generate robust, auditable datasets. This symbiosis between human expertise and digital infrastructure not only fortifies compliance frameworks but also liberates clinicians to focus on patient-centered interventions, thereby cultivating an environment where efficiency and quality coalesce.
Professional Development and Knowledge Propagation
The pursuit of CDIP certification engenders a culture of continuous learning and professional elevation. Certified practitioners frequently assume mentorship roles, disseminating specialized knowledge to coders, clinicians, and administrative staff alike. Through workshops, audits, and collaborative projects, they cultivate an organizational milieu wherein meticulous documentation is not ancillary but central to operational success. This propagation of knowledge enhances cross-functional understanding, mitigates risk exposure, and perpetuates standards that align with both regulatory expectations and patient-centered objectives.
Compliance Fortification and Regulatory Vigilance
Healthcare institutions operate within a milieu of ever-evolving regulatory scrutiny, necessitating rigorous oversight of clinical documentation. CDIP-certified professionals are pivotal in fortifying compliance structures, ensuring that documentation practices withstand external audits, payer reviews, and internal quality assessments. Their role encompasses the identification of documentation gaps, the remediation of ambiguous entries, and the promulgation of policies that codify best practices. By embedding such vigilance into routine operations, healthcare organizations not only avert financial penalties but also reinforce ethical practice and the credibility of patient records.
Clinical Quality Enhancement Through Documentation
Clinical documentation integrity is inextricably linked to patient outcomes and quality metrics. CDIP-certified practitioners influence the fidelity of clinical records, which serve as foundational evidence for performance indicators, risk stratification, and treatment efficacy assessments. By refining documentation accuracy, they enable more precise tracking of comorbidities, interventions, and patient trajectories. This precision informs clinical decision-making, augments population health analytics, and supports value-based care initiatives, thereby intertwining financial stewardship with clinical excellence.
Leadership Endorsement and Organizational Culture
The efficacy of CDIP integration is magnified when organizational leadership actively endorses documentation integrity initiatives. Administrators who prioritize certification, training, and quality audits cultivate a culture of accountability, meticulousness, and continuous improvement. Staff members operating within such environments are more likely to internalize documentation best practices, embrace technological tools, and engage in peer-led quality improvement. Leadership advocacy thus transforms documentation integrity from a procedural obligation into an intrinsic component of organizational ethos and patient-centered care.
Strategic Implications for Healthcare Management
Strategically, CDIP certification is a linchpin for holistic healthcare management, bridging the domains of operational efficiency, financial stewardship, and clinical fidelity. Institutions leveraging certified professionals' experience reduced denials, improved documentation quality, and enhanced regulatory alignment. Furthermore, CDIP practitioners facilitate cross-departmental synergy, guiding policy development, workflow optimization, and data governance initiatives. This strategic integration ensures that operational imperatives are harmonized with clinical priorities, fostering a resilient, agile, and compliant organizational infrastructure.
The Interplay of Data Integrity and Organizational Resilience
Data integrity, under the stewardship of CDIP-certified practitioners, is not merely a regulatory necessity but a strategic asset. Robust documentation supports predictive analytics, risk management, and longitudinal patient care initiatives. In the context of emergent health crises or audit scrutiny, the reliability of clinical data directly influences institutional adaptability and resilience. By maintaining stringent documentation standards, CDIP professionals enhance organizational agility, ensuring that healthcare entities can respond swiftly, ethically, and effectively to evolving operational and clinical challenges.
Future Trajectories in Documentation Excellence
As healthcare paradigms evolve, the scope of documentation integrity continues to expand, encompassing artificial intelligence-assisted coding, real-time analytics, and integrated quality monitoring. CDIP-certified practitioners are uniquely positioned to navigate these developments, translating technological innovations into practical enhancements that uphold accuracy, compliance, and operational efficacy. Their foresight and expertise ensure that documentation integrity remains a dynamic, forward-looking discipline, integral to both fiscal sustainability and the pursuit of clinical excellence.
Ethical Stewardship and Patient Advocacy
Beyond technical proficiency, CDIP-certified professionals embody ethical stewardship, safeguarding patient data, privacy, and record accuracy. By ensuring that documentation faithfully reflects clinical realities, they uphold the integrity of patient care, enhance transparency, and foster trust between patients and providers. Their commitment extends beyond regulatory compliance, representing a conscientious alignment of professional expertise with the broader imperatives of patient advocacy and healthcare equity.
CDIP Certification as a Catalyst for Holistic Healthcare Optimization
In summation, the Certified Documentation Integrity Practitioner credential transcends conventional certification paradigms, functioning as a catalyst for comprehensive healthcare optimization. Its influence permeates fiscal, operational, clinical, and ethical dimensions, driving institutions toward heightened accuracy, efficiency, and quality. By integrating CDIP-certified practitioners into strategic, technological, and educational frameworks, healthcare organizations can realize a synergistic enhancement of documentation integrity, revenue stewardship, regulatory compliance, and patient-centered excellence. The credential signifies not merely mastery of clinical documentation but a profound commitment to the meticulous, ethical, and innovative stewardship of healthcare operations.
The Symbiosis of Clinical Documentation and Coding Compliance
The labyrinthine interplay between clinical documentation and coding compliance represents a cornerstone of healthcare administration, demanding scrupulous attention to detail and systemic precision. Clinical documentation encapsulates the narrative of patient encounters, transmuting complex physiological, pharmacological, and procedural observations into written form. When this transcription is meticulously executed, it fortifies coding accuracy, ensuring that reimbursement mirrors the true intricacies of care delivery. Conversely, incomplete or equivocal records foment a cascade of interpretive errors, potentially culminating in financial repercussions or regulatory scrutiny.
The Quintessence of Documentation Accuracy
Precision in documentation is more than an administrative requisite; it constitutes a keystone of patient safety and institutional integrity. Every clinical note, whether detailing symptomatology, diagnostic trajectories, or therapeutic interventions, embodies a latent dataset critical for coding algorithms. Ambiguities or omissions engender discrepancies in code assignment, which can propagate through billing cycles, skewing financial projections and obfuscating the true burden of patient care. In this crucible of operational integrity, healthcare facilities are compelled to cultivate documentation cultures that valorize specificity, completeness, and chronological clarity.
CDIP Professionals as Translational Conduits
Certified Documentation Improvement Practitioner (CDIP) professionals serve as pivotal conduits between the clinical and administrative spheres. Their erudition in medical nomenclature, coupled with a perspicacious grasp of coding standards, allows them to translate the nuanced intricacies of patient care into codes that withstand the scrutiny of audits and regulatory evaluation. This translational proficiency mitigates the risk of compliance breaches, ensuring that remuneration reflects both the intensity and complexity of services rendered. Empirical analyses demonstrate that institutions employing CDIP-certified personnel exhibit a marked diminution in audit findings and an augmentation in revenue stability, underscoring the pragmatic dividends of investing in specialized expertise.
The Financial Ramifications of Inadequate Documentation
Financial equilibrium in healthcare is inexorably tied to documentation fidelity. Erroneous or incomplete coding precipitates underpayments or overpayments, the latter potentially incurring recoupments, fines, or reputational damage. Beyond immediate fiscal implications, flawed documentation can distort performance metrics, which increasingly inform value-based reimbursement frameworks. Consequently, the cultivation of robust documentation practices transcends clerical diligence; it becomes a strategic instrument in safeguarding institutional solvency while optimizing revenue capture.
Enhancing Patient Safety Through Documentation
Accurate and thorough documentation is indispensable to patient safety, serving as a cognitive scaffold for clinical decision-making. A meticulously chronicled patient record illuminates previous diagnoses, therapeutic regimens, and adverse event histories, reducing the likelihood of medical errors. By providing clinicians with a holistic perspective, comprehensive documentation fosters continuity of care, enabling informed interventions that are responsive to nuanced clinical presentations. In this regard, documentation functions not merely as an administrative artifact but as a sentinel of patient well-being, embodying the ethical commitment to nonmaleficence and beneficence.
Documentation as a Pillar of Value-Based Care
In contemporary healthcare ecosystems increasingly oriented toward value-based paradigms, documentation exerts a profound influence on performance evaluations and reimbursement schemas. High-fidelity records enable precise reporting of quality metrics, risk-adjusted outcomes, and care efficiency, all of which inform institutional ratings and financial incentives. Within this milieu, the interplay of documentation and coding transcends clerical exactitude, becoming an instrument of strategic advantage. Facilities adept at codifying the full spectrum of patient encounters secure favorable assessments, engender patient trust, and reinforce organizational reputability.
Ongoing Education and Compliance Vigilance
Maintaining coding compliance is an iterative endeavor, necessitating continual education and vigilant oversight. Regulatory landscapes, technological platforms, and clinical guidelines evolve at a relentless pace, rendering static policies insufficient. CDIP-certified professionals orchestrate comprehensive training initiatives, disseminating knowledge of emergent coding conventions and fostering adherence to standardized documentation practices. Through auditing, monitoring, and feedback mechanisms, these practitioners cultivate a culture of perpetual improvement, ensuring that personnel remain conversant with evolving standards and capable of sustaining institutional compliance.
The Role of Technology in Documentation Excellence
Technological integration has become an indispensable adjunct in the pursuit of documentation precision. Electronic Health Records (EHRs), natural language processing tools, and coding assistance software augment the capacity of clinicians and coders to capture, interpret, and transcribe patient data with fidelity. However, technology is not a panacea; it requires judicious implementation, ongoing training, and vigilant oversight to prevent the entrenchment of errors or inadvertent omissions. CDIP professionals function as intermediaries, aligning technological capabilities with regulatory mandates and clinical realities, ensuring that digital systems enhance rather than obfuscate documentation integrity.
Mitigating Audit Risk Through Proactive Strategies
Audit exposure represents a persistent challenge for healthcare organizations, with potential ramifications spanning financial, operational, and reputational domains. Proactive documentation strategies, championed by CDIP practitioners, constitute a bulwark against such vulnerabilities. These strategies encompass the preemptive identification of coding ambiguities, the rectification of incomplete clinical narratives, and the systematic alignment of documentation with prevailing regulatory frameworks. Institutions embracing these methodologies report diminished audit frequencies, enhanced coding accuracy, and fortified compliance postures.
Cultivating a Culture of Documentation Excellence
Sustainable documentation excellence is inextricably linked to organizational culture. Beyond procedural mandates and technological solutions, it requires an ethos in which meticulous record-keeping is valorized and reinforced. Leadership endorsement, continuous feedback loops, and interdepartmental collaboration coalesce to establish an environment where clinical and administrative personnel perceive documentation not as bureaucratic drudgery but as a professional imperative with tangible consequences. This cultural paradigm engenders higher engagement, reduces error rates, and perpetuates a virtuous cycle of compliance, financial stability, and patient safety.
Integrating Interdisciplinary Collaboration
Effective documentation and coding compliance necessitate the seamless integration of multidisciplinary insights. Clinicians, coders, compliance officers, and CDIP-certified practitioners must collaborate fluidly, ensuring that complex clinical nuances are accurately represented in coded datasets. Interdisciplinary discourse facilitates the identification of potential discrepancies, fosters consensus on ambiguous cases, and ensures that records authentically reflect the trajectory of care. This cooperative model enhances both operational efficiency and clinical fidelity, underscoring the indispensability of communication in sustaining compliance.
Documentation as a Strategic Imperative
The strategic significance of documentation extends beyond immediate compliance concerns. Detailed, precise records provide a repository of actionable intelligence that informs clinical research, operational planning, and quality improvement initiatives. Through systematic analysis of documented patient encounters, healthcare organizations can identify trends, optimize resource allocation, and implement evidence-based interventions. In this context, documentation is not merely a clerical obligation but a catalyst for institutional evolution, guiding decision-making and shaping long-term strategic trajectories.
Ethical Dimensions of Documentation
Documentation occupies a critical ethical dimension, intertwining professional accountability, transparency, and patient autonomy. Accurate recording of patient encounters safeguards against misrepresentation, supports informed consent, and ensures that therapeutic decisions are defensible and traceable. Ethical lapses in documentation—whether through omission, fabrication, or ambiguity—can erode trust, compromise patient safety, and precipitate legal ramifications. CDIP-certified practitioners reinforce ethical standards by embedding integrity, completeness, and accuracy as foundational tenets of documentation practices.
Adapting to Regulatory Flux
The regulatory environment governing healthcare documentation and coding is dynamic, characterized by frequent revisions, updates, and interpretive guidance. Compliance requires nimbleness and adaptability, demanding that personnel internalize new mandates and integrate them seamlessly into operational workflows. CDIP professionals function as navigational beacons in this fluctuating landscape, distilling complex regulations into actionable guidance, training staff in emergent standards, and auditing documentation to ensure conformity. This adaptive capacity mitigates compliance risk and sustains organizational resilience.
The Future of Documentation and Coding Synergy
As healthcare systems evolve, the synergy between documentation and coding will assume increasingly sophisticated forms. Artificial intelligence, predictive analytics, and real-time data capture will augment human oversight, enabling more granular, accurate, and efficient codification of patient encounters. Nonetheless, human expertise remains irreplaceable, particularly in interpreting nuanced clinical scenarios and contextualizing data within ethical, legal, and operational frameworks. The future, therefore, will be defined by a collaborative interplay between technological augmentation and professional acumen, anchored by the enduring principles of accuracy, compliance, and patient-centered care.
A Pillar of Sustainable Healthcare
The intersection of clinical documentation and coding compliance is foundational to the operational, financial, and ethical sustainability of healthcare organizations. Precision in documentation ensures accurate reimbursement, mitigates audit risk, enhances patient safety, and undergirds strategic initiatives. CDIP-certified practitioners, through their expertise, education, and oversight, are instrumental in translating complex clinical narratives into compliant, actionable codes. Institutions that invest in documentation excellence cultivate resilient infrastructures capable of adapting to regulatory evolution, technological advancement, and the imperatives of value-based care. Ultimately, the meticulous orchestration of documentation and coding is not merely a procedural obligation; it is a strategic, ethical, and clinical imperative that shapes the trajectory of modern healthcare delivery.
Leveraging Technology to Enhance Documentation Integrity
The burgeoning proliferation of healthcare data has precipitated a paradigm shift in clinical documentation practices, compelling institutions to embrace technology-infused solutions. In an era where voluminous patient records and multifaceted treatment pathways coexist, traditional approaches to documentation are increasingly untenable. Advanced software architectures, augmented intelligence frameworks, and automated workflow matrices are not merely adjuncts but essential instruments in the orchestration of accurate, comprehensive, and timely records. These innovations mitigate clerical encumbrances, enhance data fidelity, and liberate clinicians to concentrate on the quintessence of healthcare—patient-centric care.
The Advent of Artificial Intelligence in Clinical Records
Artificial intelligence has emerged as a fulcrum in the transformation of documentation integrity. AI-powered platforms scrutinize clinical notes with remarkable granularity, detecting anomalies, flagging inconsistencies, and proffering contextually relevant recommendations. This dual emphasis on precision and expediency revolutionizes the record-keeping landscape, ensuring that documentation transcends mere formality to become a veritable instrument of clinical insight. By leveraging natural language processing, machine learning algorithms can interpret unstructured narratives, codify medical terminology, and anticipate documentation deficiencies before they propagate downstream.
Reducing Administrative Burden Through Automation
The quotidian demands of clinical documentation have long been a source of professional fatigue and operational friction. Automation alleviates these pressures by orchestrating repetitive tasks, generating structured templates, and facilitating query resolution without continuous human intervention. By automating mundane workflows, organizations cultivate an environment where clinicians can devote intellectual bandwidth to patient engagement, complex diagnostic deliberation, and interprofessional collaboration. The resultant reduction in administrative overhead enhances not only efficiency but also professional satisfaction and retention.
Intelligent Documentation Assistants as Catalysts
Intelligent documentation assistants epitomize the confluence of technological sophistication and practical utility. These platforms serve as both sentinels and collaborators, guiding healthcare professionals through documentation protocols while preemptively identifying potential discrepancies. By offering real-time suggestions, adaptive templates, and audit-ready data, these assistants bolster compliance and reinforce accuracy. Importantly, they also serve as a buffer against cognitive overload, allowing clinicians to navigate dense medical narratives without compromising analytical rigor or patient safety.
Synergistic Effect of Certified Expertise and Technology
Clinical documentation improvement professionals (CDIPs) remain indispensable, functioning as the nexus between medical knowledge and technological facilitation. Far from being supplanted by automated systems, their expertise synergizes with AI-driven tools to elevate documentation quality. Certified professionals can leverage automated workflows to channel focus toward quality assurance, pedagogical initiatives, and anticipatory compliance measures. Organizations that cultivate this dual approach—melding certified acumen with technological prowess—report measurable gains in coding precision, operational throughput, and patient satisfaction metrics.
Enhancing Coding Accuracy Through Integration
The integration of documentation tools with coding systems represents a pivotal innovation. By synchronizing record-keeping with billing protocols, institutions can ensure immediate usability of documentation for financial and regulatory purposes. Automated coding suggestions, when guided by expert oversight, reduce errors, optimize reimbursement, and fortify audit readiness. This seamless interplay between clinical narrative and administrative coding exemplifies how technology can harmonize disparate operational domains into a coherent, error-resistant ecosystem.
Facilitating Interdepartmental Collaboration
Technological platforms also redefine interdepartmental communication by providing a shared, real-time repository of documentation. Coders, clinicians, and administrative personnel gain concurrent access to records, fostering transparency, expediting clarification, and minimizing misinterpretation. Such collaborative synergies not only accelerate workflow efficiency but also embed a culture of accountability, ensuring that each entry faithfully mirrors the care delivered. The resultant cohesion strengthens institutional integrity, enabling healthcare organizations to meet rigorous regulatory standards while advancing patient-centered objectives.
Adaptive Templates and Dynamic Workflows
Dynamic workflow design represents a critical facet of modern documentation strategy. Rather than adhering to static formats, technology permits adaptive templates that evolve with clinical context, specialty-specific requirements, and patient complexity. These templates anticipate information needs, guide narrative structure, and integrate real-time coding prompts. By embedding intelligence into routine documentation practices, institutions can achieve uniformity, completeness, and precision without stifling the nuanced judgment required in clinical decision-making.
Predictive Analytics for Proactive Compliance
Beyond record creation, technology enables predictive oversight. Analytics tools can interrogate historical data to identify recurrent deficiencies, emerging trends, or risk-prone documentation patterns. This predictive capability empowers healthcare organizations to enact preemptive corrective measures, reducing the incidence of noncompliance and enhancing overall operational resilience. By harnessing data-driven foresight, clinical teams can pivot from reactive remediation to proactive quality assurance, fostering a culture of anticipatory excellence.
Augmenting Professional Development Through Technology
Technology-driven documentation platforms serve as educational catalysts. Real-time feedback, guided templates, and analytical dashboards offer clinicians and coders opportunities for continuous learning. By illuminating areas for improvement and highlighting best practices, these tools function as personalized mentors, cultivating professional growth alongside operational efficiency. The iterative feedback loop fosters skill refinement, nurtures adherence to regulatory frameworks, and reinforces a culture of continuous improvement.
Enhancing Patient Safety and Experience
The ultimate beneficiary of technologically enhanced documentation is the patient. Accurate, real-time records facilitate clinical decision-making, minimize errors, and support seamless care transitions. Moreover, comprehensive documentation contributes to personalized care plans, ensures continuity across providers, and strengthens patient trust in the healthcare system. By reducing administrative distractions and enabling clinicians to focus on direct care, technology indirectly elevates patient experience and clinical outcomes.
Real-Time Monitoring and Feedback Mechanisms
Monitoring and feedback systems embedded within documentation platforms provide real-time visibility into compliance, accuracy, and completeness. Alerts for missing information, inconsistencies, or outdated entries guide clinicians toward timely corrections, minimizing downstream errors. These mechanisms also generate analytics that can inform policy refinement, workflow optimization, and targeted training initiatives. By creating a feedback-rich environment, healthcare organizations cultivate continuous improvement and reinforce the centrality of documentation integrity.
Streamlining Audits and Regulatory Compliance
Regulatory compliance and audit readiness are perennial challenges in healthcare administration. Technology mitigates these challenges by maintaining structured, easily retrievable records that meet rigorous standards. Automated audit trails, timestamped entries, and codified documentation pathways enhance transparency, facilitate inspections, and reduce administrative strain. By embedding compliance protocols into daily documentation practices, institutions can preempt violations, safeguard revenue streams, and reinforce public trust.
Cognitive Load Reduction for Clinicians
The cognitive burden imposed by extensive documentation has long been recognized as a factor in clinician burnout. Automated workflows, intelligent prompts, and structured templates significantly alleviate this load, allowing clinicians to devote mental resources to patient evaluation and clinical reasoning. By reducing repetitive cognitive demands, technology supports professional well-being, enhances job satisfaction, and indirectly improves patient care through more focused, thoughtful clinical engagement.
Cultivating an Organizational Culture of Precision
The integration of technology into documentation transcends operational benefits to shape organizational culture. Emphasizing accuracy, accountability, and timely record-keeping fosters a shared ethos among clinical, administrative, and coding teams. Institutions that prioritize precision through technological augmentation cultivate environments in which staff members recognize the intrinsic value of meticulous documentation. This cultural shift reinforces compliance, reduces errors, and aligns organizational priorities with patient-centered excellence.
Scalability and Adaptability in Modern Healthcare
Healthcare organizations face ever-expanding patient populations and increasingly complex clinical interventions. Scalable, adaptable documentation solutions enable institutions to accommodate growth without sacrificing accuracy or efficiency. Cloud-based platforms, modular workflows, and AI-driven adaptability ensure that documentation systems remain resilient amidst changing operational demands. Such scalability ensures that quality is preserved even as institutional scope and complexity expand.
Continuous Evolution of Documentation Practices
Technology catalyzes the ongoing evolution of clinical documentation, encouraging iterative refinement and adaptive innovation. Emerging tools—ranging from voice recognition to predictive coding algorithms—offer new avenues for enhancing record fidelity and operational efficiency. By remaining responsive to technological advancements, healthcare organizations can sustain high standards of documentation integrity, ensuring that record-keeping practices evolve in tandem with clinical, regulatory, and operational imperatives.
Data-Driven Decision Making in Documentation
The aggregation and analysis of documentation data empower leadership to make informed decisions regarding staffing, workflow allocation, and policy development. Insightful dashboards and analytical reports illuminate areas of inefficiency, potential risk, and best-practice adherence. This data-centric approach fosters strategic decision-making, guiding organizational priorities with empirical evidence and reinforcing the role of documentation as a cornerstone of operational intelligence.
Interfacing Technology with Human Judgment
Despite technological sophistication, human judgment remains indispensable in clinical documentation. AI and automation complement rather than replace professional discernment, ensuring that nuanced decisions reflect both contextual understanding and patient-specific considerations. This symbiotic interface between machine precision and human intuition maximizes both accuracy and relevance, illustrating how technology can enhance rather than supplant clinical expertise.
Future Directions in Documentation Enhancement
Looking forward, the trajectory of documentation innovation is poised toward greater interoperability, predictive sophistication, and adaptive intelligence. Emerging paradigms—such as integrated AI learning loops, context-aware documentation systems, and real-time cognitive augmentation—promise to further enhance accuracy, efficiency, and clinician engagement. By proactively exploring and adopting these innovations, healthcare organizations position themselves at the vanguard of documentation excellence, capable of meeting the demands of increasingly complex and data-rich clinical environments.
Harmonizing Technology and Expertise
leveraging technology to enhance documentation integrity is neither a replacement for professional skill nor a mere convenience—it is a strategic imperative. AI, automation, and intelligent workflow platforms serve as catalysts for accuracy, efficiency, and compliance, while certified expertise ensures contextual relevance, interpretive nuance, and ethical oversight. Together, they form a synergistic ecosystem in which documentation transcends administrative necessity to become an instrument of clinical excellence, operational efficiency, and patient-centered care. Institutions that successfully integrate technological sophistication with professional acumen cultivate a culture of precision, safeguard patient safety, and achieve sustainable improvement in both operational and clinical outcomes.
The Imperative of Clinical Documentation Fidelity
Clinical documentation fidelity is not merely a procedural obligation; it represents the nexus between patient care, organizational efficacy, and regulatory compliance. Within the intricate lattice of healthcare operations, accurate documentation forms the sine qua non for reliable data, reimbursement accuracy, and patient safety. Healthcare ecosystems thrive when the documentation substratum is meticulously maintained, minimizing ambiguity, preempting errors, and fortifying institutional credibility. The cultivation of this precision mandates a blend of rigorous education, deliberate mentorship, and proactive leadership.
Educational Pathways as the Pillar of Excellence
The pursuit of clinical documentation excellence is inseparable from structured educational endeavors. Continuous professional development endows practitioners with the perspicacity necessary to navigate complex coding systems, interpret evolving regulatory mandates, and translate clinical encounters into cogent records. CDIP-certified professionals embody this confluence of knowledge and application, serving as conduits of expertise within clinical settings. Workshops, advanced seminars, and interactive e-learning modules offer dynamic modalities for sustaining cognitive acuity, ensuring that documentation practices remain aligned with contemporary standards.
Mentorship and Knowledge Diffusion
Mentorship constitutes a critical mechanism in propagating documentation proficiency. Experienced CDIP-certified professionals function as intellectual lodestars, guiding nascent practitioners through the labyrinthine corridors of clinical nomenclature, coding conventions, and compliance parameters. This relational pedagogy promotes not only skill acquisition but also a cultural assimilation of excellence, where the subtleties of accurate documentation are internalized and consistently applied. Through sustained mentorship, organizations cultivate an ethos of perpetual improvement, mitigating lapses in documentation quality and enhancing interdisciplinary collaboration.
Leadership as the Arbiter of Quality
Leadership exerts a decisive influence over the trajectory of clinical documentation standards. Administrators who champion the pursuit of CDIP certification for staff implicitly endorse a culture of accountability and precision. By strategically aligning resources, technology, and training initiatives with organizational objectives, leaders operationalize a framework wherein accurate documentation is incentivized, monitored, and systematically reinforced. Executive oversight ensures that documentation integrity transcends individual effort, becoming a collective institutional hallmark that underpins regulatory compliance and operational efficiency.
The Nexus of Technology and Documentation
The contemporary healthcare landscape is inextricably intertwined with technological innovation. Electronic health records, advanced analytics platforms, and AI-driven coding solutions have redefined the modalities through which documentation is captured, analyzed, and utilized. CDIP-certified professionals are uniquely positioned to interface between clinical acumen and technological infrastructure, ensuring that digital solutions augment rather than obfuscate clinical clarity. Mastery of these tools enables practitioners to anticipate documentation exigencies, streamline workflow, and preserve the fidelity of patient records amid a rapidly evolving digital milieu.
Regulatory Evolution and Compliance Dynamics
Healthcare regulations are in constant flux, reflecting shifts in policy, reimbursement frameworks, and quality metrics. Documentation specialists must possess the perspicacity to interpret these changes and integrate them into everyday practice. CDIP certification signifies not merely technical competence but also a commitment to regulatory vigilance. Professionals equipped with this certification proactively monitor legislative trends, evaluate organizational adherence, and provide strategic counsel to minimize risk exposure. In this way, documentation fidelity transcends administrative compliance, becoming an instrument of organizational resilience and patient advocacy.
Interdisciplinary Collaboration and Communication
Effective documentation is contingent upon seamless communication across multidisciplinary teams. Clinical documentation specialists act as intermediaries, translating clinical narratives into codified data that is intelligible to coders, administrators, and quality auditors alike. By fostering dialogue between disparate healthcare constituencies, these professionals ensure that patient encounters are comprehensively captured, accurately interpreted, and appropriately acted upon. Networking through professional associations amplifies this effect, facilitating the exchange of best practices, innovative methodologies, and solutions to recurrent challenges in documentation fidelity.
Strategic Investment in Professional Development
Organizations that invest in the advanced training and certification of their documentation staff reap multifaceted benefits. CDIP-certified practitioners not only enhance record accuracy but also drive operational efficiency, optimize reimbursement processes, and reduce the incidence of compliance infractions. Strategic professional development initiatives encompass targeted workshops, mentorship programs, and opportunities for cross-functional engagement, cultivating a workforce that is both competent and resilient. Such investment underscores a long-term commitment to documentation excellence as a strategic organizational priority rather than a reactive measure.
The Cognitive Dimensions of Documentation Mastery
Clinical documentation mastery necessitates cognitive dexterity. Professionals must synthesize multifarious data points, discern relevant clinical indicators, and translate complex encounters into coherent narratives. This intellectual rigor is further complicated by the interplay of coding intricacies, regulatory stipulations, and technological modalities. CDIP-certified practitioners cultivate analytical precision, employing critical thinking to resolve ambiguities, identify gaps, and ensure that documentation is both accurate and defensible. This cerebral rigor elevates documentation from a perfunctory task to a disciplined practice integral to patient care and institutional credibility.
Anticipating Future Paradigms in Documentation
The trajectory of clinical documentation is poised to intersect with emergent paradigms in artificial intelligence, predictive analytics, and integrated care models. Organizations must anticipate these shifts, fostering a culture of agility, continuous learning, and technological literacy. CDIP-certified professionals serve as vanguards in this evolution, bridging the chasm between traditional documentation methodologies and next-generation innovations. Their expertise enables healthcare institutions to proactively adapt to emergent demands, mitigate transitional risks, and sustain operational excellence in a landscape characterized by perpetual flux.
Cultural and Organizational Implications
The cultivation of a documentation-centric culture extends beyond technical training. Leaders who prioritize documentation excellence embed its principles within organizational ethos, shaping expectations, behaviors, and reward structures. Such a culture valorizes precision, accountability, and interdisciplinary cooperation, aligning individual performance with institutional imperatives. CDIP-certified professionals act as cultural stewards, reinforcing these values through mentorship, advocacy, and example. The resultant organizational climate fosters resilience, minimizes errors, and promotes a shared commitment to clinical and administrative integrity.
Leveraging Analytics for Documentation Optimization
Data analytics has emerged as a transformative tool in clinical documentation management. By systematically analyzing documentation patterns, organizations can identify discrepancies, assess compliance adherence, and forecast areas requiring intervention. CDIP-certified specialists leverage these insights to optimize workflow, inform targeted training, and enhance coding accuracy. Analytics-driven strategies enable organizations to convert raw documentation data into actionable intelligence, bridging the gap between operational execution and strategic decision-making. This integration of data science with documentation practice exemplifies the forward-looking potential of professional expertise.
Ethical Considerations in Documentation Practices
Ethical stewardship is an indispensable dimension of clinical documentation. Practitioners must navigate the tension between administrative demands, clinical realities, and patient privacy. CDIP-certified professionals embody ethical vigilance, ensuring that documentation accurately reflects patient encounters while safeguarding confidentiality. Ethical practice entails more than mere compliance; it requires a conscientious engagement with the moral implications of documentation, fostering trust between patients, clinicians, and institutions. This ethical orientation reinforces the credibility of healthcare operations and strengthens institutional integrity.
Interpersonal Dynamics and Professional Influence
The efficacy of clinical documentation extends beyond technical proficiency to encompass interpersonal acumen. CDIP-certified professionals often function as influential agents within clinical teams, mediating disputes, clarifying ambiguities, and fostering mutual understanding. Their capacity to articulate complex documentation standards in accessible terms enhances cohesion, minimizes errors, and facilitates organizational alignment. Professional influence, exercised with empathy and strategic insight, amplifies the impact of documentation initiatives, transforming individual expertise into collective operational excellence.
Sustaining Documentation Excellence Amid Change
Healthcare environments are inherently dynamic, characterized by fluctuating regulatory landscapes, technological disruptions, and evolving patient needs. Sustaining documentation excellence in such contexts demands adaptability, foresight, and proactive leadership. CDIP-certified practitioners are uniquely equipped to navigate this volatility, employing continuous learning, mentorship, and analytical precision to maintain high standards. Organizations that embrace this adaptive approach ensure continuity of excellence, safeguarding patient care quality while optimizing administrative performance.
Financial Implications of Documentation Accuracy
Accurate clinical documentation is a critical determinant of organizational financial health. Errors or omissions can precipitate claim denials, regulatory penalties, and lost revenue opportunities. CDIP-certified professionals mitigate these risks through meticulous attention to detail, systematic auditing, and proactive corrective strategies. By ensuring that records are comprehensive and compliant, these specialists enhance reimbursement accuracy, streamline billing processes, and contribute to fiscal sustainability. Documentation excellence thus intersects with financial stewardship, underscoring its multifaceted strategic value.
Integrating Continuous Feedback Mechanisms
Continuous feedback mechanisms constitute a vital instrument in sustaining documentation proficiency. Regular audits, peer reviews, and performance evaluations provide actionable insights, enabling practitioners to refine skills and rectify deficiencies. CDIP-certified professionals advocate for and implement these feedback loops, fostering a culture of perpetual improvement. Iterative assessment ensures that documentation standards evolve in response to emerging best practices, regulatory updates, and technological innovations, thereby maintaining organizational resilience and operational integrity.
The Role of Advocacy in Documentation Advancement
Advocacy is integral to advancing the field of clinical documentation. CDIP-certified practitioners champion policies, resources, and initiatives that elevate documentation standards, promote professional recognition, and facilitate systemic improvements. By participating in professional networks, contributing to policy discourse, and mentoring emerging professionals, these individuals shape the trajectory of documentation practice. Advocacy transforms documentation from a localized administrative function into a field of strategic, professional, and ethical significance.
Convergence of Clinical Expertise and Administrative Precision
The hallmark of CDIP-certified professionals lies in their ability to integrate clinical insight with administrative exactitude. This convergence ensures that documentation faithfully represents patient encounters while satisfying coding, billing, and compliance imperatives. Such dual proficiency enables organizations to reconcile the often divergent priorities of clinical care and operational efficiency, delivering patient-centered outcomes without compromising regulatory or fiscal responsibilities. The synthesis of expertise underscores the transformative potential of well-trained documentation specialists.
Preparing for a Data-Driven Healthcare Ecosystem
The evolution of healthcare into a data-centric ecosystem underscores the imperative of precise documentation. Structured, accurate records serve as the substrate for analytics, population health initiatives, and evidence-based practice. CDIP-certified professionals contribute to this ecosystem by ensuring that documentation is granular, standardized, and actionable. Their work enables organizations to harness data effectively, informing strategic planning, quality improvement, and patient care optimization in a complex and increasingly data-intensive environment.
The Strategic Imperative of Certification
Certification is more than a credential; it represents a strategic investment in organizational capability. CDIP-certified professionals validate their proficiency in clinical documentation, regulatory adherence, and technological fluency, offering tangible value to healthcare institutions. Organizations that prioritize certification cultivate a cadre of practitioners capable of sustaining documentation excellence, optimizing operational performance, and navigating regulatory complexity. Certification thus functions as both a marker of individual competence and a lever for organizational advancement.
A Future Anchored in Excellence
Sustaining clinical documentation excellence requires a synthesis of education, mentorship, leadership, and technological adeptness. CDIP-certified professionals embody these attributes, translating knowledge into actionable practices that safeguard patient care, ensure compliance, and enhance organizational efficiency. In an era characterized by rapid change and escalating complexity, investing in documentation expertise is not a peripheral concern but a strategic imperative. By fostering a culture of precision, adaptability, and continuous improvement, healthcare organizations can secure a future defined by operational excellence, ethical integrity, and superior patient outcomes.
The evolving healthcare landscape necessitates a proactive approach to documentation, one that anticipates shifts in regulatory frameworks, technological integration, and interdisciplinary collaboration. As healthcare systems become increasingly interconnected and data-driven, the demand for precise, actionable clinical records intensifies. CDIP-certified professionals are uniquely positioned to navigate this terrain, functioning as linchpins that bridge clinical insight, administrative rigor, and technological fluency. Their role is not static; it evolves in concert with emerging challenges, positioning them as architects of both operational resilience and quality patient care.
Technological innovation, particularly in the domains of artificial intelligence, machine learning, and predictive analytics, is redefining the paradigms of documentation. While these tools offer unparalleled efficiency, they also introduce new complexities. Automation may streamline coding and record-keeping, but human oversight remains indispensable to ensure contextual accuracy, interpret clinical subtleties, and mitigate potential errors. CDIP-certified practitioners provide the critical cognitive interface, integrating machine-generated outputs with nuanced clinical judgment. In doing so, they ensure that technological augmentation complements rather than compromises documentation integrity.
The infusion of interdisciplinary collaboration further underscores the importance of a forward-looking approach. In contemporary healthcare settings, patient care is increasingly delivered by multifaceted teams that include physicians, nurses, allied health professionals, administrators, and informatics specialists. Effective documentation must therefore harmonize disparate perspectives, translating the granular details of clinical encounters into coherent, comprehensive records that satisfy multiple stakeholders. CDIP-certified professionals serve as facilitators and translators, ensuring that each component of patient care is accurately captured, codified, and communicated. Their work enhances clarity, reduces errors, and fosters a culture of accountability across the continuum of care.
In addition to technological and interdisciplinary considerations, regulatory evolution exerts a profound influence on documentation practices. Healthcare regulations are fluid, responding to policy shifts, emerging public health priorities, and evolving reimbursement models. Organizations that fail to anticipate or adapt to these changes risk compliance infractions, financial penalties, and reputational damage. CDIP-certified professionals, by virtue of their specialized training and certification, possess the foresight and analytical acumen necessary to interpret regulatory updates, integrate them into documentation protocols, and educate colleagues on best practices. Their strategic vigilance ensures that organizational processes remain aligned with current standards, mitigating risk and promoting sustainability.
A culture of continuous education is central to maintaining this future-focused approach. Healthcare documentation is inherently dynamic, with new coding systems, procedural nomenclatures, and compliance requirements emerging regularly. Ongoing professional development—through workshops, seminars, e-learning platforms, and peer-led mentorship—ensures that practitioners remain adept and responsive. CDIP-certified professionals often assume the role of educators within their institutions, disseminating knowledge, modeling best practices, and fostering environments where learning is perpetual rather than episodic. This commitment to intellectual agility cultivates a workforce capable of navigating uncertainty with confidence and precision.
The human dimensions of documentation excellence—ethical stewardship, interpersonal acuity, and cultural sensitivity—are equally salient. Beyond technical proficiency, CDIP-certified professionals embody ethical rigor, ensuring that patient information is captured truthfully, confidentially, and with respect for privacy considerations. They serve as mediators, reconciling divergent clinical interpretations, resolving ambiguities, and facilitating communication across hierarchical and disciplinary boundaries. By fostering trust and collaboration, these professionals transform documentation from a mere administrative function into a relationally anchored practice that upholds both professional integrity and patient-centered care.
Financial stewardship is an additional consideration in the pursuit of documentation excellence. Inaccurate, incomplete, or delayed records can precipitate claim denials, audit findings, and lost revenue opportunities. CDIP-certified practitioners, through meticulous attention to detail and adherence to compliance protocols, enhance the accuracy and completeness of documentation, optimizing reimbursement processes and fortifying institutional financial resilience. This dual focus on clinical fidelity and fiscal responsibility underscores the multifaceted value that certified professionals contribute to healthcare organizations.
Looking ahead, predictive analytics and data integration will further amplify the strategic significance of clinical documentation. Comprehensive, accurate records form the foundation for population health management, quality improvement initiatives, and evidence-based practice. CDIP-certified professionals ensure that documentation is not only precise but also structured in a manner conducive to data extraction, analysis, and decision-making. By bridging clinical encounters with organizational intelligence, they enable proactive interventions, trend identification, and resource optimization. In this way, documentation evolves from a retrospective record-keeping function into a forward-looking tool for strategic healthcare management.
Moreover, as patient engagement becomes increasingly central to healthcare delivery, documentation practices must reflect the nuances of patient experience, communication, and outcomes. CDIP-certified professionals contribute to this patient-centric orientation by ensuring that records accurately represent patient interactions, treatment decisions, and care trajectories. Their meticulous attention to detail ensures that every clinical narrative supports both high-quality care and informed decision-making, reinforcing patient trust and promoting shared accountability in the healthcare journey.
The strategic integration of CDIP-certified professionals also strengthens institutional adaptability. Healthcare organizations face unprecedented uncertainty—from policy fluctuations and technological disruption to evolving population health needs. By embedding documentation expertise within governance structures, institutions cultivate a nimble, responsive workforce capable of anticipating challenges, implementing solutions, and sustaining operational continuity. This forward-thinking integration transforms documentation excellence from a static compliance measure into a dynamic enabler of organizational resilience and innovation.
Conclusion
The future of clinical documentation is both promising and complex, demanding a synthesis of technical acumen, ethical vigilance, interdisciplinary collaboration, and strategic foresight. CDIP-certified professionals exemplify the competencies required to navigate this evolving landscape, ensuring that documentation remains accurate, compliant, and operationally impactful. Through continuous education, mentorship, technological integration, and ethical stewardship, these professionals serve as catalysts for quality care, organizational resilience, and sustainable financial performance.
Healthcare organizations that invest in cultivating documentation excellence position themselves at the vanguard of industry evolution, translating precise records into actionable insights, informed decision-making, and superior patient outcomes. By fostering a culture that values precision, adaptability, and continuous improvement, institutions not only comply with regulatory mandates but also elevate the standard of care across the continuum. In this light, clinical documentation transcends administrative necessity, emerging as a strategic linchpin—anchored in excellence, guided by expertise, and dedicated to the enduring advancement of healthcare quality and integrity.