Certification: ACSM Registered Clinical Exercise Physiologist
Certification Full Name: ACSM Registered Clinical Exercise Physiologist
Certification Provider: ACSM
Exam Code: 040-444
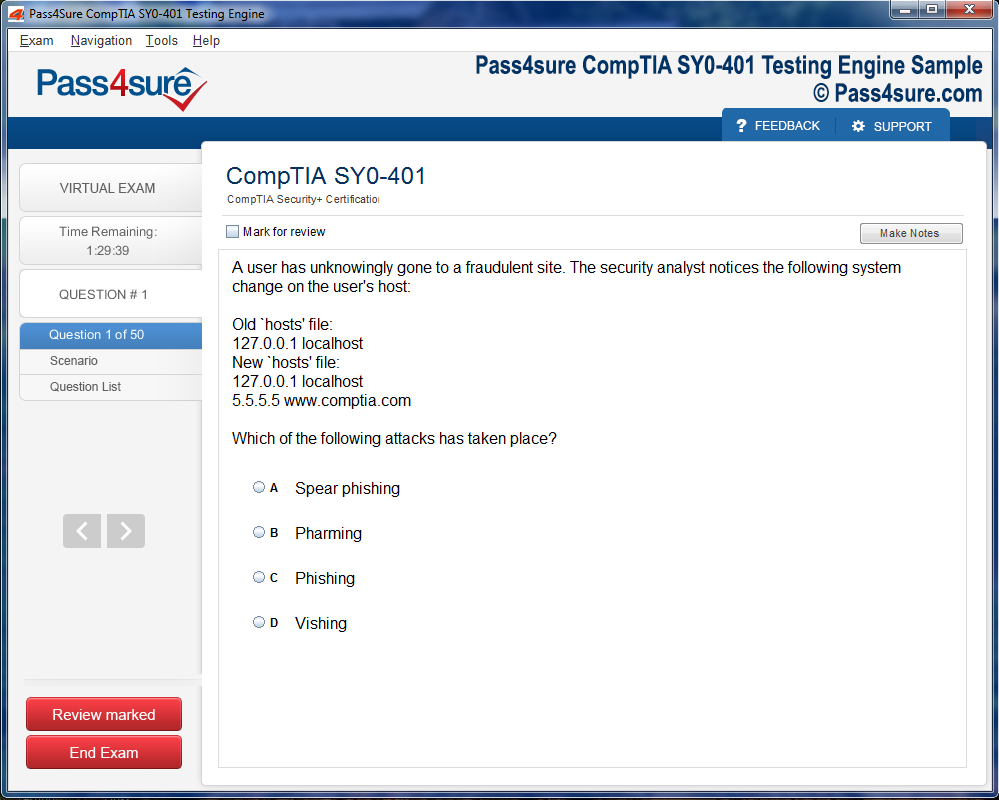
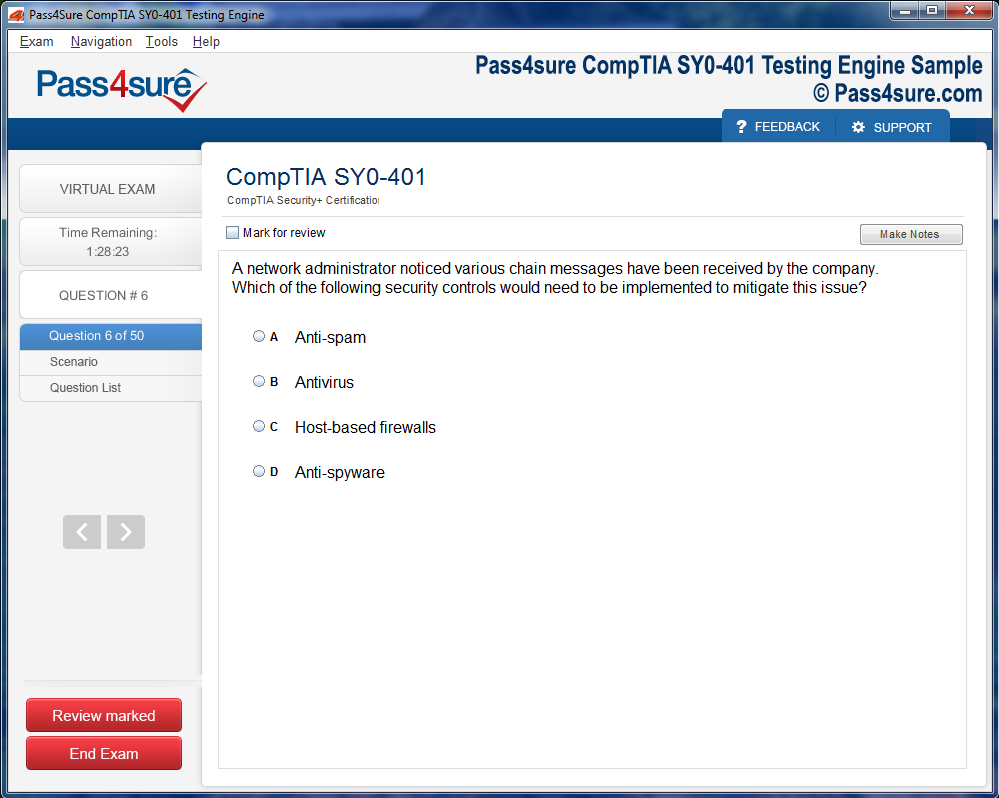
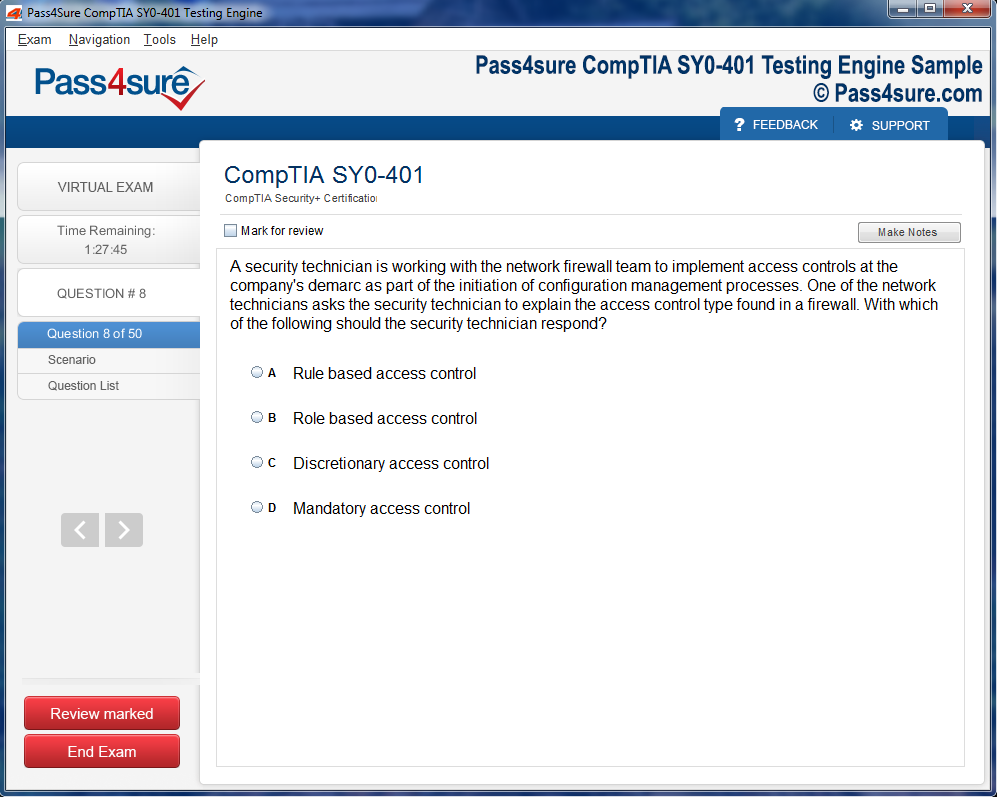
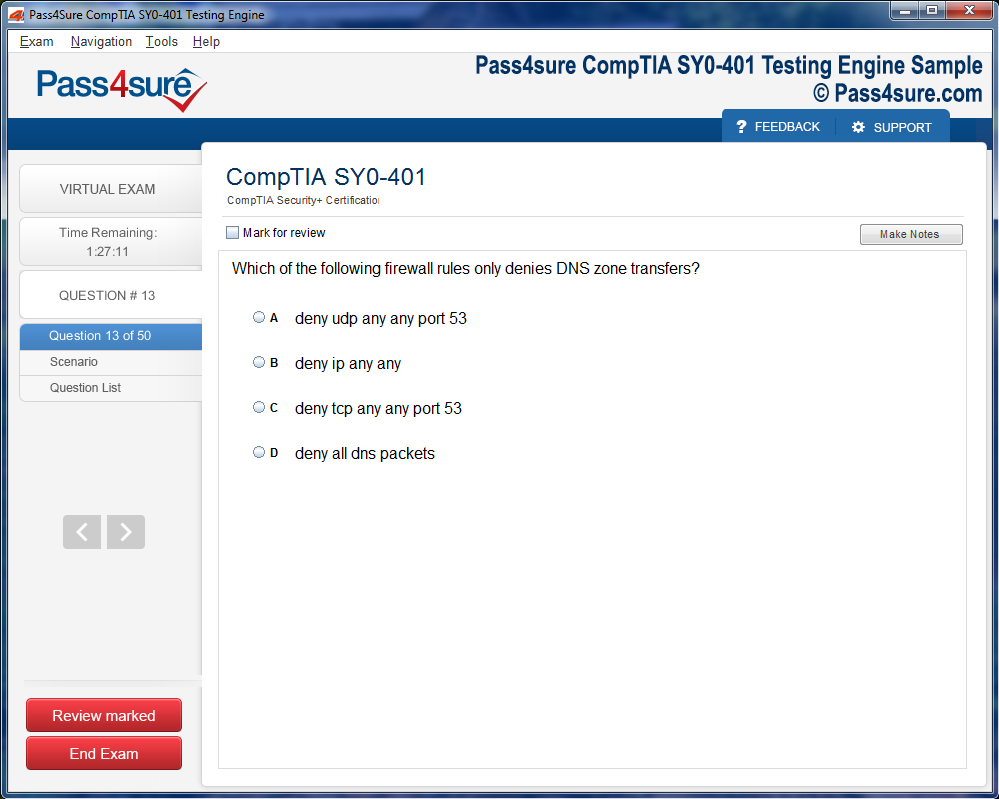
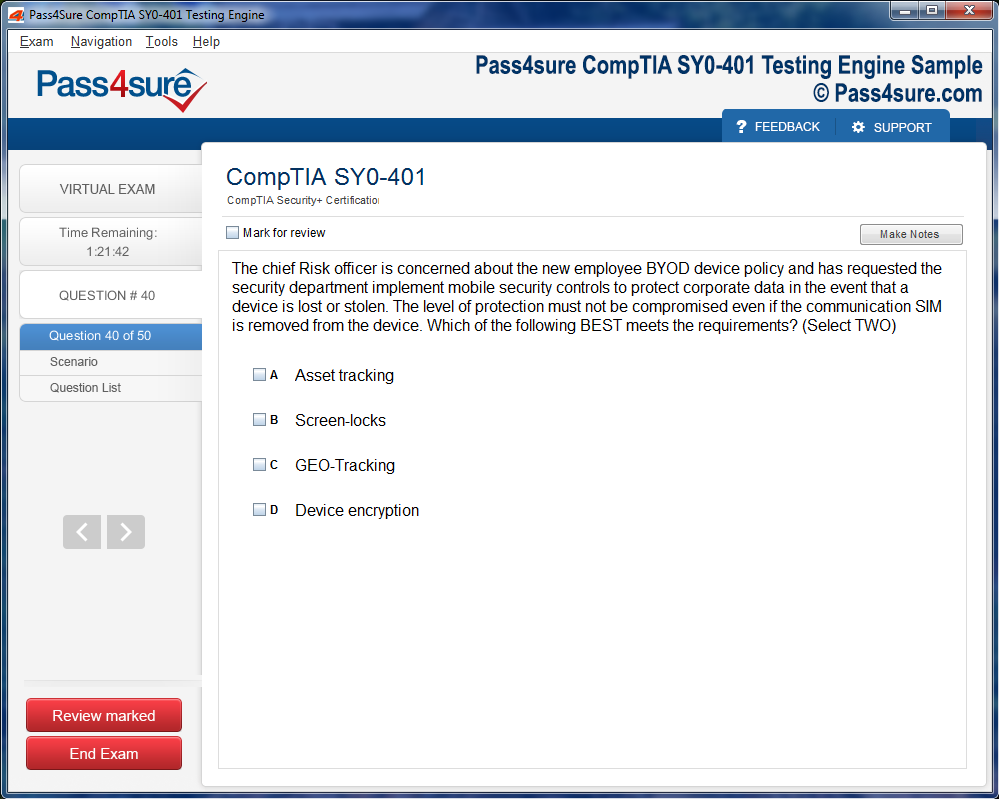
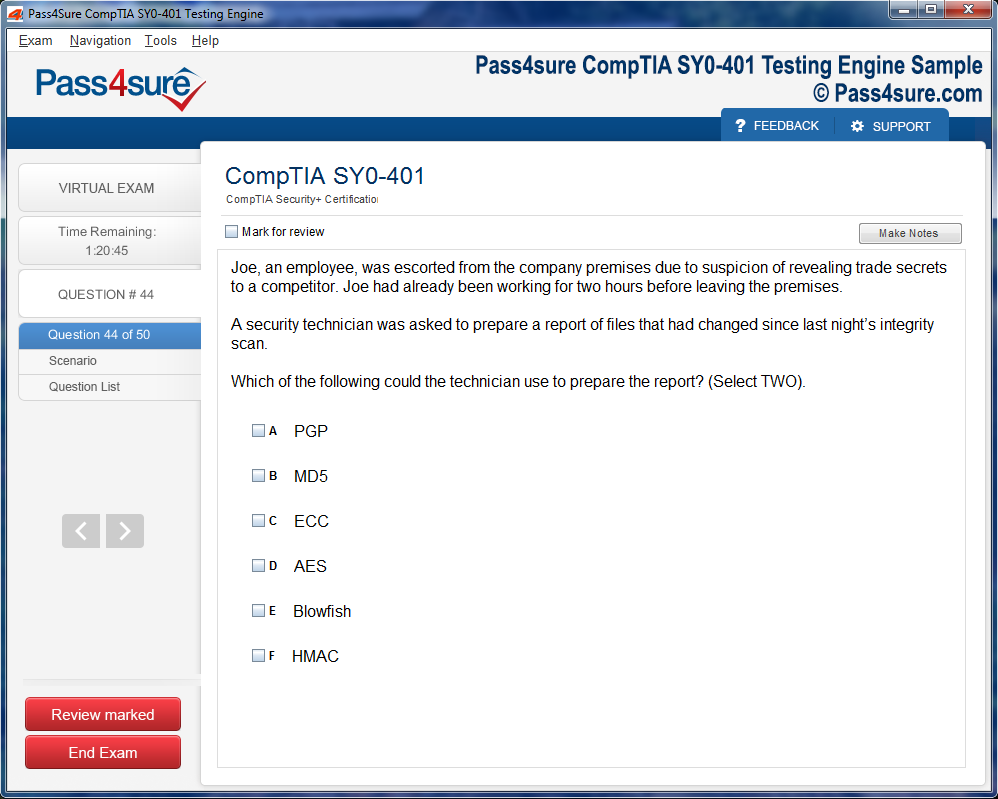
Product Screenshots
The Science of Healing Through Exercise: The Role of the ACSM Registered Clinical Exercise Physiologist
Within the quiet corridors of modern medicine, a subtle metamorphosis unfolds—one that intertwines movement and biology, empathy and evidence, discipline and grace. It is here, within this convergence, that the vocation of the ACSM Registered Clinical Exercise Physiologist reveals its transformative essence. No longer is healing confined to the sterile hum of machines or the delicate calibration of pharmaceuticals; it now extends into the rhythmic cadence of the human body in motion.
The ACSM Registered Clinical Exercise Physiologist perceives movement not as mere physical exertion but as a potent language of restoration. Each deliberate gesture, each measured inhalation, carries biochemical consequence. Muscles become messengers, translating motion into molecular repair. The act of walking, lifting, breathing—when structured through scientific precision—becomes as curative as medicine itself.
This evolution of care signals the birth of a philosophy: that recovery is not achieved through stillness, but through guided motion. In this world, every exercise is a prescription, every stretch a signature of science, every heartbeat a metric of transformation. Clinical exercise physiology thus becomes the meeting place of humanity’s oldest instinct—to move—and its most recent triumph—to understand.
The Ethos of Motion as Medicine
To the untrained eye, exercise appears as repetition and resistance, an external performance of strength. Yet beneath that visible choreography lies a symphony of invisible transformations. Cellular metabolism awakens, capillaries expand, hormones recalibrate, and neural pathways rejuvenate. The ACSM Registered Clinical Exercise Physiologist commands an understanding of this microscopic theatre. They orchestrate intensity, frequency, and recovery with the same nuance that a composer uses to balance silence and sound.
At the philosophical core of this discipline lies the doctrine of motion as medicine. Stillness, once perceived as rest, now reveals itself as decay. Inactivity disrupts circulation, erodes metabolic harmony, and diminishes vitality. Movement, conversely, rekindles equilibrium. Within every structured session, the ACSM Registered Clinical Exercise Physiologist aligns kinetics with healing, merging empirical analysis with human intuition.
The interaction between practitioner and patient transcends the transactional. It becomes an alliance rooted in trust and observation. Each assessment—whether measuring oxygen uptake, cardiovascular resilience, or muscular endurance—serves as a diagnostic conversation between physiology and expertise. Yet science alone does not suffice; empathy completes the equation. Where charts and data offer insight, compassion delivers adherence. Healing, in this paradigm, is a duet between data and devotion.
The Science of Biological Adaptation
Within the labyrinth of human physiology, adaptation reigns as the sovereign principle. The body, ever dynamic, alters itself in response to challenge. Each contraction signals microscopic restructuring; each pulse ushers a cascade of hormonal regulation. The ACSM Registered Clinical Exercise Physiologist interprets these intricate responses with clinical acuity, designing interventions that refine rather than exhaust, fortify rather than fatigue.
During every controlled session, mitochondria multiply, capillaries sprout, and enzymes evolve toward efficiency. This metamorphic dialogue between effort and evolution is the true artistry of clinical exercise physiology. The practitioner’s role extends beyond prescribing exertion; it encompasses deciphering the language of adaptation itself. Through monitoring electrocardiographic waves, metabolic flux, and hemodynamic shifts, they ensure that every threshold crossed is safe, purposeful, and progressive.
The brilliance of adaptation lies in its universality. It touches the cardiac patient reclaiming stamina, the diabetic seeking metabolic stability, and the stroke survivor rediscovering motion. Exercise becomes an act of reclamation, and adaptation to the script of recovery. To the ACSM Registered Clinical Exercise Physiologist, the patient’s body is a living manuscript, and every session another verse in its rewriting.
The Interdisciplinary Symphony of Healing
Modern healthcare thrives on collaboration, and within this intricate network, the ACSM Registered Clinical Exercise Physiologist stands as both scientist and sentinel. They interpret the silent whispers of physiology, translating them into actionable movement. Their presence bridges the gulf between diagnostic medicine and rehabilitative progression. Within hospital units, outpatient clinics, and community health centers, their expertise infuses vitality into the framework of care.
In cardiac rehabilitation, they choreograph gradual reacquaintance with endurance, guiding patients who once feared exertion back into a confident rhythm. In metabolic clinics, they cultivate resilience against the biochemical turbulence of insulin resistance, designing protocols that recalibrate rather than overwhelm. Their work in pulmonary rehabilitation restores the breath’s forgotten confidence, training the respiratory system to find strength in measured persistence.
This interdisciplinary harmony requires the ability to converse fluently in both scientific and human terms. The ACSM Registered Clinical Exercise Physiologist communicates with physicians, nurses, psychologists, and dietitians, yet their most profound dialogue occurs with the patient’s body itself. The heart rate monitor becomes a translator, the treadmill a confessional, the pulse oximeter an oracle. Through these tools, the physiologist listens deeply—to data, to silence, to the patient’s unspoken hopes.
The Humanization of Science
Amid technology and metrics, the true artistry of the ACSM Registered Clinical Exercise Physiologist lies in humanization. They do not see patients as pathologies to be corrected but as narratives to be rewritten. The clinical environment, often sterile and impersonal, transforms under their guidance into a sanctuary of motion and meaning.
A patient emerging from cardiac trauma often carries more than physical fragility—there is fear, uncertainty, and a quiet mourning for former vitality. The physiologist becomes both guide and witness, helping them reclaim autonomy one measured step at a time. Through precise progression and reassurance, exercise becomes an affirmation that recovery is possible, not hypothetical.
For another individual managing chronic pulmonary disease, the struggle to breathe becomes the central metaphor of their existence. The physiologist’s structured interventions retrain the diaphragm, expand lung capacity, and restore trust in the body’s ability to sustain. What begins as a clinical exercise evolves into liberation from the invisible prison of breathlessness.
Here, data becomes secondary to dignity. Science bends toward humanity. Healing, in this context, is not mechanical—it is relational, experiential, profoundly personal. The ACSM Registered Clinical Exercise Physiologist embodies the rare union of empirical intellect and empathic grace.
The Craft of Clinical Precision
To the observer, a session may appear simple—repetitions, rest intervals, progressive loading. Yet beneath the visible simplicity lies a cathedral of precision. Each decision—the angle of movement, the pace of progression, the monitoring of vitals—is governed by physiological logic. Nothing is arbitrary. Every motion is calculated to elicit an adaptive cascade without exceeding tolerance.
During graded exercise testing, the ACSM Registered Clinical Exercise Physiologist deciphers subtleties that others might overlook: minute fluctuations in cardiac rhythm, microscopic delays in oxygen kinetics, nuanced deviations in perceived exertion. This interpretive skill transforms complex physiological data into safe, effective movement therapy.
Such mastery emerges only from rigorous education and relentless practice. The journey toward this credential is not merely academic but experiential. It demands immersion in anatomy, biochemistry, pathophysiology, and behavioral psychology. The training embeds an intuitive sense of balance—when to push, when to pause, when to modify. Over time, the physiologist becomes both clinician and artist, blending measurement with instinct.
Their decisions ripple outward, influencing not just recovery but long-term vitality. By interpreting subtle biomarkers, they prevent relapse, safeguard cardiac function, and restore metabolic integrity. Precision, in this craft, is not rigidity; it is an evolving dialogue between evidence and experience.
The Educational Journey of Mastery
The making of an ACSM Registered Clinical Exercise Physiologist is an odyssey through layers of knowledge and empathy. It begins within academic sanctuaries, where future practitioners absorb the architecture of the human organism—the pulse of circulation, the symphony of respiration, the chemical whispers of metabolism. Yet theory alone is insufficient. The crucible of clinical practice forges competence into wisdom.
In supervised rotations, they confront the raw complexity of human fragility: the trembling gait of post-surgical recovery, the uncertainty of a diabetic managing glucose fluctuations, the cautious optimism of a heart patient rediscovering endurance. Here, the abstractions of physiology acquire faces, voices, and stories. Science begins to feel human.
Certification, though a formal milestone, is only the threshold. Lifelong education becomes both an obligation and an instinct. The evolving discoveries of molecular biology, biomechanics, and clinical technology require constant adaptation. The true hallmark of mastery lies not in memorized protocols but in the capacity to evolve. The ACSM Registered Clinical Exercise Physiologist remains both student and innovator, forever refining their craft to mirror the ever-changing contours of human health.
The Resonance of Preventive Care
While clinical exercise physiology often enters the narrative of rehabilitation, its true potency may lie in prevention. The body thrives not in crisis but in preparation. The ACSM Registered Clinical Exercise Physiologist envisions health not as the absence of disease but as a dynamic state of adaptability. Their mission extends beyond the recovery ward into workplaces, schools, and communities, where movement becomes a social prescription.
They advocate for environments that invite motion—ergonomic designs, accessible fitness programs, educational campaigns that redefine physical activity as integral, not optional. In doing so, they influence the trajectory of public health. Chronic conditions such as cardiovascular disease, metabolic syndrome, and musculoskeletal decline can be forestalled when society embraces exercise as a universal medicine.
In preventive sessions, the physiologist teaches subtle self-awareness. Patients learn to listen to their bodies, to perceive fatigue not as weakness but as feedback, to recognize exertion as communication. The culture of care shifts from reaction to anticipation. Health becomes not a goal but a practice, not a finish line but a rhythm.
The Emotional Architecture of Recovery
Every clinical encounter unfolds within an emotional landscape. Pain, uncertainty, frustration, and hope coexist in a delicate balance. The ACSM Registered Clinical Exercise Physiologist navigates this emotional topography with patience and poise. They understand that physiological progress often follows psychological permission. A fearful patient cannot adapt efficiently; a confident one can transcend limitation.
Through careful dialogue, they dismantle the architecture of fear. Words become as potent as protocols. Encouragement replaces apprehension, curiosity replaces dread. The act of movement transforms from obligation into celebration. In that transformation, the patient discovers not just recovery but resilience.
Emotional intelligence thus becomes a clinical tool as vital as any instrument. The ACSM Registered Clinical Exercise Physiologist uses empathy as calibration—sensing hesitation, measuring courage, adjusting pace. Healing becomes a collaborative rhythm, composed not of commands but of shared conviction.
The Evolution of Clinical Technology
The modern ACSM Registered Clinical Exercise Physiologist operates at the intersection of human touch and technological sophistication. Advanced devices capture the minutiae of motion—heart rate variability, oxygen saturation, power output, and biomechanical alignment. Yet these technologies serve as mirrors, not masters. The physiologist interprets them through the lens of humanity, ensuring that data enhances rather than eclipses care.
Emerging technologies such as wearable biosensors and telemetric monitoring expand the reach of personalized rehabilitation. Remote feedback systems allow patients to perform guided sessions under invisible supervision, maintaining consistency without compromising safety. Artificial intelligence, once peripheral, now assists in analyzing massive datasets, identifying patterns that inform individualized progression.
But the physiologist’s intuition remains irreplaceable. Machines can quantify; only humans can contextualize. The marriage of technology and empathy creates a new paradigm of care—precise yet personal, digital yet deeply human. The ACSM Registered Clinical Exercise Physiologist stands at this crossroads, translating innovation into intimacy.
The Expanding Horizon of Global Health
As chronic illnesses proliferate worldwide, the demand for scientifically guided exercise intervention increases. The ACSM Registered Clinical Exercise Physiologist becomes an architect of resilience within an overstressed healthcare system. Their work mitigates the economic and emotional burden of disease, empowering societies to move from reactive medicine toward proactive wellness.
In developing regions, they advocate for community-based programs that transform limited resources into dynamic movement platforms. In technologically advanced nations, they refine digital rehabilitation protocols that harmonize convenience with clinical integrity. Across all cultures, they embody the same philosophy: that motion is the universal dialect of vitality.
The implications ripple across generations. When elders regain mobility, families regain stability. When youth embrace activity as identity, societies safeguard longevity. The ACSM Registered Clinical Exercise Physiologist does not merely rehabilitate individuals—they recalibrate humanity’s understanding of health.
The Poetics of Purpose
Beyond measurement and medicine lies something subtler: meaning. Every patient’s story becomes a verse in the evolving poem of clinical exercise physiology. The ACSM Registered Clinical Exercise Physiologist serves as both author and listener, shaping movement into metaphor, turning exertion into eloquence.
A cancer survivor learns to lift again, not for strength alone but to reclaim agency. A cardiac patient walks further each week, not just to train the heart but to prove its endurance mirrors their own. The physiologist observes these moments with quiet reverence, knowing that the truest metric of success is not in data but in restored dignity.
Clinical exercise physiology, at its highest expression, transcends therapy. It becomes philosophy—an affirmation that the human body, when guided by knowledge and nurtured by compassion, possesses infinite capacity for renewal. Through this practice, motion becomes memory, endurance becomes enlightenment, and healing becomes an art without conclusion.
Metabolic Symphonies: Exercise as Restorative Alchemy
Metabolism is the silent alchemist within, transforming ingested sustenance into kinetic vigor, cognitive lucidity, and cellular vitality. Yet in the cadence of contemporary life, where lethargy reigns and processed indulgences proliferate, this alchemy falters. Disorders once uncommon—diabetes, obesity, and the constellation of metabolic syndrome—have burgeoned, revealing the fragility of unmodulated physiology. Within this complex labyrinth, the ACSM Registered Clinical Exercise Physiologist assumes a role both pragmatic and transformative, converting metabolic theory into orchestrated movement that reanimates balance and vigor.
Cells converse in biochemical dialects, exchanging signals, catalyzing reactions, and converting nutrients into energy. Exercise, precisely dosed and strategically timed, acts as a lingua franca in this conversation, guiding reactions toward homeostasis and resilience. The clinical exercise physiologist becomes a choreographer of this internal symphony, ensuring that each contraction, each inhalation, and every cadence of motion contributes to the restoration of metabolic poise.
The Epidemic of Sedentary Imbalance
The rise of metabolic disorders extends beyond medical pathology; it is a societal lament. Convenience has eclipsed exertion, and ease has generated systemic discord. The ACSM Registered Clinical Exercise Physiologist confronts this imbalance by architecting movement patterns that awaken dormant metabolic circuits. Carefully prescribed regimens—tailored to the singular physiology of each client—resurrect cellular efficiency, rekindling vitality in previously quiescent pathways.
Prolonged sedentarism diminishes insulin sensitivity and retards glucose assimilation, forging cycles of fatigue and adiposity. Through targeted aerobic and resistance interventions, the physiologist invigorates muscular tissue, transforming it into a metabolic engine capable of sustained fuel utilization. Over time, these adaptations stabilize glycemic flux and enhance energetic equilibrium even at rest.
Exercise as Molecular Modulator
Physical activity evokes intricate physiological choreography. During exertion, glucose transporters migrate to cellular membranes, facilitating insulin-independent glucose uptake. This natural mechanism is harnessed to mitigate insulin resistance and normalize glycemia. The ACSM Registered Clinical Exercise Physiologist calibrates these responses, designing exercise prescriptions that optimize benefit while circumventing overexertion or injury.
Resistance modalities expand lean muscle mass, elevating basal metabolic rate, while aerobic conditioning amplifies mitochondrial density and cardiovascular efficacy. The convergence of these adaptations orchestrates systemic metabolic harmony. In individuals contending with obesity, the process transcends mere caloric expenditure, emphasizing metabolic flexibility—the capacity to seamlessly shift between carbohydrate and lipid substrates. As this adaptability flourishes, energy surges, cravings wane, and overall vitality intensifies.
Individualized Metabolic Renaissance
No two human metabolisms are congruent. Clinical exercise physiology recognizes that uniform approaches fail to honor genetic diversity, medical nuance, and lifestyle idiosyncrasies. Comprehensive assessments—encompassing body composition, resting metabolic rate, and cardiovascular capacity—form the scaffolding upon which bespoke programs are constructed.
Prediabetic clients may commence with low-intensity continuous modalities to optimize insulin sensitivity, whereas individuals with joint limitations might explore aquatic therapy. Intensity, volume, and frequency are perpetually calibrated, allowing for progressive adaptation without compromise to safety or efficacy. Progress is quantified not solely in pounds shed but through biomarkers—lipid profiles refined, fasting glucose moderated, blood pressure stabilized—evidencing the body's intrinsic potential for self-restoration.
Synergy of Nutrient and Motion
Metabolic restoration is rarely the province of exercise alone. The ACSM Registered Clinical Exercise Physiologist collaborates with nutritional specialists to synchronize movement with sustenance. Exercise heightens nutrient receptivity, enabling macronutrients to be converted into functional energy more efficiently. Strategic timing of meals relative to activity ensures stable energy availability, while post-exercise nutrition supports glycogen replenishment and myofibrillar repair. This synthesis engenders a metabolic cadence that persists beyond the clinical environment, nurturing a rhythm of cellular equilibrium.
Emotional Reclamation Through Physical Agency
Metabolic dysfunction often bears an emotional toll, manifesting as guilt, frustration, or despondence. The ACSM Registered Clinical Exercise Physiologist approaches the patient with empathetic acuity, transforming exercise into an instrument of empowerment. Milestones—small yet profound—rekindle confidence, reframing movement as identity rather than obligation. Each increment of progress reinforces the body-mind connection, reconstituting a narrative of capability and resilience.
Hormonal Equilibrium and Biochemical Restoration
Exercise exerts a profound influence on endocrine homeostasis. Endorphin release mitigates stress, while cortisol attenuation preserves metabolic function. Complementary strategies—controlled breathing, mindful stretching, and movement meditations—enhance recovery and amplify hormonal balance. Furthermore, adaptations in leptin and adiponectin secretion recalibrate appetite and lipid metabolism. These subtle shifts, facilitated by precise intervention, underpin sustainable metabolic restoration and weight regulation.
Data-Infused Precision in Exercise Therapy
Advances in technology have transformed clinical exercise into a data-driven science. Continuous glucose monitoring, metabolic analyzers, and wearable trackers furnish real-time insights, enabling physiologists to fine-tune intensity, duration, and recovery. The integration of empirical data converts subjective perception into measurable progress, while remote monitoring ensures sustained accountability. The ACSM Registered Clinical Exercise Physiologist thereby assumes dual roles: empirical analyst and guiding mentor, uniting precision with compassion.
Mitochondrial Vitalization and Cellular Energetics
At the microscopic frontier, exercise induces mitochondrial biogenesis, amplifying ATP production and diminishing oxidative stress. Tailored protocols—ranging from interval training to moderate continuous activity—maximize mitochondrial adaptation. Enhanced organelle efficiency mitigates fatigue, harmonizes substrate utilization, and restores intrinsic energetic equilibrium. This cellular rejuvenation constitutes the zenith of metabolic healing, a renewal that originates from the molecular nucleus and radiates outward.
Preventive Paradigms and Societal Implications
Beyond therapy, clinical exercise physiology cultivates prevention. Early identification of metabolic perturbations, coupled with community-based interventions, can attenuate disease progression. Programs spanning schools, workplaces, and public initiatives propagate an ethos of motion as essential sustenance. By embedding exercise into daily life, these interventions shift healthcare from reactive remediation to proactive vitality, reshaping population health trajectories.
Measuring Transformation Beyond Quantification
True metabolic restoration transcends laboratory metrics. The ACSM Registered Clinical Exercise Physiologist witnesses change in lived experiences: a stair climb unburdened by exhaustion, an energetic interaction with children, or the rekindling of purpose in retirement. These qualitative shifts epitomize the profundity of sustained, mindful movement. Improved cognition, sleep patterns, and medication reduction further substantiate the pervasive influence of exercise-guided recovery.
Innovations and the Frontier of Clinical Exercise Physiology
Emerging methodologies continue to refine the science of metabolic rehabilitation. High-intensity interval training, neuromuscular stimulation, and personalized genetic insights herald a new era of precision intervention. Yet amidst technological sophistication, the intuitive insight of the ACSM Registered Clinical Exercise Physiologist—translating complex physiology into actionable motion—remains irreplaceable. The synergy of science and human understanding ensures that the art of healing retains its nuance, empathy, and effectiveness.
The Enigmatic Symphony of Brain and Body
The human nervous system is a labyrinthine nexus of electrical impulses, chemical messengers, and sensory feedback loops, orchestrating both voluntary and involuntary movements with exquisite precision. Yet, trauma, neurodegenerative maladies, or prolonged sedentism can perturb this delicate equilibrium, triggering deficits in coordination, cognition, and affective regulation. Within this crucible of vulnerability, the ACSM Registered Clinical Exercise Physiologist emerges as an arbiter of kinetic restoration, translating empirical insights into rehabilitative praxis.
Neuroplasticity: Sculpting the Cerebral Terrain
Neuroplasticity embodies the brain's remarkable proclivity to remodel itself, forging novel synapses and fortifying latent circuits. Exercise operates as an alchemical catalyst, enhancing synaptogenesis, vascular perfusion, and metabolic efficiency. Aerobic exertion propels oxygen-rich blood to cortical and subcortical regions, whereas resistance and proprioceptive modalities amplify motor neuron recruitment and intermuscular coordination. Fine motor drills induce cortical reorganization, while repetitive task engagement consolidates functional connectivity. The ACSM Registered Clinical Exercise Physiologist choreographs these interventions with perspicacity, ensuring each regimen resonates with the patient's evolving neurological landscape.
Cognitive Resonance Through Movement
Neurological compromise often begets cognitive perturbations—attenuated attention spans, impaired working memory, and diminished executive functionality. Integrating cognitive challenges within movement paradigms cultivates dual-domain neuroplasticity. Patients might traverse obstacle-laden pathways while engaging in mnemonic exercises or semantic categorization, reinforcing both motor and cognitive networks. Each session is a delicate interplay between stimulus and adaptation, calibrated meticulously to optimize recovery without overwhelming neural substrates.
Equilibrium and Kinesthetic Refinement
Balance deficits are both a hallmark and a hazard in neurological impairment. The ACSM Registered Clinical Exercise Physiologist employs interventions that elevate proprioceptive acuity, enhance vestibular integration, and refine postural synergy. Tasks may involve dynamic weight shifts, perturbation-based exercises, and destabilized support surfaces. Supervision, assistive devices, and graduated complexity safeguard against iatrogenic injury, while patients gradually internalize confidence in autonomous movement. This amalgamation of neuromuscular precision and psychological empowerment is a cornerstone of functional restoration.
Sensory-Motor Harmonization
Sensory perturbations—diminished tactile perception, vestibular dysfunction, or visual-motor incongruence—can derail motor recovery. Exercises designed to recalibrate multisensory integration bolster neural efficiency and adaptability. Tactile stimulation, visual tracking, and vestibular challenges cultivate a coherent, responsive system. By engaging multiple sensory modalities simultaneously, the ACSM Registered Clinical Exercise Physiologist enhances functional outcomes and mitigates fall risk.
The Pursuit of Functional Autonomy
The apex of neurological rehabilitation is the reclamation of independence in quotidian activities. Simulated tasks—ascending stairs, manipulating utensils, or performing grooming routines—transform therapy into a conduit for autonomy. Structured repetition in a controlled milieu allows neural and muscular systems to recalibrate, fostering both competence and self-efficacy. Success in these domains reverberates beyond the corporeal, reinforcing emotional resilience and a sense of agency.
Psychophysiological Enrichment
Emotional turbulence—anxiety, despondency, or frustration—is endemic in neurological affliction. Exercise serves as a dual-modality intervention, catalyzing neurochemical shifts while reinforcing psychological stability. Elevated endorphin and BDNF levels enhance mood, neurogenesis, and cognitive plasticity. The ACSM Registered Clinical Exercise Physiologist melds empathetic engagement with kinetic therapy, nurturing motivation, and fostering an optimistic trajectory for recovery.
Synergistic Collaboration in Rehabilitation
Neurological rehabilitation is inherently multidisciplinary. Coordination with neurologists, occupational therapists, physical therapists, speech-language pathologists, and psychologists ensures interventions are complementary, not discordant. The exercise physiologist’s domain-specific acumen ensures that movement prescriptions amplify therapeutic outcomes, bridging gaps between medicine, therapy, and lived experience.
Adaptive Modalities and Technological Integration
Complex neurological impairments necessitate adaptive ingenuity. Modified apparatus, assistive devices, robotics, virtual reality, and biofeedback constitute a versatile arsenal. Virtual environments enable risk-free practice of locomotion and obstacle negotiation, while biofeedback provides instantaneous insight into balance, posture, and motor precision. Each technological adjunct is harnessed judiciously, with the physiologist interpreting data to fine-tune interventions for maximal neurofunctional engagement.
Iterative Assessment and Program Modulation
Neurological recovery is nonlinear, a mosaic of progression and plateau. Continuous assessment—spanning fatigue, cognitive engagement, and motor performance—ensures interventions remain optimally calibrated. Real-time adjustments preserve efficacy, prevent overtraining, and sustain motivation. Rigorous documentation facilitates interprofessional communication, supporting dynamic recalibration of therapeutic trajectories and pharmacological management.
Sustaining Gains and Mitigating Decline
The cessation of formal rehabilitation does not signify recovery’s terminus. Longitudinal maintenance strategies—home exercise regimens, community-based fitness participation, and ongoing neurocognitive engagement—cement functional gains. Patients are equipped with self-monitoring techniques and adaptive heuristics, transforming recovery from a clinician-directed endeavor into an autonomous, lifelong praxis. This continuum safeguards against regression and optimizes neurophysiological resilience.
Pioneering Horizons in Neurorehabilitation
Emergent research illuminates novel avenues for exercise-driven neural restitution. Wearable biosensors, tele-rehabilitation platforms, and advanced neuroimaging expand the precision of individualized intervention. Yet, despite technological sophistication, the nuanced discernment, empathetic guidance, and adaptive ingenuity of the ACSM Registered Clinical Exercise Physiologist remain irreplaceable. Human intuition and experiential judgment orchestrate recovery in ways no device can emulate, ensuring that each patient’s journey is both scientifically grounded and profoundly personalized.
The Architecture of Musculoskeletal Resilience
The human musculoskeletal apparatus is an intricate latticework of bones, tendons, ligaments, and musculature, orchestrating the symphony of movement. Disruption to this architecture through trauma, degeneration, or repetitive strain fractures the harmony of mobility. The ACSM Registered Clinical Exercise Physiologist functions as both cartographer and conductor of this complex system, mapping weaknesses, recalibrating imbalances, and cultivating kinetic fluency. Recovery is not a mere return to baseline; it is an elevation of functional aptitude, where strength, flexibility, and coordination are meticulously interwoven.
Precision in Injury Remediation
Orthopedic afflictions, whether ligamentous tears, articular fissures, or post-surgical limitations, demand strategic intervention. The Clinical Exercise Physiologist meticulously engineers progressive regimens that reintroduce movement through graded exposure, controlled resistance, and adaptive neuromuscular engagement. Initial exercises prioritize joint lubrication, muscular activation, and proprioceptive acuity, evolving toward complex, functionally aligned tasks that mirror quotidian demands. The interplay of biomechanical insight and patient feedback ensures that recovery is measurable, safe, and psychologically affirming.
Strength Harmonization and Postural Equilibrium
Muscular asymmetry and joint instability are endemic to musculoskeletal compromise. The Clinical Exercise Physiologist employs exercises that recalibrate these disparities, emphasizing core integrity, kinetic chain synchronization, and postural refinement. Strategies may include dynamic stabilization drills, proprioceptive challenges, and flexibility augmentation, all designed to attenuate compensatory patterns. For example, a post-knee arthroplasty patient may engage in multi-planar squats, hip abductive resistance, and proprioceptive balance sequences, each iteration enhancing neuromuscular synergy while safeguarding joint integrity.
Analgesic Properties of Motion
Chronic musculoskeletal conditions, including osteoarthritic degeneration or persistent lumbar discomfort, reveal the analgesic potential of structured exercise. Through orchestrated loading, targeted strengthening, and posture correction, exercise diminishes nociceptive stimuli while enhancing circulation and neuromuscular efficiency. Interventions integrate aerobic conditioning, resistive exercises, and mobility routines to attenuate inflammation and recalibrate musculoskeletal signaling pathways. The outcome is not solely physical amelioration but the cultivation of self-efficacy, autonomy, and corporeal confidence.
Functional Reclamation of Daily Living
True rehabilitation transcends clinical metrics; it manifests in the reclamation of quotidian competence. The Clinical Exercise Physiologist crafts exercises that replicate functional tasks such as lifting, stair negotiation, and rotational bending. This pragmatic approach ensures that strength and flexibility translate into tangible independence. Adaptive strategies are implemented to accommodate limitations, reinforcing capability and resilience while minimizing risk. Each progressive milestone fortifies both physical restoration and cognitive assurance, cementing the patient’s trust in their rehabilitated body.
Interdisciplinary Synergy
Musculoskeletal restoration rarely occurs in isolation. The Clinical Exercise Physiologist engages in a collaborative dialogue with orthopedic surgeons, physical therapists, and occupational specialists, harmonizing exercise prescriptions with medical directives. Continuous data acquisition and performance monitoring enable iterative adjustment, ensuring interventions are both precise and holistic. Through this symbiosis, exercise transcends therapy; it becomes an integral conduit for coordinated clinical care.
Prophylaxis and Lifelong Mobility
Recovery is but a prologue to sustained musculoskeletal health. The Clinical Exercise Physiologist imparts strategies for long-term preservation, including strength maintenance, flexibility routines, postural vigilance, and ergonomic literacy. Patients are empowered to detect early strain, integrate dynamic movement into routines, and employ adaptive modifications, establishing a paradigm where exercise functions as both rehabilitative and preventive medicine. This ethos of anticipatory care fosters enduring autonomy and mitigates future injury risk.
Psychophysiological Integration
Musculoskeletal disruption invariably affects the psyche, generating apprehension, frustration, and diminished self-efficacy. Exercise prescription, under the guidance of a Clinical Exercise Physiologist, operates as a dual conduit: rehabilitating physical function while fostering mental resilience. Encouragement, milestone acknowledgment, and structured goal progression transform rehabilitation into a holistic experience, where neurochemical and psychological reinforcement coalesce to optimize recovery outcomes.
Technological Augmentation in Rehabilitation
Innovative tools have expanded the horizons of musculoskeletal therapy. Motion capture systems, wearable kinematic sensors, and biofeedback mechanisms enable precise quantification of movement patterns, muscle activation, and postural dynamics. Emerging modalities, including robotic-assisted training and virtual reality-enhanced neuromotor retraining, allow for sophisticated rehabilitation of complex injuries. Despite technological sophistication, the Clinical Exercise Physiologist’s clinical discernment remains paramount, ensuring that interventions are not only empirically guided but also patient-centric and adaptable.
Evolution of Therapeutic Exercise Paradigms
Exercise has evolved from simplistic strength routines into a nuanced therapeutic modality encompassing neuroplasticity, biomechanical precision, and psychosocial reinforcement. The Clinical Exercise Physiologist synthesizes these dimensions, crafting regimens that are simultaneously curative, preventative, and performance-enhancing. This evolution embodies the principle that human movement is not merely mechanical but a dynamic interplay of physiology, cognition, and emotion.
Holistic Wellness and the Confluence of Bodily Systems
Holistic wellness transcends the mere absence of disease, embracing an intricate symphony of physiological, psychological, and environmental harmonics. It acknowledges that the human organism is an intricate constellation, where cardiovascular vigor, neuromuscular integrity, endocrine balance, and cognitive acuity interlace in dynamic interplay. The ACSM Registered Clinical Exercise Physiologist serves as a cartographer of this terrain, navigating the labyrinthine interactions between body systems and lifestyle factors, orchestrating interventions that transcend the reductionist paradigm of conventional care. By mapping the individual’s unique physiological topography, these professionals cultivate a state of functional congruence that fosters resilience, adaptability, and vitality.
Exercise as a Therapeutic Modality in Chronic Conditions
Chronic disease management demands more than episodic care; it necessitates deliberate, sustained interventions that recalibrate systemic physiology. Exercise emerges as a potent therapeutic modality, capable of ameliorating metabolic derangements, attenuating inflammatory cascades, and enhancing cardiopulmonary efficiency. The ACSM Registered Clinical Exercise Physiologist designs bespoke programs, interweaving aerobic, resistance, neuromotor, and flexibility modalities to address the idiosyncratic demands of each patient. These interventions are not monolithic; they evolve in response to longitudinal monitoring, ensuring that intensity, volume, and modality harmonize with the patient’s adaptive trajectory, mitigating risk while maximizing functional gains.
Neuropsychological Fortification Through Movement
The burden of chronic illness extends beyond corporeal manifestations, often manifesting as affective dysregulation, cognitive perturbation, and existential disquiet. The ACSM Registered Clinical Exercise Physiologist integrates psychophysiological strategies that cultivate neuropsychological fortitude. Mindful kinetic practices, motivational scaffolding, and structured goal-setting serve as conduits for self-efficacy and emotional resilience. Physical activity itself elicits neurochemical cascades, augmenting dopaminergic, serotonergic, and neurotrophic activity, thereby enhancing mood, cognitive clarity, and stress modulation. Through this integrative lens, movement becomes an agent not merely of physical restoration but of mental and emotional alchemy.
Pedagogy of Empowerment and Self-Efficacy
Central to holistic intervention is the pedagogy of empowerment. Patients are not passive recipients of prescriptive regimens; they are co-conspirators in their wellness odyssey. The ACSM Registered Clinical Exercise Physiologist equips individuals with the acumen to decipher physiological feedback, calibrate exertion, and implement adaptive strategies independently. Mastery of these skills cultivates agency, transforming exercise from a transactional chore into an autonomous, self-sustaining habit. The emphasis on self-efficacy engenders adherence, fosters enduring lifestyle metamorphosis, and embeds wellness within the fabric of daily life.
Integrative Synergy with Multidisciplinary Care
Optimal wellness necessitates a confluence of expertise across multiple healthcare domains. The ACSM Registered Clinical Exercise Physiologist functions as a nexus within multidisciplinary teams, ensuring exercise prescriptions dovetail seamlessly with pharmacological regimens, nutritional protocols, and psychosocial interventions. This integrative synergy amplifies therapeutic efficacy, promoting systemic homeostasis and functional restoration. Lifestyle modifications, including sleep hygiene, stress mitigation, and alimentary optimization, are embedded into exercise programming, producing a holistic, interconnected approach to chronic disease management that is both pragmatic and scientifically grounded.
Community Engagement and Preventive Paradigms
Holistic wellness extends beyond the individual, encompassing the collective milieu. ACSM Registered Clinical Exercise Physiologists spearhead community-based initiatives, corporate wellness programs, and public health campaigns that democratize access to movement and education. By fostering environments that valorize physical activity and preventive health, they reduce disease incidence, enhance communal vitality, and cultivate societal resilience. These initiatives serve as catalysts for behavioral transformation, engendering cultural shifts where healthful practices become normative, accessible, and sustainable.
Technological Augmentation in Clinical Practice
In the era of digital proliferation, technology functions as an extension of clinical acumen. Wearable biosensors, telehealth platforms, and analytic software enable real-time surveillance of adherence, performance, and physiological response. The ACSM Registered Clinical Exercise Physiologist harnesses these tools to fine-tune programming, ensuring individualized interventions remain responsive to fluctuating health indices. Advanced data analytics facilitate predictive modeling, allowing proactive modifications that preempt exacerbations, optimize performance, and enhance patient engagement. Technology thus becomes a conduit through which precision, accessibility, and longitudinal oversight converge.
Lifespan Longevity and Functional Flourishing
The ultimate aspiration of holistic exercise intervention is not merely disease mitigation but the cultivation of lifespan longevity, functional flourishing, and existential vitality. By integrating therapeutic, preventive, and rehabilitative strategies, the ACSM Registered Clinical Exercise Physiologist empowers individuals to navigate the vicissitudes of aging with agency, strength, and grace. Functional independence, mobility, cardiovascular robustness, and neurocognitive acuity are preserved and enhanced, enabling individuals to engage fully with life’s multifaceted dimensions. Movement becomes an instrument of vitality, resilience, and transcendence, embedding wellness into the continuum of lived experience.
The Subtle Architecture of Cardiovascular Resilience
The human heart, a ceaseless metronome of vitality, does more than circulate blood; it orchestrates a symphony of cellular resonance and systemic coherence. When cardiovascular integrity is compromised, the body enters a state of precarious imbalance. In this arena, the ACSM Registered Clinical Exercise Physiologist emerges as both architect and custodian of restoration, translating scientific insight into deliberate motion. Their practice is a choreography of exertion and recuperation, calibrated to awaken dormant capacities while honoring the fragility inherent in post-illness physiology.
The heart’s recovery is neither abrupt nor linear. Each contraction, each nuanced shift in arterial pressure, represents a negotiation between vulnerability and fortitude. The physiologist’s task is to facilitate this negotiation, fostering adaptive remodeling that extends beyond myocardial tissue to encompass the autonomic, endocrine, and psychological landscapes. In these meticulously crafted interventions, the principles of hemodynamics and cellular energetics converge, revealing exercise not merely as movement but as a profound therapeutic vector.
Cardiac Rejuvenation Through Deliberate Motion
Following myocardial insult, whether through infarction, surgical intervention, or ischemic insult, the myocardium exhibits a delicate plasticity. The ACSM Registered Clinical Exercise Physiologist harnesses this plasticity through tailored exercise regimens that prioritize gradation and specificity. Movement becomes an instrument of regeneration, enhancing perfusion, promoting angiogenesis, and reinforcing contractile efficiency without provoking maladaptive strain.
Aerobic engagement, in measured intervals, stimulates capillary proliferation and mitochondrial amplification. Even subtle exertion, such as slow ambulation or gentle cycling, catalyzes biochemical cascades that mitigate oxidative stress and temper inflammatory mediators. The physiologist monitors these processes through meticulous metrics, interpreting heart rate variability, oxygen uptake kinetics, and perceived exertion to ensure that each session is both restorative and instructive. Recovery is reframed as a conversation between patient and physiology, mediated by guided movement.
The Invisible Currents of Emotional Reconstitution
Physical healing in cardiovascular rehabilitation is invariably entwined with emotional recalibration. Anxiety, apprehension, and hypervigilance toward bodily sensations often accompany post-cardiac vulnerability. Here, the ACSM Registered Clinical Exercise Physiologist interlaces pedagogy with kinesthetic practice. Patients are educated on the mechanistic benefits of controlled exertion, cultivating a cognitive framework wherein activity is reframed as an ally rather than a threat.
Trust forms the substratum of this process. Within supervised sessions, patients confront their fears in incremental doses, observing physiological responses in real time. The act of navigating exertional thresholds without adverse events instills an embodied assurance that ripples into daily life. The physiologist’s guidance becomes a scaffold for both cardiac and psychological fortification, demonstrating that resilience is as much an internalized narrative as it is a functional metric.
Integrative Symbiosis of Science and Sensibility
Clinical exercise physiology is predicated upon a delicate synthesis of quantitative assessment and qualitative intuition. The ACSM Registered Clinical Exercise Physiologist interprets electrocardiographic fluctuations, blood-pressure oscillations, and metabolic indices, yet simultaneously attends to subjective accounts of fatigue, breathlessness, and affective state. This dual attention transforms sterile clinical spaces into laboratories of human experience, where the data illuminate patterns and the patient’s story provides context.
Milestone achievements—extended ambulation, stair navigation, or light resistance work—are celebrated not only for their physiological significance but for their symbolic affirmation of recuperative agency. In this integrative praxis, science and empathy coalesce, creating a therapeutic environment where the body’s adaptations are mirrored by the psyche’s recovery. The physiologist thus becomes both investigator and advocate, translating numbers into narrative and exertion into empowerment.
Multidimensional Collaboration in Rehabilitation
Healing the heart extends beyond muscular or vascular considerations; it necessitates a multidisciplinary alliance. The ACSM Registered Clinical Exercise Physiologist collaborates with cardiologists, nurses, nutritionists, and mental-health specialists to construct a tapestry of holistic rehabilitation. Exercise prescriptions are interwoven with dietary guidance, pharmacologic adherence, and stress-modulation strategies, producing synergistic gains that transcend isolated interventions.
Within rehabilitation centers, meticulous records chart progress, flag anomalies, and guide iterative adjustments. The physiologist’s analytical acumen ensures that adaptations remain within safe physiological thresholds, optimizing recovery velocity while minimizing risk. This collaborative orchestration underscores the recognition that cardiovascular restoration is neither singular nor linear, but an emergent property of integrated, responsive care.
Cellular Mechanisms of Adaptive Renewal
At a microscopic level, exercise orchestrates a renaissance within myocardial and vascular tissues. Repetitive, controlled loading amplifies stroke volume, augments endothelial function, and fosters mitochondrial proliferation. Inflammatory mediators are downregulated, and neurohormonal pathways recalibrate toward homeostasis. The ACSM Registered Clinical Exercise Physiologist leverages these molecular responses, designing regimens that target precise functional deficits while promoting systemic equilibrium.
The principle of specificity guides each intervention. Interval walking, resistance training with minimal load, or rhythmic aquatic activity is prescribed not arbitrarily but to elicit targeted physiological adaptations. Vigilant monitoring ensures that stimuli remain constructive, enabling the patient’s cardiovascular system to acquire resilience without incurring deleterious stress. Each session is an iterative dialogue between biology and practice, an exercise in both precision and patience.
Social Reintegration Through Guided Vitality
Cardiac convalescence extends beyond the clinical environment into social and communal contexts. The ACSM Registered Clinical Exercise Physiologist equips patients with self-monitoring acumen, teaching recognition of safe exertion limits and bodily signals. Community programs, walking groups, and adaptive sport initiatives translate rehabilitative gains into enduring lifestyle habits, cultivating both physical capacity and social connectedness.
These interventions foster not only endurance but also autonomy. Patients internalize principles of pacing, recovery, and incremental challenge, transforming movement from a prescribed duty into an experiential and communal pursuit. Social engagement amplifies adherence, reinforces identity reconstruction, and mitigates the isolation that often shadows post-cardiac convalescence.
Psychological Resonance of Kinetic Therapy
Movement, when guided with precision, becomes a conduit for psychological transformation. Exercise mitigates depressive symptoms, reduces anxiety, and fosters cognitive clarity among cardiovascular patients. The ACSM Registered Clinical Exercise Physiologist integrates mindfulness, breath regulation, and progressive goal-setting into each session, cultivating an experiential awareness that complements physiological gains.
The repeated experience of controlled exertion affirms self-efficacy, creating a feedback loop in which bodily capability reinforces mental resilience. Patients emerge from rehabilitation not merely restored but reconceptualized, perceiving their corporeal and cognitive capacities as resilient and responsive rather than fragile and constrained.
Technological Augmentation of Clinical Insight
Emergent technologies have magnified the precision and reach of cardiac rehabilitation. Wearable monitors, telemetric sensors, and remote data analytics enable the ACSM Registered Clinical Exercise Physiologist to track heart rate, oxygen saturation, and hemodynamic variability continuously. These tools provide early detection of aberrant responses and facilitate intervention before complications arise.
Telehealth platforms extend guidance beyond physical proximity. Patients receive real-time feedback, encouragement, and adaptive programming even when geographically distant from clinical facilities. The fusion of digital oversight with human expertise exemplifies a new paradigm in which empirical data and empathic instruction converge to optimize recovery.
Preventive Kinetics and Lifelong Cardiovascular Stewardship
Exercise in cardiac rehabilitation naturally evolves into a preventive strategy. Once recuperation stabilizes, patients are empowered to sustain and amplify gains through habitual, moderated activity. The ACSM Registered Clinical Exercise Physiologist instructs on lifelong kinetic stewardship, emphasizing the maintenance of cardiovascular integrity, metabolic balance, and functional independence.
Community initiatives, educational seminars, and public health collaborations extend the reach of rehabilitative knowledge, transforming individual recovery into collective vitality. The principle remains singular yet profound: deliberate, sustained movement is the most reliable instrument of cardiac preservation, translating complex biological principles into accessible, actionable practice.
Reawakening Rhythmic Vitality
The journey of cardiac healing encompasses both the corporeal and the existential. Patients traverse a continuum from trepidation to empowerment, guided by the ACSM Registered Clinical Exercise Physiologist whose interventions harmonize scientific rigor with humanistic sensitivity. Each heartbeat, each incremental exertion, becomes a testament to adaptive resilience, a living chronicle of physiological and emotional restoration.
Through meticulously structured exercise, patients regain not only cardiovascular competence but also the confidence to navigate the unpredictabilities of daily life. Walking evolves into cycling, light resistance into functional mobility, and the physiological narrative is mirrored by renewed autonomy and self-assurance. Exercise thus transforms into a medium of reclamation—a rhythm of vitality that resonates through body, mind, and community.
Cardiac Remodeling and Adaptive Resilience
The human heart, a ceaselessly pulsating organ, responds to perturbation with an intricate interplay of structural remodeling and functional adaptation. Post-infarction, hypertensive stress, or cardiomyopathic changes demand careful orchestration of therapeutic movement. The ACSM Registered Clinical Exercise Physiologist functions as both a cartographer and a conductor, mapping cardiovascular vulnerabilities and prescribing interventions that elicit favorable remodeling.
Exercise-induced shear stress augments endothelial function, enhancing nitric oxide bioavailability and promoting vascular compliance. Low- to moderate-intensity aerobic activity fosters cardiac efficiency by optimizing stroke volume and attenuating maladaptive hypertrophy. Simultaneously, controlled resistance training strengthens ancillary musculature, improving peripheral perfusion and reducing cardiac workload. This duality—central cardiac adaptation paired with peripheral enhancement—underscores the physiologist’s capacity to translate abstract physiological principles into tangible patient progress.
The Psychophysiology of Recovery
Cardiac rehabilitation is as much a psychophysiological endeavor as it is anatomical. Anxiety, depressive symptomatology, and fear of exertion frequently accompany myocardial insult, creating barriers to functional progression. Exercise functions as a bidirectional conduit, simultaneously bolstering autonomic stability and fortifying psychological resilience.
Aerobic engagement modulates heart rate variability, reflecting improved parasympathetic tone, while resistance modalities stabilize metabolic control and attenuate systemic inflammation. Endorphin surges and increased production of brain-derived neurotrophic factor (BDNF) enhance mood and cognitive clarity, creating a feedback loop wherein physiological recovery fosters emotional equanimity. Patients gradually internalize their capacity for exertion, shifting from a paradigm of vulnerability to one of empowered agency.
Metabolic Synchrony and Energy Economy
A pivotal aspect of cardiac rehabilitation involves optimizing metabolic efficiency. Post-cardiac event, patients often experience dysregulated glucose metabolism, lipid abnormalities, and reduced mitochondrial density. The ACSM Registered Clinical Exercise Physiologist deploys a multifaceted regimen that stimulates oxidative capacity, enhances insulin sensitivity, and refines substrate utilization.
High-repetition, low-load resistance protocols augment muscular mitochondrial density, while interval aerobic sessions improve maximal oxygen consumption and endothelial responsiveness. By recalibrating the energy economy, these interventions reduce the energetic cost of routine tasks, from ascending stairs to performing household activities. Each incremental gain in metabolic efficiency reverberates through the patient’s daily existence, reinforcing autonomy and sustaining engagement with rehabilitative strategies.
Cardiopulmonary Integration
The heart does not operate in isolation; it is entwined with the lungs, vasculature, and peripheral musculature in a sophisticated symphony of cardiopulmonary integration. The ACSM Registered Clinical Exercise Physiologist facilitates this integration through graded aerobic conditioning, interval-based exertion, and respiratory-focused interventions.
Breathing mechanics, often overlooked, are refined to improve oxygen uptake and CO2 clearance. Inspiratory muscle training enhances ventilatory efficiency, while postural alignment exercises support diaphragmatic excursion and thoracic expansion. These subtle yet potent modifications contribute to overall cardiovascular efficiency, ensuring that the system operates as a cohesive, synchronized entity rather than a collection of discrete organs.
Exercise as a Chronobiological Modulator
Cardiac recovery is influenced not only by intensity and duration of activity but also by temporal rhythms. Circadian and ultradian cycles modulate autonomic tone, hormonal secretion, and vascular responsiveness. The ACSM Registered Clinical Exercise Physiologist leverages these chronobiological insights, prescribing sessions during optimal windows for heart rate control, blood pressure stability, and metabolic responsiveness.
Aligning exercise with intrinsic physiological rhythms enhances both efficacy and adherence. Patients experience less fatigue, improved cardiovascular response, and greater psychological receptivity to interventions. This chronobiological attunement transforms the act of exercise from a mechanical prescription into a harmonious alignment with the body’s internal cadence.
Hemodynamic Mastery
Effective cardiac rehabilitation demands vigilant attention to hemodynamic parameters. Blood pressure, heart rate, cardiac output, and vascular resistance must be continuously monitored to prevent deleterious strain. The ACSM Registered Clinical Exercise Physiologist employs sophisticated assessment tools and real-time observation to calibrate exercise intensity, ensuring that each session provokes adaptation without precipitating ischemic or arrhythmic events.
Gradual progression in workload, coupled with interval monitoring, cultivates hemodynamic resilience. Patients regain the capacity for sustained activity without symptomatic compromise, reinforcing confidence and supporting long-term functional independence.
Neuromuscular Coordination and Functional Reintegration
Cardiovascular recovery is inseparable from neuromuscular re-education. Fatigue, deconditioning, and post-event muscular atrophy compromise movement economy, heightening the risk of injury. Structured functional exercises, incorporating gait training, core stabilization, and dynamic balance, restore biomechanical efficiency.
Resistance training is integrated not merely for strength but for synergistic coordination, enhancing muscle recruitment patterns and intermuscular timing. Patients progress from supported ambulation to dynamic functional tasks, regaining the fluidity and confidence necessary for daily life. This reintegration exemplifies the ACSM Registered Clinical Exercise Physiologist’s holistic approach, wherein cardiovascular, musculoskeletal, and proprioceptive systems are rehabilitated in concert.
Psychosocial Embodiment and Community Reconnection
Healing extends beyond the somatic realm into the psychosocial dimension. Social isolation, post-event fear, and disrupted routines often accompany cardiac pathology. The physiologist cultivates community and accountability through group sessions, mentorship programs, and structured peer interactions. These communal frameworks provide emotional scaffolding, normalize recovery experiences, and encourage sustained participation.
Moreover, the psychosocial reinforcement inherent in guided exercise—encouragement, achievement acknowledgment, and shared milestones—bolsters self-efficacy. Patients internalize a renewed sense of agency, perceiving not merely the absence of pathology but the presence of possibility.
Adaptive Interventions for Diverse Cardiac Pathologies
Cardiac pathology is heterogeneous. Coronary artery disease, heart failure, arrhythmias, and valvular disorders each necessitate bespoke intervention strategies. The ACSM Registered Clinical Exercise Physiologist evaluates each patient’s hemodynamic tolerance, arrhythmic susceptibility, and functional reserve to craft individualized programs.
For heart failure patients, low-intensity interval training combined with resistance exercise minimizes exertional dyspnea while augmenting stroke volume. For post-infarction patients, graded aerobic progression alongside neuromuscular re-education enhances perfusion and reduces ischemic risk. Across all pathologies, interventions are meticulously titrated to elicit adaptation while safeguarding patient safety.
Integrating Technology and Biofeedback
Modern cardiac rehabilitation increasingly incorporates technological adjuncts. Wearable monitors, heart rate variability sensors, and telemetry systems provide instantaneous feedback on physiological responses. Virtual reality modules simulate environmental challenges, allowing patients to practice activities of daily living with real-time physiological tracking.
The ACSM Registered Clinical Exercise Physiologist synthesizes this information to refine intensity, monitor fatigue, and optimize adaptation. Technology augments human expertise rather than replacing it, transforming data into actionable insights and elevating patient engagement.
Longitudinal Monitoring and Sustained Health
Cardiac rehabilitation is not ephemeral. Long-term maintenance, encompassing home-based exercise, dietary guidance, stress modulation, and lifestyle integration, preserves gains and mitigates recurrence risk. The physiologist educates patients on self-monitoring strategies, adaptive modifications, and contingency planning for periods of illness or travel.
These practices cultivate autonomy, embedding recovery into the patient’s daily existence rather than confining it to clinical spaces. The result is a sustainable rhythm of vitality, a lifelong dialogue between body, mind, and environment.
The Interplay of Emotion and Physiology
Emotion and physiology are inseparable in cardiac recovery. Anxiety, frustration, or depression can compromise autonomic regulation, vascular tone, and adherence to therapy. The ACSM Registered Clinical Exercise Physiologist addresses these dimensions through empathetic communication, motivational interviewing, and paced exposure to exertion.
Patients learn to interpret bodily signals accurately, distinguishing adaptive fatigue from maladaptive distress. This interoceptive literacy enhances self-efficacy and fosters resilience, allowing individuals to navigate daily challenges with poise and confidence.
Nutritional Synergy and Metabolic Support
Exercise alone is insufficient for optimal cardiac recovery. Nutritional strategies amplify adaptation, modulate inflammation, and support energy balance. Anti-inflammatory dietary components, balanced macronutrient intake, and timed nutrient consumption synergize with exercise-induced metabolic adaptations.
The physiologist integrates nutritional guidance into the rehabilitative framework, collaborating with dietitians and healthcare providers. Patients learn to view food as an adjunct to recovery, enhancing both physical function and cognitive clarity.
Forward Horizons in Cardiac Rehabilitation
Emergent research elucidates novel mechanisms of adaptation, from mitochondrial biogenesis to autonomic recalibration. Tele-rehabilitation platforms expand access, while wearable technology provides continuous physiological insight. Despite these advances, the ACSM Registered Clinical Exercise Physiologist remains the linchpin of personalized care.
Human discernment, intuition, and adaptability ensure that interventions are nuanced, responsive, and deeply individualized. The future of cardiac rehabilitation is not merely technological but profoundly human, leveraging science and empathy in equal measure.
Conclusion
The journey through healing and wellness demonstrates that exercise is far more than a routine or a fitness goal; it is a profound agent of restoration and resilience. From cardiovascular recovery to metabolic regulation, neurological rehabilitation, musculoskeletal restoration, and holistic wellness, the ACSM Registered Clinical Exercise Physiologist serves as both guide and advocate, translating scientific knowledge into individualized, life-changing interventions.
Throughout each part of this series, it becomes clear that recovery and health are multidimensional. The ACSM Registered Clinical Exercise Physiologist not only addresses physical deficits but also nurtures emotional well-being, cognitive function, and patient empowerment. Their work transforms fear into confidence, limitation into capability, and injury or illness into opportunity for growth.
At the core of their practice lies a simple yet powerful principle: movement is medicine. By designing safe, evidence-based exercise programs tailored to each individual, the physiologist unlocks the body’s innate capacity to heal and adapt. They monitor progress meticulously, adjust interventions dynamically, and provide encouragement that fosters long-term adherence and sustainable lifestyle change.
Moreover, the reach of the ACSM Registered Clinical Exercise Physiologist extends beyond clinical settings. Through community programs, educational initiatives, and preventive strategies, they influence public health, promote wellness, and cultivate a culture where movement is recognized as essential for life, not optional.
In a world where chronic disease, injury, and sedentary lifestyles pose significant challenges, the ACSM Registered Clinical Exercise Physiologist stands as a beacon of hope. Their expertise bridges science and compassion, clinical knowledge and practical application, ensuring that each patient not only recovers but thrives.
Ultimately, the impact of the ACSM Registered Clinical Exercise Physiologist is transformative. They empower individuals to reclaim independence, restore function, and achieve holistic wellness. Each session, each exercise, each guided step embodies the profound truth that the body, when properly supported, can heal, adapt, and flourish.
Through their work, exercise becomes more than movement; it becomes a pathway to life, vitality, and renewed possibility. The ACSM Registered Clinical Exercise Physiologist is not just a professional—they are a partner in the ongoing journey toward health, resilience, and the full expression of human potential.
Frequently Asked Questions
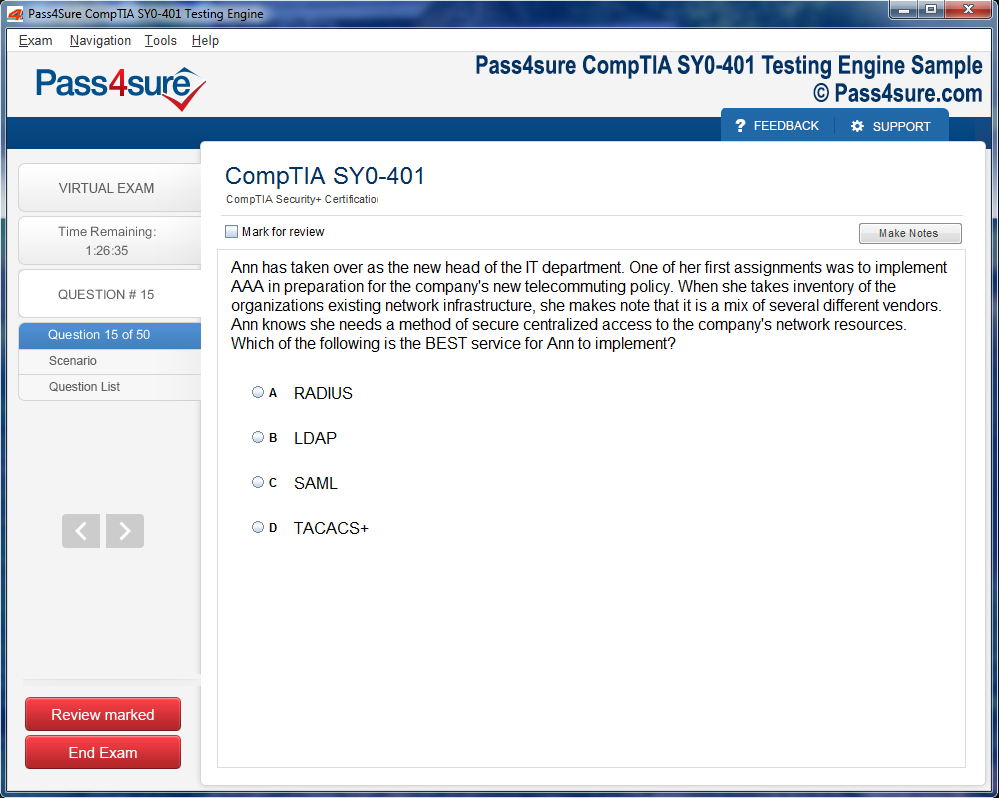
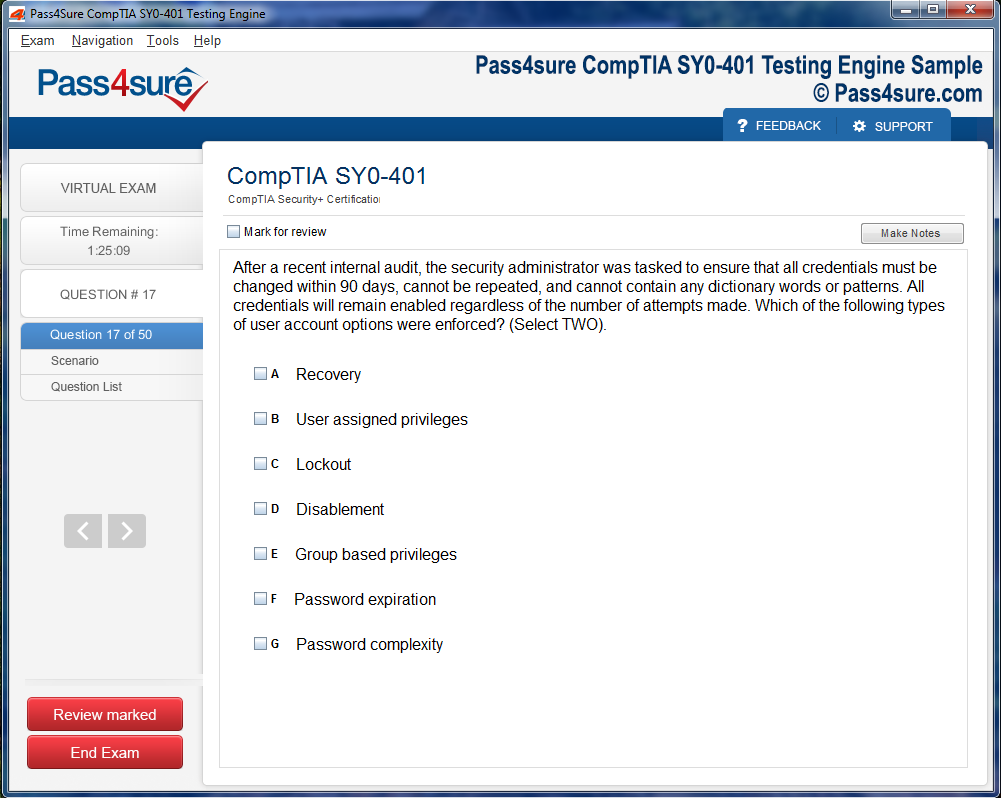
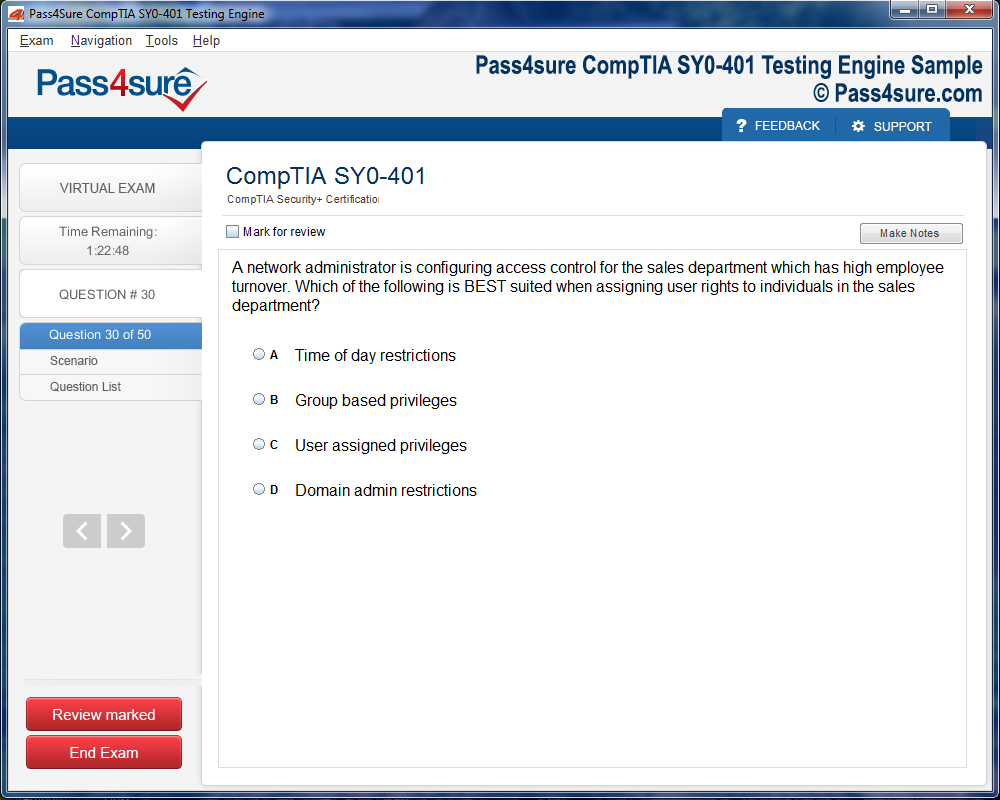
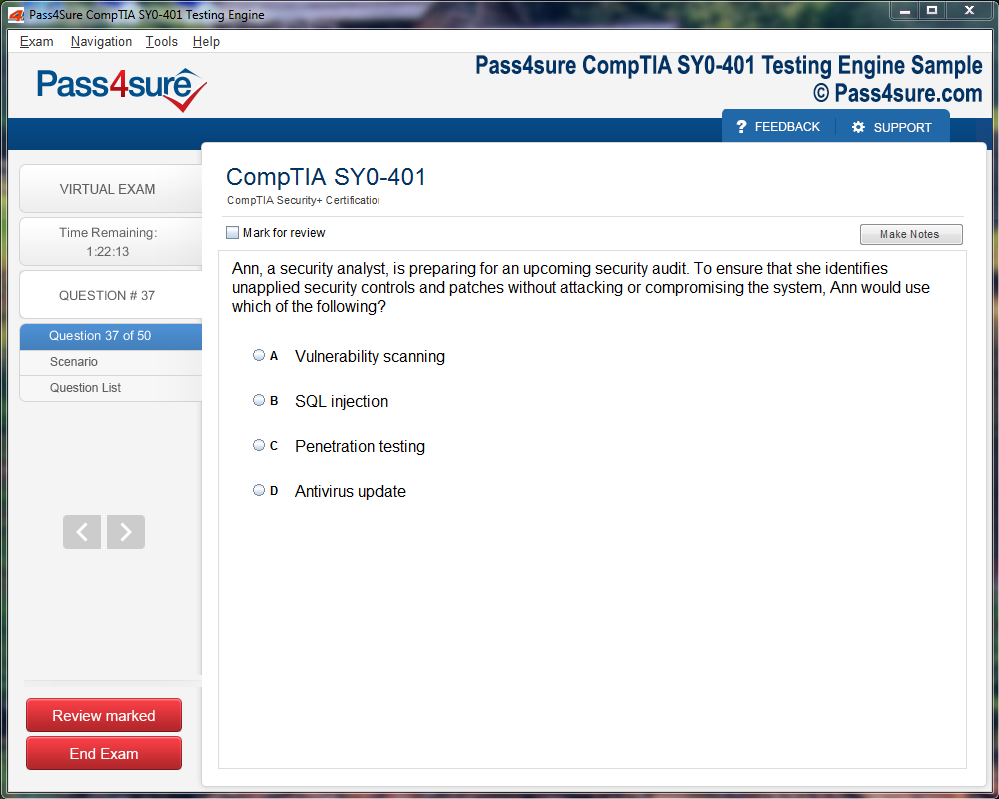
How does your testing engine works?
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations).
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.