Test Name: NBRC - National Board for Respiratory Care
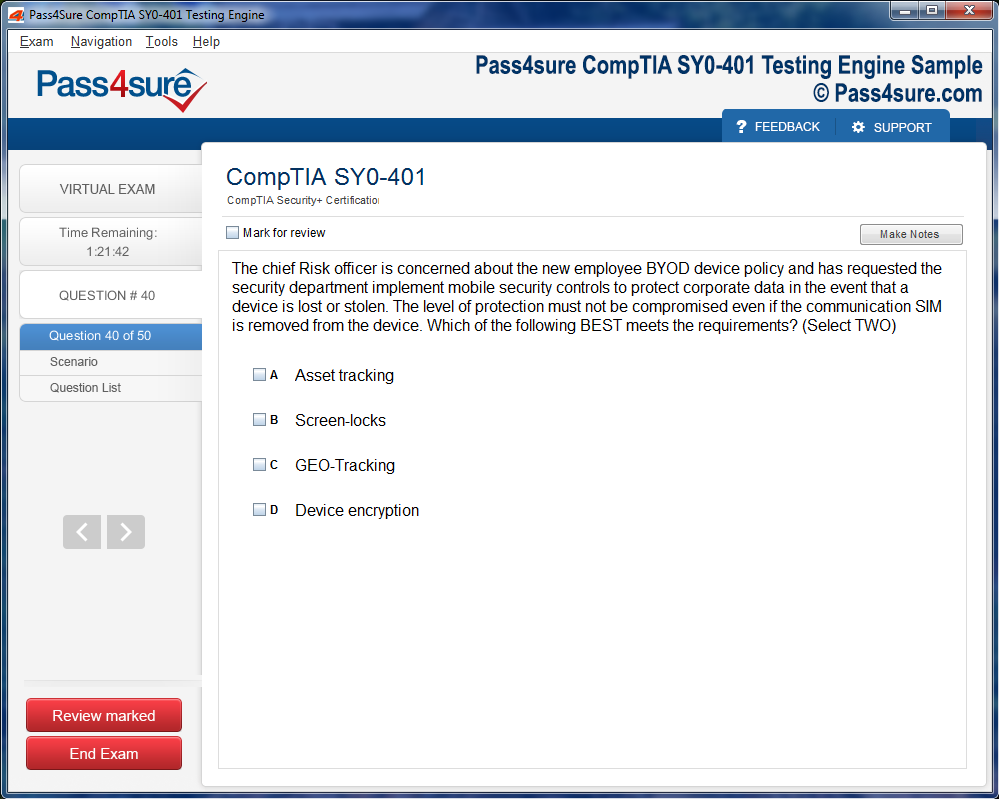
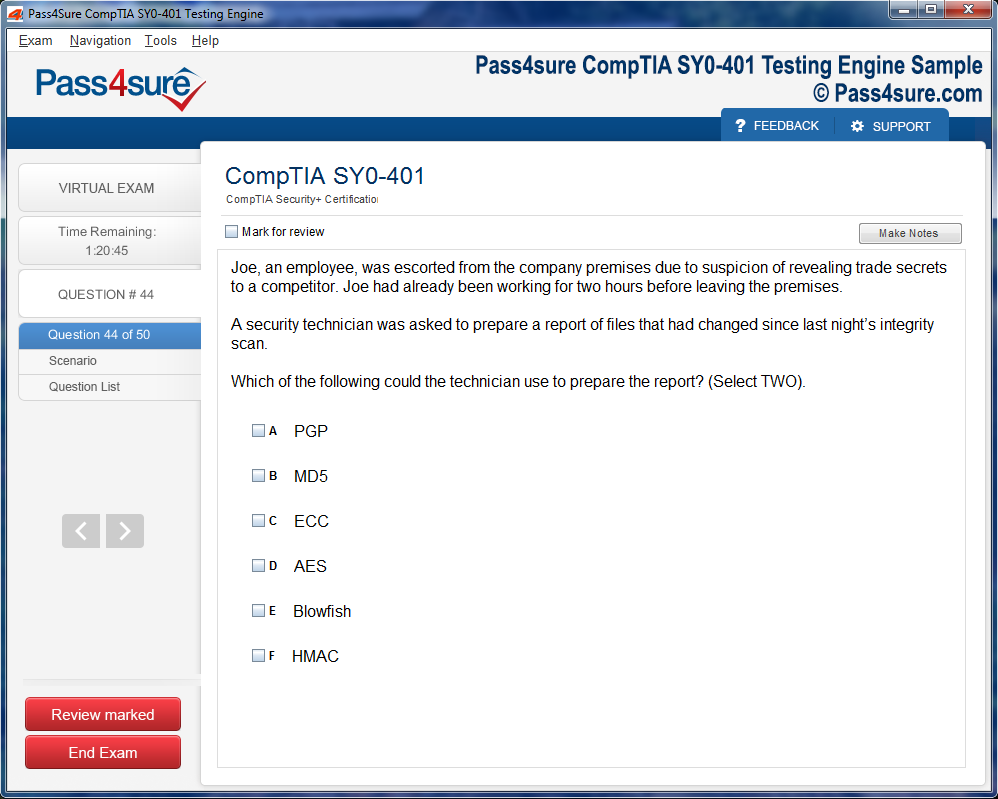
Product Screenshots
Navigating NBRC Credentialing Challenges: The Complete Guide
The journey toward successful NBRC credentialing demands a strategic and layered approach to preparation. Candidates must cultivate a framework that balances cognitive absorption, skill application, and time efficiency. Strategic preparation is not merely about memorizing facts; it is an intricate process that intertwines comprehension, repetition, and contextual application. Effective preparation begins with an honest assessment of one’s strengths and weaknesses, allowing learners to allocate time and effort where gaps exist most prominently.
An essential component of strategic preparation involves creating a structured study plan that respects cognitive rhythms. Learning in concentrated intervals, interspersed with reflection and practical exercises, enhances memory retention and conceptual clarity. The NBRC examinations require proficiency not only in theoretical knowledge but also in critical thinking under pressure. Therefore, candidates benefit from simulated practice scenarios that replicate clinical encounters, laboratory procedures, and patient interactions. These exercises cultivate a sense of familiarity and confidence, reducing performance anxiety during actual examinations.
Equally important is the selection of study materials and resources. While conventional textbooks provide foundational knowledge, candidates gain an edge by integrating multi-modal learning tools. Visual aids, interactive simulations, and case-based discussions foster deeper understanding, especially in complex topics such as pulmonary pathophysiology or ventilator management. Engaging with peers and mentors further enhances comprehension, as collaborative learning exposes one to alternative perspectives and problem-solving strategies. This diversity in approach prevents monotony, promotes analytical thinking, and nurtures adaptability—qualities indispensable for clinical excellence.
Moreover, time management emerges as a critical determinant of success. Candidates must juggle professional responsibilities with rigorous study schedules, necessitating disciplined allocation of hours and meticulous prioritization. Tracking progress through self-assessment quizzes, timed mock tests, and reflective journals provides measurable insights into readiness levels. Strategic preparation, therefore, is not a linear pursuit; it is an iterative process of learning, testing, refining, and consolidating knowledge until mastery is achieved.
Mastery of Core Clinical Concepts
A cornerstone of NBRC credentialing is mastery over core clinical concepts. Respiratory care, by its nature, demands precision, critical analysis, and the ability to synthesize vast amounts of information quickly. Professionals aspiring to certification must develop an intimate understanding of cardiopulmonary physiology, respiratory pharmacology, diagnostic methodologies, and patient-centered care principles. The depth of mastery extends beyond factual recall, requiring the ability to apply knowledge in dynamic, often unpredictable clinical scenarios.
Cardiopulmonary anatomy forms the foundation upon which other competencies are built. Understanding the intricate architecture of the lungs, heart, and vascular systems, as well as their interactions, allows practitioners to interpret clinical signs accurately and anticipate potential complications. Advanced pathophysiology complements this knowledge by highlighting mechanisms of disease, enabling therapists to identify subtle deviations from normal function. By weaving anatomical knowledge with pathophysiological insights, candidates cultivate a holistic vision of patient health that informs every therapeutic intervention.
Pharmacology represents another domain of critical significance. Respiratory therapists must grasp the pharmacokinetics, therapeutic effects, contraindications, and potential interactions of medications commonly used in pulmonary care. The ability to predict patient responses and adjust therapy based on individual needs is a hallmark of expertise. This level of understanding elevates practice from routine procedure execution to thoughtful, patient-specific care planning, which is precisely the competence NBRC examinations aim to evaluate.
Patient assessment and diagnostic proficiency are equally essential. Clinical reasoning involves integrating observational data, laboratory findings, and patient history to formulate effective interventions. Practicing systematic approaches to assessment, such as structured physical examinations and interpretation of diagnostic tests, ensures that candidates are well-prepared for both written and practical examination components. Mastery of these concepts is not achieved overnight; it emerges from continuous study, reflective practice, and iterative learning cycles that reinforce comprehension and application.
The Role of Simulation in Clinical Skill Enhancement
Simulation-based learning has emerged as a transformative tool in the preparation for NBRC credentialing. It bridges the gap between theoretical knowledge and real-world clinical application, offering a controlled environment in which candidates can hone skills, make mistakes safely, and refine decision-making processes. Simulation exercises, ranging from virtual patient encounters to hands-on ventilator management, cultivate procedural competence, confidence, and rapid problem-solving abilities.
The value of simulation lies in its capacity to replicate the pressures and unpredictability of actual clinical settings. Candidates confront scenarios that demand quick judgment, prioritization of interventions, and accurate documentation. By repeatedly navigating these simulated environments, learners develop not only technical expertise but also emotional resilience. The ability to remain composed and decisive under stress directly translates to improved performance in high-stakes NBRC examinations and daily clinical responsibilities.
Simulation also enhances critical thinking by encouraging reflective practice. After each exercise, candidates analyze decisions, identify errors, and evaluate alternative approaches. This reflective loop strengthens cognitive flexibility, allowing therapists to adapt strategies in response to evolving patient conditions. Furthermore, simulation facilitates inter-professional collaboration skills. Many exercises involve coordinated efforts with nurses, physicians, and other healthcare providers, mirroring the collaborative dynamics of actual patient care. Such experiential learning deepens understanding, reinforces clinical protocols, and embeds professional confidence.
Cognitive Strategies for Exam Success
Examination success extends beyond knowledge mastery; it requires sophisticated cognitive strategies designed to optimize recall, comprehension, and problem-solving under timed conditions. Cognitive strategies encompass memory techniques, pattern recognition, analytical reasoning, and stress modulation—each of which significantly impacts performance outcomes. Candidates who integrate these strategies systematically tend to outperform peers who rely solely on rote memorization.
Active recall and spaced repetition are foundational memory techniques. By periodically retrieving information from memory rather than passively reviewing notes, learners strengthen neural connections and improve long-term retention. Spaced repetition, which involves revisiting material at increasing intervals, enhances retention efficiency and ensures readiness even for complex, layered concepts such as mechanical ventilation modes or arterial blood gas interpretation. These techniques transform learning into an active, dynamic process rather than a passive accumulation of information.
Pattern recognition plays a crucial role in clinical problem-solving. Many NBRC examination questions present clinical scenarios requiring the identification of subtle cues, interpretation of diagnostic data, and prediction of patient outcomes. By practicing recognition of common patterns and anomalies, candidates accelerate decision-making while reducing cognitive load. Analytical reasoning further complements this skill, as candidates synthesize disparate pieces of information to formulate coherent solutions. Cognitive strategies, therefore, integrate memory, observation, and reasoning into a seamless problem-solving workflow.
Stress management is equally critical. High-pressure testing environments can trigger anxiety that interferes with cognitive function. Techniques such as controlled breathing, mindfulness, and pre-exam mental rehearsal enhance focus, stabilize physiological responses, and maintain clarity of thought. Candidates who proactively cultivate resilience find that examinations become opportunities to demonstrate competence rather than trials of endurance. Cognitive strategies, when combined with rigorous preparation, transform the examination process into a platform for showcasing mastery and confidence.
Integrating Continuous Professional Development
Credentialing does not mark an endpoint; it signifies a commitment to ongoing professional growth. Continuous professional development (CPD) is integral to maintaining competence, staying abreast of evolving clinical standards, and cultivating advanced expertise. Respiratory care is a dynamic field, influenced by technological innovations, emerging research, and shifting patient care paradigms. Engaging in CPD ensures that practitioners remain proficient, adaptable, and capable of delivering high-quality care throughout their careers.
CPD encompasses a variety of activities, including attending workshops, participating in case discussions, and engaging in peer-reviewed research. Each activity enriches knowledge, hones skills, and fosters reflective practice. For credentialed professionals, CPD also reinforces the principles assessed by NBRC examinations, creating a feedback loop that continuously sharpens both theoretical understanding and practical competence. Beyond technical skill, CPD nurtures critical attributes such as ethical judgment, cultural sensitivity, and patient-centered communication, all of which enhance professional identity.
The integration of CPD into daily practice cultivates a mindset of lifelong learning. Credentialed practitioners who embrace continuous growth are better equipped to anticipate challenges, innovate solutions, and contribute meaningfully to healthcare teams. Moreover, CPD facilitates specialization, enabling professionals to pursue advanced roles in pulmonary function testing, critical care, or respiratory education. The synergy between credentialing and ongoing development ensures that practitioners not only meet current standards but also shape the future of respiratory care with skill, insight, and integrity.
Navigating Professional Challenges in Respiratory Care
Respiratory therapists face a spectrum of professional challenges that extend beyond clinical expertise. High patient volumes, complex disease presentations, evolving technology, and regulatory expectations all demand adaptability, resilience, and problem-solving acumen. Credentialed professionals navigate these challenges by leveraging knowledge, experience, and interpersonal skills to deliver consistent, high-quality care under demanding conditions.
Ethical dilemmas and decision-making complexity are inherent to respiratory care. Therapists frequently encounter situations requiring careful balancing of patient autonomy, safety, and resource allocation. The ability to apply ethical frameworks, communicate effectively, and collaborate with interdisciplinary teams is vital. Credentialed professionals cultivate these capabilities during preparation for NBRC examinations, ensuring that clinical judgment is informed, compassionate, and evidence-based.
Workplace dynamics also present challenges. Communication gaps, varying team expectations, and time-sensitive demands can create stress and hinder performance. Effective strategies include proactive communication, reflective practice, and leadership development. Credentialed therapists who embrace these strategies foster positive team environments, enhance patient outcomes, and model professionalism for peers. The challenges of respiratory care, when met with preparation and insight, transform into opportunities for growth, skill refinement, and leadership within the healthcare ecosystem.
Understanding the Core of Respiratory Care
Respiratory care is a discipline that transcends simple clinical knowledge. It demands a sophisticated understanding of the respiratory system's intricate physiology and the subtle interplay between oxygen delivery, gas exchange, and patient responses. Practitioners navigate complex clinical scenarios that require a blend of empirical knowledge and intuitive judgment. Each patient presents a unique constellation of variables, from age and comorbidities to environmental influences, making adaptability a cornerstone of effective practice.
The mastery of respiratory mechanics forms the foundation of competent care. Recognizing the nuances of ventilation, perfusion, and diffusion allows clinicians to anticipate potential complications before they manifest. Beyond mechanical ventilation, clinicians engage with a spectrum of therapies that include oxygen supplementation, aerosolized medications, and noninvasive support. Integrating these modalities requires not only technical skill but also a keen sensitivity to patient comfort, physiological tolerance, and evolving clinical status.
Respiratory care also intersects with broader systemic considerations. Pulmonary function does not operate in isolation; cardiovascular health, neurological status, and metabolic balance exert continuous influence. Awareness of these interdependencies equips practitioners to craft interventions that are precise and contextually appropriate. High-caliber professionals cultivate a diagnostic lens that perceives subtle shifts in patient status, translating observation into timely intervention.
Building a Robust Knowledge Framework
Constructing a strong foundation for NBRC examinations begins with a deliberate accumulation of knowledge. This framework extends beyond memorization, encompassing the conceptual architecture that links pathophysiology, therapeutic intervention, and patient outcomes. Effective learners prioritize comprehension over rote learning, seeking to understand why a particular intervention produces a physiological effect rather than merely recalling the sequence of steps.
Integrating clinical scenarios into study routines amplifies retention. Case-based learning transforms abstract concepts into tangible experiences, fostering the ability to apply theory under time constraints. Simulated patient interactions, whether through role play or high-fidelity manikins, reinforce procedural memory and cultivate a practical mindset. This experiential learning sharpens diagnostic reasoning, ensuring that candidates can navigate complex questions on the NBRC examination with confidence and precision.
Resource selection plays a pivotal role in shaping the knowledge base. While textbooks provide structure, supplementing study with peer-reviewed articles, clinical guidelines, and evidence-based protocols ensures that knowledge remains current. The dynamic nature of respiratory care necessitates continuous intellectual engagement, encouraging learners to evolve alongside advances in therapeutic techniques and technological innovations.
Mastering Practical Skills Through Iteration
Excellence in respiratory care is inseparable from practical proficiency. Mastery of procedures such as endotracheal intubation, arterial blood gas interpretation, and ventilator management demands repetitive practice under guided supervision. Iteration transforms competence into fluid expertise, reducing the likelihood of error during high-pressure scenarios.
Structured practice regimens accelerate skill acquisition. Allocating focused time to each procedure, dissecting the steps into smaller components, and systematically correcting errors cultivates both accuracy and confidence. Observation and feedback from experienced mentors amplify the learning process, providing nuanced insights that textbooks cannot convey.
Integration of technology enhances practical preparedness. Advanced simulation tools replicate physiological responses, offering immediate feedback on clinical decisions. Trainees can observe the consequences of ventilator adjustments, medication titration, and airway interventions in real-time, reinforcing theoretical understanding with experiential evidence. Over time, repeated exposure to diverse scenarios fosters adaptability, ensuring practitioners remain composed and effective even in unfamiliar situations.
Strategic Time Management for Peak Performance
Time management is a critical determinant of success in both preparation and professional practice. The dual demands of occupational responsibilities and rigorous study schedules necessitate a disciplined approach that balances intensity with sustainability. Effective candidates craft study timetables that harmonize concentration periods with restorative intervals, preventing cognitive fatigue and sustaining engagement over long preparation cycles.
Prioritization is equally essential. Identifying high-yield topics, allocating time for weaker areas, and adhering to incremental goals ensures consistent progress. Micro-learning sessions, brief yet focused study blocks, promote retention by capitalizing on periods of heightened attention. Combining these with spaced repetition techniques embeds critical concepts into long-term memory, reducing the risk of knowledge decay as examination day approaches.
Equally important is the integration of reflective practices. Post-study review sessions, where learners critically assess comprehension and procedural accuracy, strengthen metacognition. This awareness enables learners to recognize patterns of misunderstanding and implement corrective strategies efficiently. Over time, deliberate planning and consistent evaluation cultivate an organized, resilient approach to both study and clinical practice.
Cultivating Analytical Reasoning
The NBRC examinations evaluate more than knowledge recall; they probe analytical reasoning, critical thinking, and clinical judgment. Success requires the ability to deconstruct complex scenarios, identify key variables, and synthesize information into actionable conclusions. Analytical proficiency emerges from practice, reflection, and deliberate engagement with challenging material.
Scenario-based study is a powerful method to enhance reasoning. By confronting varied clinical cases, learners develop the skill to discern relevant from irrelevant data, recognize subtle patterns, and anticipate potential complications. This process nurtures adaptive thinking, enabling candidates to navigate novel situations with confidence. It also fosters intellectual flexibility, a trait essential for high-level clinical decision-making where standard protocols may require contextual adaptation.
Pattern recognition is another essential aspect. Repeated exposure to clinical presentations and question types builds an intuitive understanding of common pitfalls and logical pathways. Over time, this experience allows candidates to approach complex problems methodically, reduce errors, and respond to unexpected challenges with agility and composure.
Strengthening Psychological Resilience
Psychological resilience underpins consistent performance, both in preparation and examination environments. Stress, anxiety, and performance pressure can erode focus and impair judgment, making mental conditioning an indispensable component of success. Mindfulness exercises, cognitive restructuring, and stress modulation techniques enhance emotional regulation, allowing candidates to remain centered under pressure.
Peer engagement and mentorship amplify resilience. Collaborative study environments provide motivation, perspective, and accountability. Discussing challenging cases, sharing strategies, and receiving constructive feedback fosters a supportive atmosphere that mitigates feelings of isolation and builds confidence. Mentorship, in particular, offers experiential guidance, helping learners navigate both procedural complexities and the psychological demands of rigorous preparation.
Visualization and mental rehearsal are potent tools for cultivating composure. Imagining procedural steps, anticipated questions, and potential complications primes the mind for real-world scenarios, reducing the likelihood of hesitation or error. Over time, these practices strengthen the neural pathways that govern decision-making, creating a cognitive framework that is both responsive and resilient.
Integrating Holistic Preparation Strategies
Effective preparation is holistic, encompassing cognitive mastery, procedural competence, and emotional resilience. Each element reinforces the others, creating a synergistic framework that enhances both learning and performance. Candidates who cultivate this integrated approach navigate the complexities of the NBRC examinations with strategic confidence and professional poise.
Holistic preparation includes deliberate reflection on progress. Self-assessment tools, practice exams, and procedural audits illuminate areas requiring reinforcement, while also reinforcing strengths. This cyclical process of evaluation, adjustment, and reapplication accelerates skill acquisition and knowledge consolidation.
Equally important is the harmonization of physical and mental well-being. Adequate rest, nutrition, and regular physical activity support cognitive function, endurance, and stress management. These factors are often underestimated, yet they play a decisive role in maintaining peak performance during intensive preparation and on examination day.
Through the integration of structured knowledge acquisition, iterative skill development, strategic time management, analytical reasoning, psychological resilience, and holistic self-care, candidates cultivate a robust, adaptive framework for success. This multifaceted preparation equips practitioners not only to excel in examinations but also to navigate the evolving landscape of respiratory care with competence and confidence.
Understanding the Core Competencies
Mastering the essential competencies required for professional credentialing is not merely a formality; it is the bedrock of long-term career success. These core skills encompass both technical proficiency and interpersonal acuity. For many aspiring practitioners, clinical knowledge forms the initial foundation. However, expertise in patient management, ethical practice, and effective communication is equally crucial. Developing these abilities demands deliberate practice, reflection, and consistent evaluation.
Clinical proficiency extends beyond rote memorization of protocols. It involves a nuanced understanding of human physiology, the capacity to interpret diagnostic data, and the agility to respond to unforeseen complications. Candidates who immerse themselves in real-world scenarios often find that textbook knowledge is amplified by practical exposure. Observation, guided practice, and reflective analysis cultivate a depth of skill that purely theoretical study cannot replicate.
Interpersonal competencies, though less tangible, significantly influence professional efficacy. Empathy, clear articulation, and collaboration with colleagues ensure that clinical interventions are implemented with precision and sensitivity. Practitioners who cultivate these qualities often experience smoother patient interactions, stronger professional relationships, and a more resilient approach to workplace challenges. In this sense, the mastery of core competencies represents an intersection of science, humanity, and strategic execution.
Strategic Preparation for Examination Success
The pathway to credentialing is invariably punctuated by rigorous examinations designed to assess both knowledge and application. Effective preparation transcends mere memorization; it requires strategic engagement with material, self-assessment, and iterative refinement. Structured study schedules, coupled with active recall techniques, strengthen retention and facilitate mastery of complex concepts.
Simulation exercises serve as a potent tool in reinforcing learning. By recreating real-life clinical scenarios, candidates are able to practice decision-making under pressure, refine procedural skills, and evaluate outcomes. This form of deliberate practice bridges the gap between theory and practice, ensuring that knowledge is not only internalized but readily deployable in professional contexts.
Time management also plays a pivotal role in exam preparation. Breaking study material into manageable segments, prioritizing high-yield content, and balancing rest periods reduces cognitive overload. Candidates who maintain disciplined routines often report increased confidence, reduced anxiety, and enhanced performance. Equally important is cultivating a mindset that embraces challenges as opportunities for growth rather than sources of stress, fostering resilience that extends beyond the examination room.
Mastery of Documentation and Record-Keeping
In clinical and credentialing contexts, meticulous record-keeping is far more than administrative compliance; it is a reflection of professional integrity. Detailed documentation provides a verifiable trail of clinical experience, supports continuity of care, and ensures adherence to ethical standards. Developing systematic methods for recording patient interactions, procedural steps, and reflective notes enhances both accountability and learning.
Digital platforms now enable sophisticated tracking of professional activities. Candidates can log encounters, track skill development, and generate performance analytics with precision. These tools not only facilitate credentialing verification but also provide valuable feedback for self-assessment. Proper documentation cultivates habits of organization, critical thinking, and reflective practice, which are indispensable across the healthcare continuum.
Maintaining accuracy and completeness requires ongoing vigilance. Minor omissions or inconsistencies in records can compromise credibility or delay credentialing outcomes. Establishing routine audits, seeking mentor feedback, and cross-referencing documentation with formal requirements minimize the risk of errors. Over time, meticulous record-keeping evolves from a procedural necessity into an ingrained professional ethic.
Integrating Practical Experience with Theoretical Knowledge
The symbiotic relationship between practical exposure and theoretical understanding is central to professional development. Knowledge alone, no matter how extensive, remains incomplete without the lens of real-world application. Conversely, clinical experience without foundational understanding can lead to inconsistent practice or gaps in reasoning. Integrating these domains ensures competence, confidence, and adaptability.
Clinical rotations, internships, and supervised practice provide invaluable opportunities for experiential learning. Engaging actively in patient care, observing diverse methodologies, and participating in multidisciplinary teams cultivate both technical skill and professional judgment. Reflection upon these experiences enables practitioners to internalize lessons, identify areas for improvement, and apply abstract principles to tangible challenges.
Equally critical is the iterative cycle of assessment and feedback. Constructive critique from mentors, peers, and supervisors illuminates blind spots, validates progress, and motivates refinement. This ongoing dialogue transforms experience into expertise, fostering a deep comprehension of both the science and art of patient care. By consciously bridging theory and practice, professionals achieve a level of mastery that prepares them for increasingly complex responsibilities.
Navigating Professional Ethics and Responsibility
Ethical conduct forms the backbone of trustworthy practice. Credentialing boards emphasize adherence to professional codes, emphasizing the moral, legal, and social dimensions of healthcare. Ethical dilemmas often require nuanced judgment, balancing patient welfare, institutional policies, and societal norms. Developing a robust ethical framework ensures that decisions remain consistent, defensible, and patient-centered.
Responsibility extends beyond individual actions to encompass accountability within teams and organizations. Practitioners must exercise vigilance in reporting errors, respecting confidentiality, and advocating for equitable care. Cultivating ethical resilience involves reflective practice, continuous education, and an unwavering commitment to core values. Candidates who internalize these principles not only meet credentialing standards but also cultivate professional credibility and enduring trust within the communities they serve.
Ethics also intersect with documentation, decision-making, and communication. Transparent reporting, informed consent, and respectful interaction with patients and colleagues reinforce ethical integrity. Over time, these practices evolve from regulatory compliance into a professional identity defined by conscientiousness, empathy, and moral clarity.
Optimizing Time and Resource Management
The journey toward credentialing demands the integration of multiple concurrent responsibilities: study, clinical practice, documentation, and personal obligations. Efficient time and resource management becomes a critical skill for sustaining progress without burnout. Establishing structured routines, prioritizing high-impact activities, and leveraging supportive resources reduces stress and maximizes outcomes.
Strategic allocation of resources encompasses both tangible and intangible assets. Study aids, mentorship opportunities, and digital tools enhance efficiency and provide targeted support. Equally important is the judicious management of energy and attention, ensuring that focus is sustained during high-intensity periods while allowing for restorative intervals. Practitioners who achieve this equilibrium report enhanced performance, greater retention, and sustained professional growth.
Long-term planning also mitigates the impact of unforeseen disruptions. Contingency strategies, flexible scheduling, and proactive engagement with credentialing authorities ensure that setbacks do not derail progress. By cultivating foresight and organizational discipline, candidates navigate the multifaceted demands of credentialing with confidence and resilience.
Cultivating Lifelong Learning and Professional Growth
Credentialing represents a milestone, not an endpoint, in professional development. The rapidly evolving landscape of healthcare demands continuous learning, skill refinement, and adaptability. Practitioners who embrace lifelong learning remain at the forefront of practice, ensuring that knowledge and competencies evolve in tandem with emerging research, technologies, and patient needs.
Engagement with professional communities, attendance at workshops, and participation in specialized training programs foster both knowledge expansion and collegial networking. Exposure to diverse perspectives enhances critical thinking, stimulates innovation, and encourages reflective practice. By embedding continuous learning into daily routines, professionals transform credentialing into a launchpad for ongoing growth rather than a singular achievement.
Equally vital is cultivating intellectual curiosity and self-directed inquiry. Asking probing questions, seeking evidence-based solutions, and exploring interdisciplinary approaches promote depth of understanding and versatility in practice. Lifelong learning thus becomes both a personal commitment and a professional imperative, ensuring sustained competence, relevance, and fulfillment throughout a career in healthcare.
Navigating the Pathway to NBRC Credentialing
The journey toward NBRC credentialing requires more than simply studying for exams. It demands a holistic approach encompassing strategic planning, intellectual adaptability, and emotional endurance. Many aspirants underestimate the intricacies involved, assuming that diligence alone suffices. In reality, credentialing is a multifaceted process that intertwines rigorous knowledge acquisition, procedural accuracy, and personal discipline. Understanding the landscape in its entirety allows candidates to approach preparation with a framework that integrates both content mastery and practical execution.
Developing a systematic plan begins with an honest assessment of current competencies and potential gaps. Candidates must evaluate prior academic exposure, clinical experience, and familiarity with examination formats. This self-awareness informs the creation of a personalized roadmap, where time allocation aligns with areas demanding greater attention. Regularly revisiting and adjusting this plan ensures that preparation remains dynamic rather than stagnant, fostering steady progress even amid competing responsibilities.
Time management emerges as a pivotal factor. Balancing professional duties, personal life, and study schedules often stretches candidates to their limits. Embedding learning into existing routines can transform constraints into opportunities. Short, focused study intervals, frequent review sessions, and the integration of applied clinical scenarios cultivate retention without imposing excessive strain. This approach emphasizes efficiency over volume, reinforcing the principle that strategic engagement with material outweighs sheer quantity of hours invested.
Cultivating Intellectual Mastery
The NBRC examinations challenge candidates to synthesize knowledge across diverse domains. Respiratory care is not a field of compartmentalized information; rather, it demands an integrated understanding of pathophysiology, therapeutic interventions, diagnostic reasoning, and procedural protocols. Candidates who focus on isolated memorization often find themselves disoriented when faced with complex, scenario-based questions.
A more fruitful approach emphasizes contextual learning. For example, understanding the physiological rationale behind mechanical ventilation choices equips candidates to navigate nuanced patient scenarios with confidence. Concept mapping and structured visual aids transform abstract principles into accessible frameworks, enhancing both comprehension and recall. Collaborative study, where peers engage in simulated clinical discussions, further reinforces mastery by exposing candidates to perspectives they might not independently consider.
Reinforcement through repetition remains essential, but the methodology matters. Passive reading or rote memorization yields limited retention under examination pressure. Active engagement—summarizing, teaching concepts to others, or applying knowledge to clinical simulations—consolidates learning and builds confidence. Intellectual mastery is less about the volume of content covered and more about the depth of understanding achieved, allowing candidates to respond flexibly to unfamiliar challenges.
Overcoming Common Credentialing Hurdles
The journey toward NBRC credentialing is seldom linear. Candidates encounter diverse obstacles ranging from content difficulty to procedural complexities. One prevalent challenge is balancing professional obligations with rigorous study demands. Many candidates juggle clinical shifts, family responsibilities, and ongoing education, creating a dynamic where time feels scarce and stress is magnified. Adopting flexible study techniques and integrating learning into daily routines can alleviate these pressures. Micro-learning during breaks, applying concepts in real patient scenarios, and collaborative study sessions offer practical solutions.
Another hurdle involves mastering the breadth of content covered in examinations. Respiratory care encompasses extensive knowledge domains, from mechanical ventilation strategies to pharmacologic interventions and diagnostic testing. Candidates often struggle with retaining nuanced details and applying them accurately under time constraints. Contextual learning, concept mapping, and scenario-based exercises enhance comprehension and facilitate recall. Recognizing that understanding principles is more valuable than rote memorization enables candidates to navigate complex questions with greater ease.
Procedural and administrative challenges also surface frequently. Missteps in application submission, misreading eligibility requirements, or misunderstanding examination protocols can create avoidable setbacks. Engaging with NBRC resources, attending preparatory workshops, and connecting with peers who have successfully navigated the process reduces uncertainty and fosters confidence.
Psychological barriers should not be underestimated. Fear of failure, perfectionism, and self-doubt often impede progress more than knowledge gaps. Developing resilience through mindfulness, reflective practice, and stress management equips candidates to confront these mental challenges. Learning to approach obstacles as opportunities for growth transforms frustration into motivation, creating a mindset conducive to sustained effort and eventual success.
Overcoming credentialing hurdles is ultimately about adaptability, foresight, and perseverance. Candidates who anticipate challenges, employ strategic approaches, and cultivate emotional resilience position themselves not merely to succeed but to thrive in the credentialing process.
Enhancing Clinical Reasoning Skills
A critical component of NBRC preparation involves the refinement of clinical reasoning. Knowledge alone does not translate into effective decision-making at the bedside. Candidates must learn to interpret patient data, weigh therapeutic options, and anticipate potential complications. This analytical capacity emerges through consistent exposure to real or simulated clinical scenarios, where candidates actively reason through diverse challenges.
Case-based learning strengthens this ability by bridging theory with practice. Examining patient histories, laboratory results, and ventilatory parameters allows candidates to apply foundational concepts in authentic contexts. This process not only improves knowledge retention but also develops judgment under pressure, a skill highly relevant both during examinations and in professional practice.
Reflective practice further amplifies reasoning abilities. Evaluating past clinical encounters, considering alternative approaches, and identifying areas for improvement nurtures a habit of continual learning. Candidates who cultivate self-awareness in their decision-making process often demonstrate superior adaptability, responding with agility to unforeseen complications or novel scenarios.
Time Management and Study Efficiency
Effective time management is indispensable for successful credentialing. Many candidates underestimate the demands of examination preparation, leading to last-minute cramming, heightened anxiety, and incomplete content coverage. Establishing a structured schedule that balances intensive review with rest periods prevents burnout while promoting consistent progress.
Micro-study techniques enhance efficiency by transforming otherwise idle moments into productive learning experiences. Short, concentrated intervals of review—whether during commutes, breaks, or quiet periods—reinforce retention without overwhelming the candidate. Strategic prioritization, focusing first on weaker content areas, ensures that study efforts yield maximum benefit. Over time, this disciplined approach fosters both knowledge mastery and confidence, reducing the sense of being overwhelmed.
Consistency proves more valuable than intensity. Regular engagement with material, even in small increments, solidifies understanding and creates a sense of forward momentum. Candidates who adhere to a reliable schedule find that cumulative effort surpasses sporadic bursts of exhaustive study, reflecting the principle that slow, steady preparation outpaces hurried cramming.
Building Emotional Resilience
The psychological dimension of credentialing is often underestimated. Anxiety, self-doubt, and fear of failure can significantly hinder performance. Candidates who neglect emotional preparedness may encounter obstacles even when fully competent in content knowledge. Developing resilience is thus as critical as intellectual preparation.
Mindfulness and stress management techniques foster a sense of calm, allowing candidates to approach study sessions and examinations with clarity. Visualization strategies, positive self-talk, and structured reflection reinforce confidence, helping candidates maintain focus under pressure. Additionally, maintaining a support network of peers, mentors, or family members provides encouragement and perspective, preventing isolation and emotional fatigue.
Resilience also involves embracing setbacks as opportunities for growth rather than indicators of inadequacy. Mistakes, misunderstandings, or incomplete practice tests should be viewed as diagnostic tools rather than failures. By reframing challenges as learning experiences, candidates cultivate a mindset that supports continuous improvement, perseverance, and sustained motivation.
Leveraging Peer Networks and Resources
A robust support network can dramatically enhance credentialing outcomes. Engaging with peers who share similar goals facilitates the exchange of knowledge, study strategies, and moral support. Collaborative learning environments enable discussion of complex topics, clarification of doubts, and exposure to diverse problem-solving approaches.
Resource utilization extends beyond peer engagement. Accessing up-to-date reference materials, participating in workshops, and employing practice examinations provides candidates with both content reinforcement and familiarity with test formats. These resources, when used strategically, reduce uncertainty and allow candidates to approach examinations with greater confidence. A proactive approach to resource engagement transforms preparation from a solitary endeavor into a dynamic, interactive process.
Networking also nurtures accountability. Regular check-ins with peers or mentors encourage consistent effort, provide constructive feedback, and create an environment in which goals remain visible and achievable. This interconnected approach promotes both intellectual growth and emotional stability, essential components of a successful credentialing journey.
The Significance of Lifelong Learning in Respiratory Care
Respiratory care is a profession that evolves with remarkable pace. The acquisition of credentials represents not merely an endpoint but the commencement of a journey toward continuous refinement. Professionals who attain certification are entrusted with the responsibility of sustaining and enhancing their expertise. Lifelong learning is therefore not an optional endeavor; it is an essential component of professional identity. Engaging consistently with new knowledge allows practitioners to adapt seamlessly to emerging therapies, cutting-edge technologies, and evolving clinical guidelines. The practice of respiratory care demands a flexible mind and a commitment to perpetual intellectual growth, ensuring that practitioners remain adept at navigating complex patient scenarios.
The process of lifelong learning transcends mere knowledge acquisition. It encompasses critical thinking, reflective evaluation, and the application of novel information in real-world clinical settings. Practitioners who cultivate these abilities demonstrate resilience in the face of changing clinical landscapes. Furthermore, ongoing education fosters adaptability, allowing respiratory care specialists to anticipate shifts in patient needs and healthcare standards. This proactive approach ensures that care delivery is informed by both historical insight and contemporary innovation. Continuous engagement with professional literature, workshops, and seminars solidifies competence and promotes a culture of excellence within the healthcare environment.
Maintaining expertise through lifelong learning is also intrinsically linked to patient outcomes. Research indicates that healthcare providers who regularly update their knowledge and skills are better equipped to implement evidence-based interventions. The assimilation of new methodologies enhances diagnostic accuracy, therapeutic precision, and overall patient safety. Consequently, the commitment to lifelong learning represents not only a professional obligation but a moral imperative, reflecting the ethical responsibility of practitioners to deliver optimal care. Respiratory care professionals who embrace this ethos cultivate a robust foundation upon which both their individual growth and the advancement of the field rest.
Reflective Practice as a Tool for Professional Growth
After credential attainment, the practice of reflection becomes a cornerstone for sustained proficiency. Reflective practice is a deliberate process through which practitioners analyze their actions, decisions, and outcomes to derive meaningful insights. By identifying areas of strength and recognizing aspects requiring improvement, respiratory care specialists can tailor their professional development strategies with precision. Reflection transcends mere self-evaluation; it is a mechanism for cultivating deeper understanding, sharpening clinical judgment, and fostering intellectual agility.
Structured reflection allows professionals to dissect their clinical experiences systematically. This process encourages the identification of recurring challenges, assessment of decision-making processes, and consideration of alternative approaches. Such analytical scrutiny strengthens critical reasoning, enabling practitioners to navigate complex cases with enhanced confidence. Moreover, reflective practice nurtures emotional intelligence, as professionals become more attuned to the nuances of patient interactions, interdisciplinary collaboration, and personal responses to clinical stressors. This comprehensive awareness amplifies both technical competence and empathetic care delivery.
Incorporating reflection into routine practice also encourages a culture of continuous improvement. Even those who demonstrate exemplary performance benefit from scrutinizing their methods and outcomes. By embracing reflective habits, respiratory care specialists maintain an active dialogue with their own professional growth, ensuring that accomplishments are not static but are instead leveraged to achieve higher levels of mastery. Reflection, therefore, functions as both a mirror and a compass, providing insight into past experiences while guiding future endeavors toward ever-greater proficiency.
Strategic Engagement in Continuing Education
Continuing education represents a pivotal avenue for sustaining respiratory care credentials. Participation in accredited courses, workshops, and seminars enables professionals to remain conversant with advancements in technology, therapy modalities, and clinical protocols. These educational endeavors are not perfunctory obligations but rather dynamic opportunities to expand the repertoire of knowledge, refine practical skills, and cultivate innovative approaches to patient care. Professionals who embrace ongoing education demonstrate a proactive commitment to excellence and a readiness to adapt to shifting healthcare paradigms.
Effective continuing education requires deliberate planning and goal setting. Practitioners should identify areas that require reinforcement or exploration and seek opportunities aligned with these objectives. Integrating learning into daily practice fosters an experiential understanding, bridging theoretical knowledge with hands-on application. Moreover, exposure to interdisciplinary educational formats enhances holistic comprehension, as insights from related fields illuminate new strategies and solutions. The interplay between formal education and clinical experience forms the bedrock of sustainable expertise, ensuring that practitioners remain agile, informed, and competent.
The benefits of continuing education extend beyond technical proficiency. Engaging with diverse perspectives stimulates intellectual curiosity, encourages innovation, and strengthens problem-solving abilities. Professionals exposed to varied approaches and case studies develop versatility, improving their capacity to respond to unpredictable patient scenarios. Additionally, structured educational engagement reinforces professional credibility, signaling to peers, employers, and patients alike that the practitioner maintains an active commitment to competence and best practice standards. In essence, continuing education is both a shield against obsolescence and a catalyst for enduring professional growth.
Documentation and Compliance in Credential Maintenance
Credential maintenance is inextricably linked to meticulous record-keeping and adherence to regulatory mandates. Many credentials require systematic documentation of practice hours, completion of approved educational modules, and proof of ongoing professional engagement. Establishing disciplined documentation practices ensures uninterrupted credential validity and safeguards against lapses in compliance. The cultivation of organized, precise records reflects a conscientious approach to professional responsibility and reinforces trust in the practitioner’s expertise.
Implementing effective documentation strategies begins with the creation of structured systems for tracking activities. Digital platforms, spreadsheets, and dedicated professional logs can streamline the recording process, reducing the risk of oversight. Scheduling periodic reviews and updates of these records ensures that all requirements are met proactively, mitigating the stress of last-minute verification. Moreover, a consistent documentation routine reinforces accountability, encouraging practitioners to integrate professional development seamlessly into their daily practice rather than treating it as an ancillary task.
Compliance with credentialing standards is not solely an administrative exercise; it reflects a broader ethical commitment. Adherence to established protocols safeguards patient safety, upholds professional integrity, and fosters a culture of accountability. Respiratory care specialists who prioritize regulatory compliance demonstrate an understanding of the interplay between procedural diligence and clinical excellence. By maintaining meticulous documentation and anticipating credentialing obligations, practitioners secure both professional recognition and the confidence necessary to perform at the highest level of competency.
The Role of Professional Networking in Sustaining Expertise
Professional networking constitutes a powerful mechanism for maintaining respiratory care credentials and enhancing clinical acumen. Interacting with colleagues, mentors, and interdisciplinary teams facilitates the exchange of knowledge, exposure to innovative practices, and engagement with emerging trends. Networking extends beyond superficial socialization, serving as a dynamic platform for collaboration, consultation, and professional enrichment. It enables practitioners to remain connected to the broader community, fostering shared learning and reinforcing professional identity.
Participation in conferences, forums, and online professional communities provides a fertile ground for intellectual stimulation. Engaging with peers exposes practitioners to diverse perspectives, novel techniques, and case studies that may not arise within routine practice. Networking also supports problem-solving, as practitioners can seek guidance, discuss challenges, and explore alternative strategies in a collaborative environment. These interactions cultivate both competence and confidence, equipping respiratory care specialists with the resources and insights necessary to navigate complex clinical landscapes effectively.
Beyond knowledge acquisition, professional networking nurtures mentorship and leadership development. Experienced practitioners can guide emerging professionals, offering advice, feedback, and support. This mentorship dynamic fosters continuity of expertise within the field, ensuring that institutional knowledge and best practices are transmitted across generations. Simultaneously, networking empowers practitioners to assume leadership roles, contribute to policy development, and influence the trajectory of respiratory care. In this way, professional connections serve as both a lifeline for personal growth and a conduit for broader professional impact.
Innovative Approaches to Sustaining Clinical Competence
Sustaining clinical competence requires more than adherence to conventional strategies; it demands innovation and adaptability. Respiratory care specialists who experiment with novel techniques, integrate emerging technologies, and explore interdisciplinary approaches position themselves at the forefront of practice. Innovation in professional development encourages creative problem-solving, enhances efficiency, and fosters a forward-thinking mindset that transcends routine procedural adherence. By embracing innovative strategies, practitioners ensure that their expertise evolves in tandem with the field rather than stagnating.
Incorporating technology into ongoing professional growth offers significant advantages. Digital simulation, virtual training modules, and interactive learning platforms provide immersive experiences that enhance skill retention and clinical decision-making. The integration of technology into routine practice supports precision, reduces error rates, and facilitates continuous assessment. Moreover, technological tools allow for customized learning paths, enabling practitioners to address individual knowledge gaps and target specific competencies effectively. Innovation, therefore, becomes a vehicle for both personal enrichment and improved patient outcomes.
Interdisciplinary collaboration further enhances innovative professional development. Exposure to allied healthcare perspectives, research findings, and complementary therapeutic approaches broadens clinical understanding and inspires inventive solutions. Collaborative innovation fosters adaptive expertise, equipping practitioners to respond to complex scenarios with ingenuity and flexibility. This proactive embrace of innovation ensures that credentialed professionals maintain relevance, demonstrating both mastery of established protocols and readiness to lead advancements in respiratory care.
Sustaining Momentum Through Structured Professional Habits
The post-examination phase represents a critical juncture in professional evolution. Establishing structured habits and routines ensures that credentialed practitioners sustain momentum beyond initial achievement. Daily engagement with literature, periodic reflection, and consistent skill application cultivate a rhythm of professional activity that supports ongoing competence. Structured habits embed excellence into the fabric of practice, transforming professional growth from an abstract goal into a tangible, achievable reality.
Developing a personalized framework for continuous development enhances both efficiency and efficacy. Prioritizing tasks, scheduling educational sessions, and dedicating time for reflection ensure that professional obligations are met without undue strain. This structured approach also facilitates long-term planning, enabling practitioners to align immediate learning objectives with broader career aspirations. By maintaining disciplined routines, respiratory care specialists reinforce their commitment to excellence, demonstrating that credentials are living representations of capability rather than static acknowledgments of past success.
The integration of structured habits fosters resilience and adaptability. Practitioners who cultivate consistent routines develop the capacity to navigate unforeseen challenges, respond to evolving clinical demands, and sustain high standards under pressure. This resilience reinforces confidence, ensuring that professional identity remains robust and agile. Ultimately, the establishment of structured habits transforms credential maintenance into a dynamic, ongoing process, embedding professional excellence into daily practice and securing a trajectory of continuous advancement.
The Foundation of Respiratory Care Excellence
Respiratory care stands as a pivotal domain in modern healthcare, bridging the complex intersection of patient physiology, technology, and compassionate care. At the heart of this field lies the art of balancing precise clinical interventions with empathetic patient interaction. The early days of a respiratory professional’s journey are marked by immersion into rigorous academic and practical experiences, where foundational skills are honed and clinical judgment begins to flourish. The cultivation of sharp observational abilities, coupled with a profound understanding of pulmonary mechanics, establishes the essential groundwork for a career that thrives on both intellect and human connection.
Professional competence is shaped not only by technical knowledge but also by the ability to navigate dynamic healthcare environments. Respiratory practitioners often encounter scenarios demanding rapid assessment, adaptability, and decisive action. These challenges foster resilience and refine problem-solving capacities. The meticulous study of anatomy, physiology, and pharmacology becomes a canvas upon which practical expertise is painted, enabling professionals to anticipate complications, optimize interventions, and ensure patient safety with precision. The journey begins with a dedication to foundational mastery, yet it quickly evolves into a pursuit of nuanced understanding, where every clinical encounter contributes to the depth of professional wisdom.
Cultivating Lifelong Learning and Adaptability
The landscape of respiratory care is characterized by perpetual innovation and evolving clinical standards. As new therapeutic modalities, diagnostic tools, and treatment protocols emerge, the imperative for continuous learning intensifies. Professionals who embrace a mindset of curiosity and intellectual agility position themselves at the forefront of their field, capable of integrating cutting-edge advancements into daily practice. Lifelong learning transcends formal education; it encompasses the deliberate pursuit of knowledge through workshops, peer collaboration, and self-directed study, fostering an enduring commitment to excellence.
Adaptability complements this pursuit, enabling professionals to navigate unpredictable clinical environments with poise. Changes in patient demographics, healthcare policies, and technological infrastructures demand practitioners who can recalibrate strategies swiftly and effectively. The capacity to integrate novel approaches while maintaining evidence-based standards distinguishes exceptional practitioners from their peers. By valuing adaptability alongside knowledge acquisition, respiratory care professionals cultivate a professional resilience that not only enhances patient outcomes but also enriches their own career trajectory.
Advanced Clinical Skills and Specialized Competencies
The evolution from competent practitioner to expert clinician is marked by the acquisition of specialized skills and competencies. Advanced proficiency in mechanical ventilation, pulmonary diagnostics, and critical care interventions positions professionals to address complex patient needs with precision and confidence. Beyond technical acumen, the ability to interpret intricate data, anticipate physiological responses, and implement nuanced treatment plans differentiates seasoned professionals from novices. Each intervention becomes an opportunity to apply both analytical rigor and compassionate insight, ensuring that care remains patient-centered while anchored in clinical excellence.
Specialization in niche areas offers a pathway for profound professional growth. Subfields such as neonatal respiratory therapy, pulmonary rehabilitation, or sleep medicine provide avenues for focused mastery. These specialized roles demand a higher level of expertise, yet they simultaneously afford practitioners the satisfaction of delivering deeply impactful care. The pursuit of advanced certifications and fellowships enhances not only technical skills but also professional recognition, reinforcing a practitioner’s authority within the broader healthcare community. Specialization transforms routine practice into a platform for innovation, thought leadership, and meaningful patient outcomes.
Strategic Career Advancement and Leadership
Building a thriving career in respiratory care requires more than clinical skill—it necessitates strategic vision and proactive engagement with professional opportunities. Credentialing serves as an initial gateway, validating core competencies and facilitating entry into the field. Yet long-term success depends on leveraging credentials to access leadership roles, interdisciplinary collaboration, and decision-making responsibilities. Effective leaders in respiratory care balance operational insight with visionary thinking, guiding teams through complex challenges while shaping policies that influence patient care at systemic levels.
Mentorship is a critical component of leadership development. By guiding junior professionals, leading educational workshops, and contributing to training programs, experienced practitioners expand their influence while refining essential interpersonal skills. These experiences cultivate the ability to communicate complex concepts clearly, foster collaboration, and inspire confidence among colleagues. Leadership in this context is not solely about hierarchical authority but about the capacity to elevate collective performance, inspire professional growth, and advocate for evidence-based improvements within healthcare institutions.
Professional Engagement and Scholarly Contribution
Active engagement with the professional community amplifies both career development and the advancement of respiratory care as a discipline. Participation in conferences, research initiatives, and clinical trials enables practitioners to contribute to the evidence base, shape emerging standards, and engage with peers at the forefront of innovation. Such involvement fosters intellectual stimulation, enhances professional visibility, and strengthens networks that support collaborative problem-solving and idea exchange.
Research engagement, in particular, provides a conduit for thought leadership. By designing studies, analyzing outcomes, and disseminating findings, practitioners influence clinical practices, inform policy decisions, and inspire the next generation of healthcare professionals. Scholarly contribution extends the impact of individual expertise beyond immediate patient interactions, positioning the professional as a vital agent in the evolution of respiratory care. The integration of research, clinical practice, and professional networking transforms individual achievement into a collective advancement that elevates the field as a whole.
Cultivating Personal Resilience and Professional Fulfillment
The demands of respiratory care can be intense, encompassing high-stakes clinical decisions, emotionally charged patient interactions, and continuous adaptation to technological and procedural developments. Cultivating personal resilience is essential for sustaining performance, maintaining mental well-being, and achieving long-term professional fulfillment. Strategies such as reflective practice, mindfulness, and structured peer support provide mechanisms to navigate stress, prevent burnout, and reinforce the intrinsic motivation that draws many into the field.
Professional fulfillment arises from a combination of mastery, impact, and personal growth. When respiratory care practitioners align their technical skills with patient-centered values, pursue ongoing education, and engage in leadership or specialized roles, they experience a sense of purpose that transcends routine duties. This alignment of capability and meaning cultivates a career that is not only sustainable but also profoundly rewarding. Each milestone, whether it be the successful management of a complex case or the completion of an advanced certification, contributes to an enduring sense of accomplishment and professional satisfaction.
Transforming Credentials into Lasting Influence
Credentials, while essential, represent merely the foundation upon which a distinguished career is built. The true measure of professional excellence lies in the capacity to translate recognized qualifications into tangible impact, both within clinical settings and across the broader healthcare landscape. By embracing continuous learning, seeking specialization, participating in research, and engaging in leadership, respiratory care professionals transform credentials into instruments of influence. These efforts enable the shaping of healthcare practices, the mentoring of future practitioners, and the delivery of care that is both scientifically robust and deeply humane.
The journey from initial certification to sustained professional mastery is dynamic and multifaceted. It demands intellectual curiosity, strategic foresight, and an unwavering commitment to patient well-being. Professionals who navigate this path with diligence and vision discover a landscape rich with opportunities, from pioneering interventions to shaping the evolution of the discipline itself. The process is continuous, rewarding, and imbued with significance, reflecting the unique blend of technical skill, compassion, and innovation that defines the essence of respiratory care.
Conclusion
Navigating NBRC credentialing is a multifaceted journey that blends knowledge, clinical skill, strategic planning, and emotional resilience. From understanding the credentialing landscape to preparing effectively, managing applications, overcoming hurdles, and maintaining credentials, each phase demands deliberate effort and thoughtful engagement. Success is not measured solely by passing examinations but by the transformation into a confident, competent, and reflective healthcare professional.
Beyond the immediate achievement, credentialing lays the foundation for a thriving career in respiratory care. It opens doors to specialization, leadership, mentorship, and meaningful contributions to patient outcomes. Embracing lifelong learning, staying current with evolving practices, and actively engaging in the professional community ensures that credentials remain a living testament to expertise rather than a static accomplishment.
Ultimately, the NBRC credentialing process is both a challenge and an opportunity. It tests knowledge, sharpens clinical reasoning, and strengthens character. Professionals who approach it with preparation, persistence, and foresight emerge not only credentialed but empowered, ready to elevate standards of care, inspire peers, and leave a lasting impact on the field of respiratory therapy.
Frequently Asked Questions
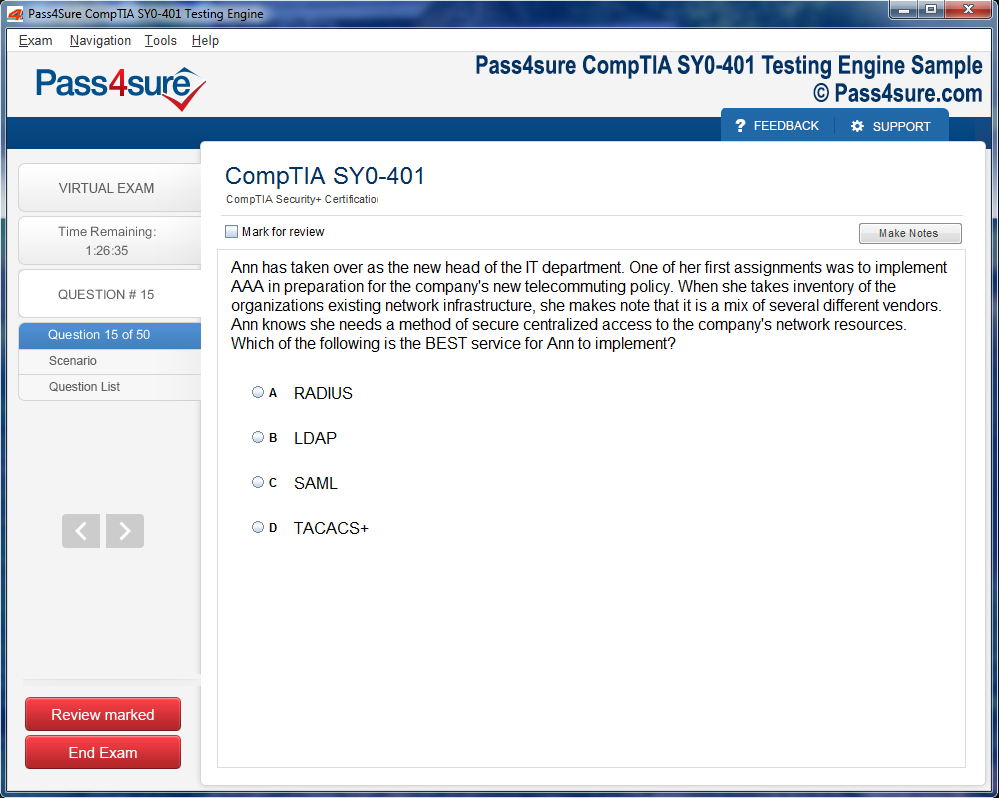
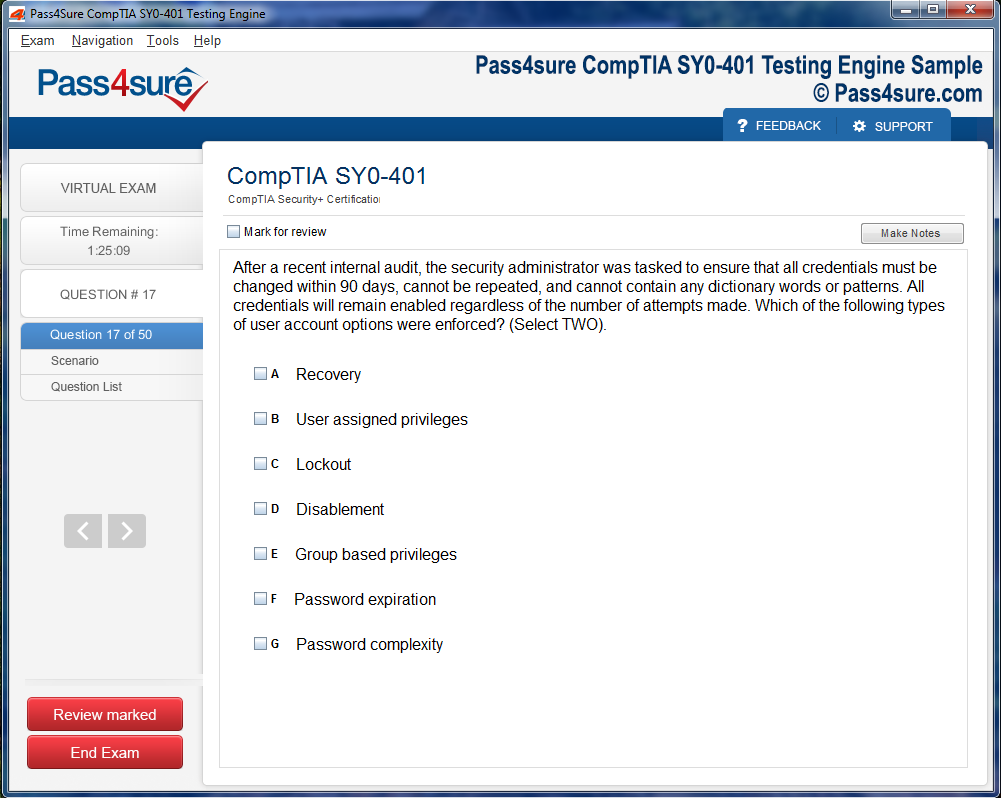
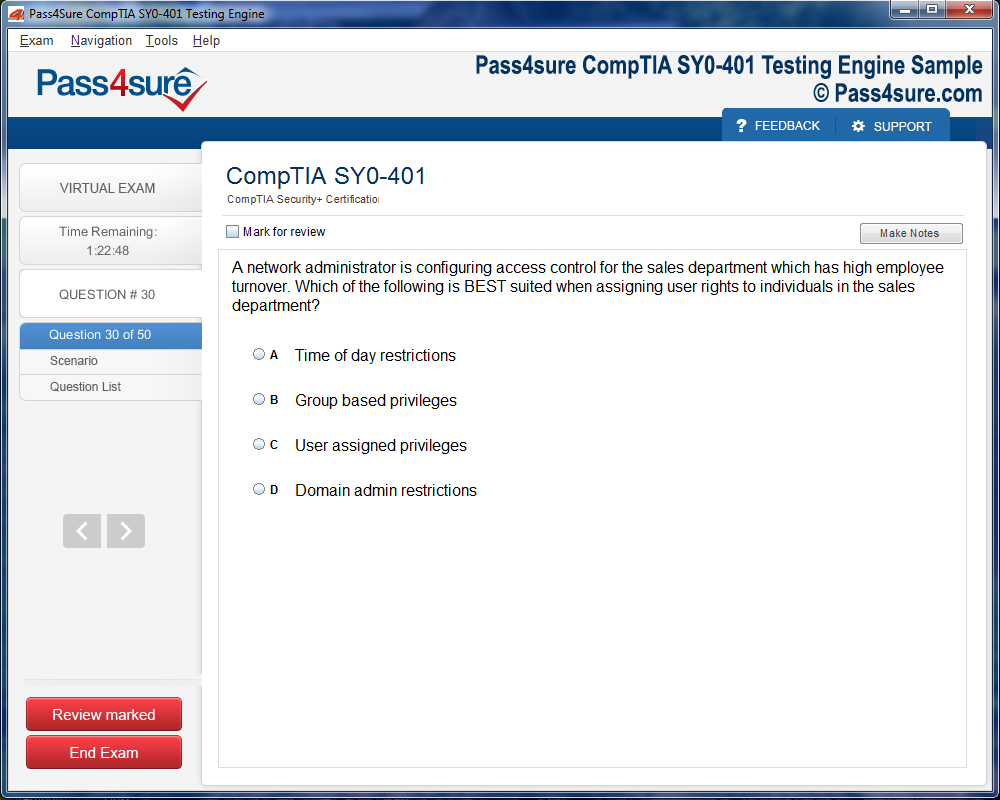
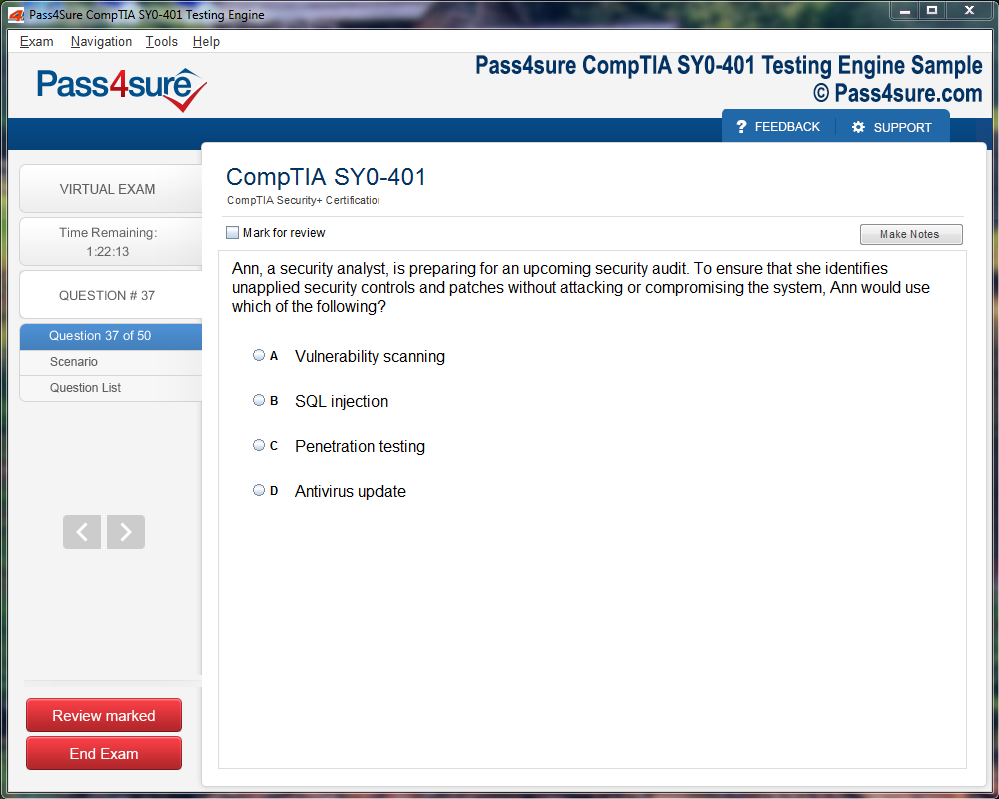
How does your testing engine works?
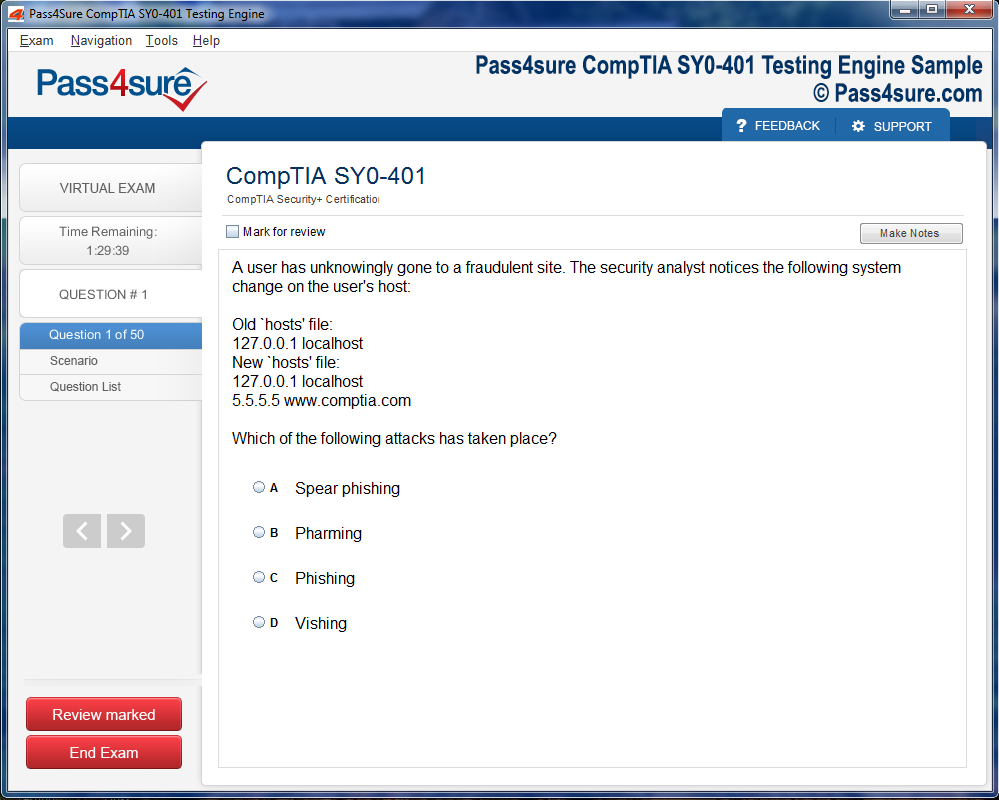
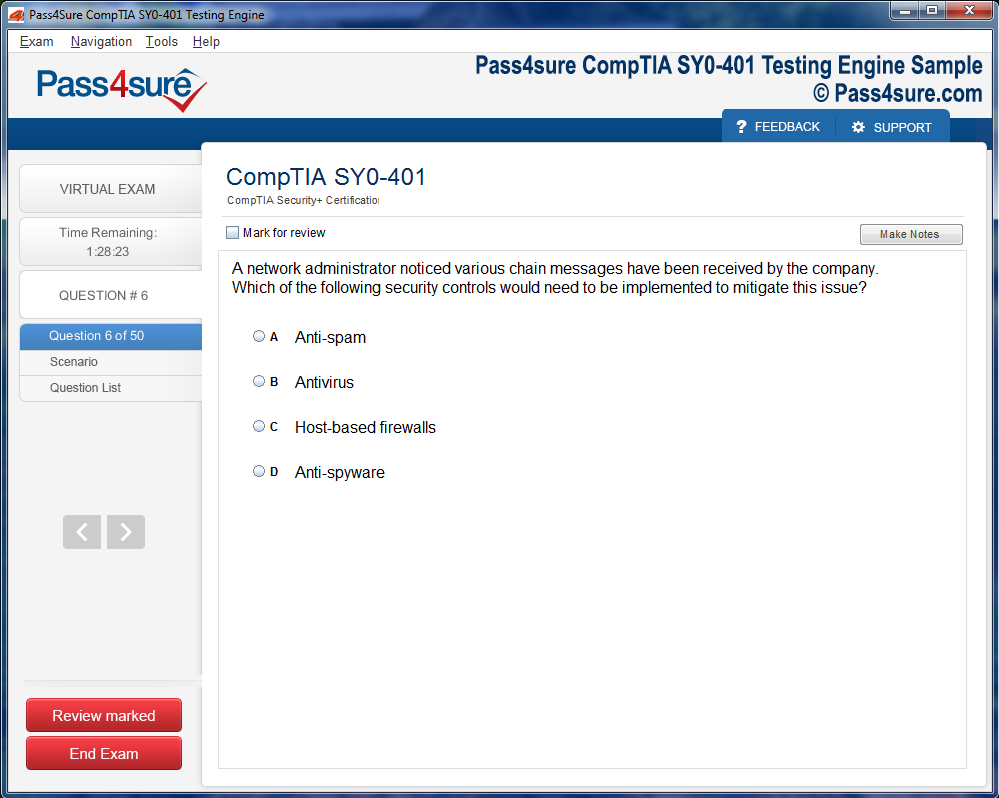
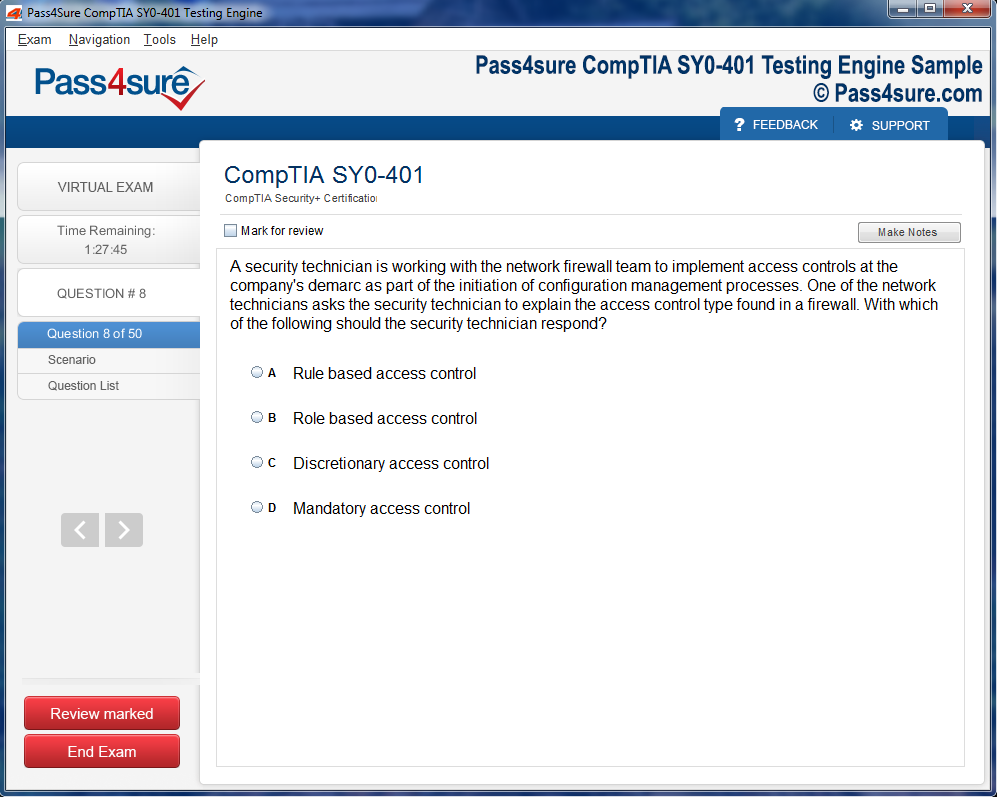
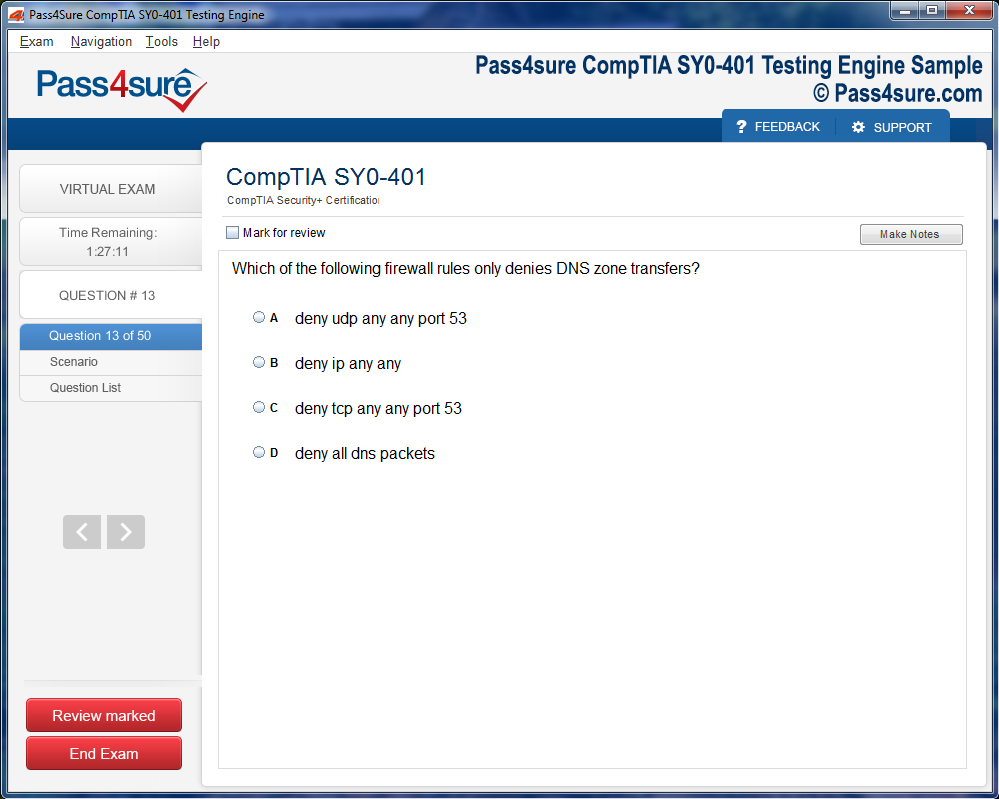
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations).
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.