Test Name: NAPLEX - North American Pharmacist Licensure Examination
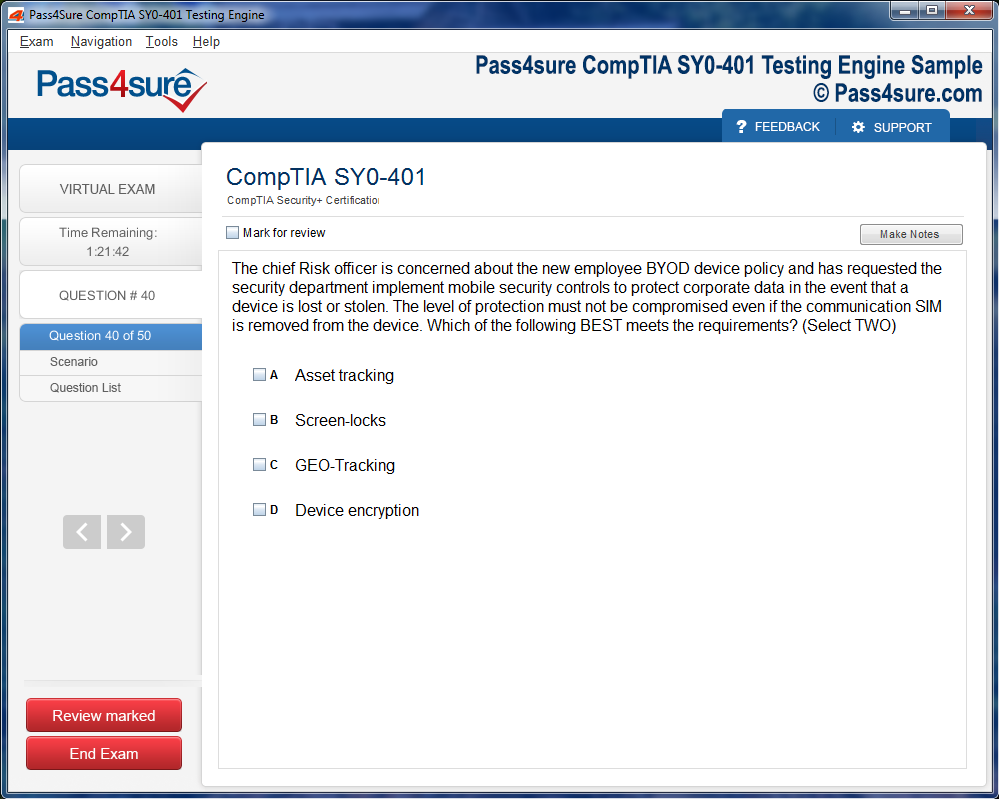
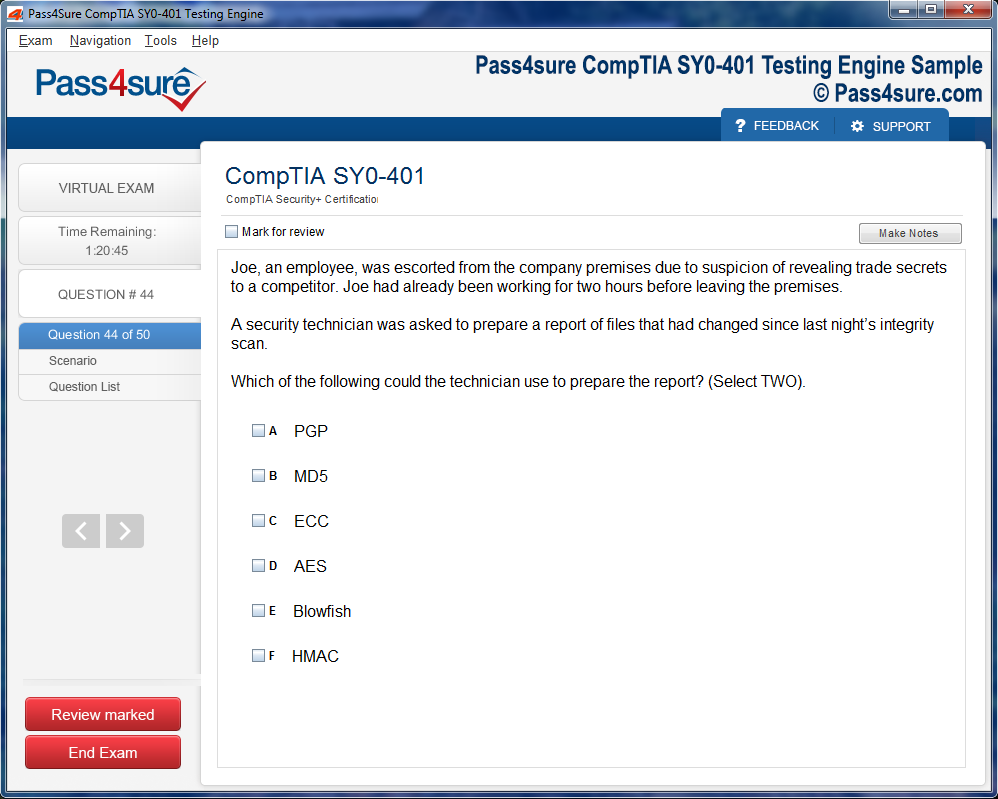
Product Screenshots
The Ultimate NAPLEX Guide: What Every Pharmacist Needs to Know
Pharmacology forms the cornerstone of every pharmacist’s knowledge. Delving into drug classes, mechanisms, and interactions is more than a memorization exercise; it is an intellectual exploration of cause and effect within the human body. Medications do not exist in isolation; they traverse complex physiological landscapes, influencing systems in subtle and profound ways. Understanding receptor affinities, enzyme inhibition, and transport mechanisms empowers a pharmacist to predict outcomes, anticipate adverse reactions, and tailor therapy for individual patients. Beyond the academic appeal, pharmacology demands precision and discipline. Each drug carries potential benefits and risks, and navigating this duality requires more than factual recall. It necessitates synthesizing information from diverse sources, recognizing patterns, and applying knowledge with discretion.
Pharmacokinetics and pharmacodynamics are particularly intricate yet indispensable aspects of this mastery. Pharmacokinetics reveals how a drug is absorbed, distributed, metabolized, and excreted, while pharmacodynamics illuminates the effects a drug exerts on the body at the molecular and systemic levels. These interrelated domains teach aspiring pharmacists to anticipate how individual patient factors can modulate therapeutic outcomes. Age, genetic variations, organ function, and comorbidities intertwine with pharmacological principles, creating a tapestry of individualized medicine. Cultivating an intimate understanding of these relationships enhances both exam performance and clinical intuition, laying the foundation for safe and effective patient care.
Moreover, pharmacology is not static; it evolves with ongoing research, novel therapies, and emerging safety data. Engaging with contemporary studies and integrating new insights into existing frameworks nurtures adaptability, a skill that proves invaluable for both licensure and long-term professional growth. In essence, mastering pharmacology is less about memorizing every molecule and more about developing a cognitive agility that allows one to interpret and act on information reliably and ethically.
Developing Clinical Judgment
The heart of pharmacy lies in clinical judgment. Beyond understanding how drugs work, a pharmacist must determine when and how to apply this knowledge to optimize patient outcomes. Clinical judgment encompasses the ability to assess patient histories, recognize deviations from normal physiology, and interpret laboratory values within the context of an evolving medical condition. It demands an appreciation for nuance; two patients may present with similar symptoms but require distinct therapeutic strategies due to underlying differences. Developing this acumen involves exposure to diverse case scenarios, reflection on decision-making processes, and careful consideration of ethical principles that govern patient care.
Case-based learning proves especially effective in cultivating clinical judgment. By encountering simulated scenarios that replicate real-world complexities, learners refine their ability to identify critical information, weigh options, and predict consequences. This method reinforces not only knowledge retention but also the mental agility required to respond to novel situations. Furthermore, it encourages metacognition, prompting students to evaluate the reasoning behind each choice and identify potential biases or gaps in understanding. Over time, these iterative experiences shape a pharmacist’s decision-making lens, enabling them to navigate uncertainty with confidence and precision.
Pharmacy is also deeply collaborative, requiring coordination with physicians, nurses, and other healthcare professionals. Effective communication skills complement clinical judgment by ensuring recommendations are conveyed clearly, respectfully, and persuasively. The ability to translate complex pharmacological data into actionable guidance for patients or colleagues is an art in itself, one that merges scientific insight with empathy and clarity. In this light, developing clinical judgment is a multidimensional endeavor, blending analytical reasoning, ethical reflection, and interpersonal competence to produce safe and effective outcomes.
Excelling in Pharmacy Calculations
Pharmacy calculations form an indispensable pillar of competence, bridging the gap between theoretical knowledge and practical application. Accurate dosing is critical, as even minor errors can lead to significant harm. Calculations extend beyond simple arithmetic, encompassing concepts such as concentration, dilution, rate of infusion, and pharmacokinetic modeling. Each problem challenges students to integrate multiple layers of information, from patient weight and renal function to drug potency and administration schedule. Success requires not only numerical proficiency but also a methodical approach to problem-solving.
To excel in this domain, students benefit from deliberate practice and structured methodologies. Breaking problems into sequential steps, double-checking assumptions, and verifying units are essential strategies. Beyond procedural rigor, developing intuition for expected outcomes fosters confidence and reduces reliance on trial and error. For instance, recognizing that a pediatric dose should not exceed a typical adult dose allows for rapid error detection. Similarly, understanding the principles behind equations, rather than simply memorizing formulas, promotes adaptability when confronted with unconventional problems.
The importance of calculations extends into clinical scenarios, where precision underpins patient safety. Pharmacists often adjust dosages based on lab results, monitor therapeutic drug levels, and provide instructions for compounded medications. Each calculation carries real-world consequences, reinforcing the necessity of both competence and attentiveness. Over time, repeated engagement with calculation problems cultivates a mindset that values accuracy, foresight, and diligence—qualities that serve pharmacists throughout their careers.
Nurturing Study Strategies
Effective preparation for the NAPLEX extends beyond the mastery of content; it requires strategic organization, focus, and resilience. Students who succeed often adopt multi-layered study approaches, blending review of core concepts with applied problem-solving. Spaced repetition, concept mapping, and scenario-based exercises facilitate long-term retention, while timed practice exams simulate real-world testing conditions and build endurance. Integrating diverse modalities—visual aids, written summaries, and interactive quizzes—accommodates varied learning styles, ensuring concepts are reinforced from multiple angles.
Consistency is equally important. Establishing a disciplined schedule fosters momentum and minimizes last-minute stress. Breaking study sessions into manageable intervals, punctuated by brief mental rests, enhances concentration and retention. Moreover, cultivating a reflective mindset allows students to monitor their progress, identify weaknesses, and adjust strategies accordingly. Preparation is not merely an accumulation of knowledge; it is the development of habits, resilience, and cognitive flexibility that enable one to perform reliably under pressure.
Mental and emotional readiness are integral components of preparation. The demands of sustained study, high stakes, and self-imposed expectations can be taxing. Techniques such as mindfulness, controlled breathing, and deliberate breaks provide essential respite, maintaining focus and preventing burnout. Peer support and mentorship further enhance motivation, offering perspective, encouragement, and practical guidance. By attending to both intellectual and emotional dimensions of preparation, candidates position themselves to navigate the NAPLEX with confidence and clarity.
Integrating Patient-Centered Care
Pharmacy is inherently human-centered. Beyond calculations and pharmacological theory, the ultimate goal of every pharmacist is to enhance patient well-being. Integrating patient-centered care into preparation involves considering how medication choices influence quality of life, adherence, and long-term health outcomes. Empathy, cultural sensitivity, and active listening shape therapeutic decisions, fostering trust and collaboration between patients and healthcare providers. This perspective elevates learning from abstract memorization to meaningful application, reinforcing the relevance of each concept studied.
Patient-centered care also entails anticipating challenges and adapting interventions accordingly. For instance, a patient with multiple chronic conditions may require careful monitoring for drug interactions, adherence support, and education about potential side effects. Pharmacists who internalize these considerations cultivate a proactive approach, identifying potential complications before they manifest. Through case studies, role-playing, and reflection on clinical experiences, students can simulate these interactions, developing both competence and compassion.
Ultimately, integrating patient-centered care into NAPLEX preparation bridges the divide between theory and practice. It instills a holistic view of pharmacy, emphasizing not only what medications do, but also how they impact individuals, families, and communities. This orientation nurtures professional identity, grounding knowledge and skills in ethical and humanistic principles that endure long after licensure.
Leveraging Technology in Preparation
Technology has become an indispensable ally in the journey toward licensure. Digital resources, practice question banks, and simulation tools provide dynamic, interactive platforms for reinforcing knowledge. Unlike static textbooks, these resources offer immediate feedback, performance analytics, and adaptive challenges that target individual weaknesses. This tailored approach accelerates learning, ensuring effort is focused on areas with the greatest potential for improvement.
Beyond content review, technology facilitates exposure to realistic scenarios. Simulated patient encounters, virtual labs, and case management exercises recreate the complexities of modern practice, enhancing both clinical judgment and practical skills. Mobile applications allow for on-the-go reinforcement, ensuring that even brief intervals of study contribute meaningfully to overall preparation. Additionally, online forums and collaborative platforms foster peer discussion, enabling learners to exchange insights, clarify doubts, and gain diverse perspectives.
Harnessing technology effectively requires intentionality. It is easy to become distracted or overwhelmed by the abundance of tools available. Structured schedules, selective resource choices, and critical evaluation of content quality ensure that technology serves as a catalyst for mastery rather than a source of confusion. In doing so, students not only prepare efficiently for the NAPLEX but also cultivate digital literacy, a skill increasingly vital in contemporary pharmacy practice.
Organizing Therapeutics into Coherent Frameworks
The foundation of pharmacology mastery lies in the ability to organize therapeutics into coherent frameworks. Random memorization leads to confusion, but when drugs are clustered according to mechanism, chemical structure, or therapeutic purpose, patterns naturally emerge. For instance, grouping antihypertensive agents reveals connections between their biochemical targets and physiological outcomes. ACE inhibitors, angiotensin receptor blockers, and direct renin inhibitors each converge on the renin-angiotensin-aldosterone system, yet subtle differences dictate patient selection. Recognizing these nuances allows students to anticipate both efficacy and adverse reactions. Beyond cardiovascular drugs, categories such as antimicrobials, analgesics, and immunomodulators each harbor their own logic. By mapping these drug families, learners create mental scaffolding that transforms overwhelming lists into intuitive structures. This approach reduces cognitive overload and enhances retention, making exam preparation both strategic and efficient.
Integrating Pharmacokinetics and Pharmacodynamics
A profound understanding of pharmacology requires integrating pharmacokinetics and pharmacodynamics, the twin pillars that explain drug action. Pharmacokinetics addresses absorption, distribution, metabolism, and excretion, describing how the body handles medications. In contrast, pharmacodynamics explores the molecular effects of drugs on receptors, enzymes, and cellular pathways. When studied in tandem, these disciplines illuminate the reasoning behind dosing schedules, potential toxicities, and drug interactions. Consider antibiotics: pharmacokinetics determines serum concentrations and tissue penetration, while pharmacodynamics predicts bactericidal versus bacteriostatic effects. For the NAPLEX, this knowledge becomes practical when evaluating clinical scenarios, such as adjusting doses for renal impairment or anticipating drug accumulation in elderly patients. Mastery of these principles empowers candidates to make informed judgments, demonstrating not only recall but clinical reasoning, a skill critical to passing the exam and excelling in real-world practice.
Predicting and Managing Adverse Effects
Pharmacology is incomplete without an emphasis on predicting and managing adverse effects. Each drug carries potential risks that must be anticipated to ensure patient safety. This begins with understanding mechanistic foundations. For example, nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit cyclooxygenase enzymes, relieving pain but simultaneously increasing the risk of gastrointestinal bleeding. Similarly, selective serotonin reuptake inhibitors may improve mood but carry the risk of hyponatremia or serotonin syndrome under certain circumstances. For NAPLEX preparation, students benefit from constructing mental checklists of common adverse effects for each drug class. Beyond memorization, it is vital to integrate this knowledge into patient-centered decision-making, such as modifying therapy for high-risk populations or counseling on warning signs. By practicing adverse effect prediction through case studies and scenario-based questions, candidates cultivate a proactive mindset, transforming pharmacology from static knowledge into actionable clinical insight.
Understanding Drug Interactions and Polypharmacy
Drug interactions present a complex but essential aspect of pharmacology mastery. The interplay between medications can profoundly affect efficacy and safety, and the NAPLEX frequently tests this understanding in multifaceted scenarios. Cytochrome P450 enzymes, a key metabolic pathway, illustrate this complexity, as multiple drugs may compete for metabolism, resulting in elevated serum concentrations or diminished effects. Polypharmacy further complicates the landscape, particularly in patients with multiple chronic conditions. By recognizing pharmacokinetic and pharmacodynamic interactions, candidates can anticipate outcomes, prevent adverse events, and select appropriate therapy. Additionally, certain interactions are synergistic or antagonistic, requiring nuanced judgment. Exercises that simulate multi-drug regimens or complex patient charts enhance this skill. A comprehensive grasp of interactions not only aids exam performance but also prepares future pharmacists to navigate the intricacies of modern clinical practice, where vigilance and foresight are indispensable.
Applying Clinical Guidelines in Pharmacology
Pharmacology does not exist in isolation; it is intertwined with evidence-based clinical guidelines that inform real-world decisions. These guidelines distill extensive research into actionable recommendations for therapy selection, monitoring, and patient education. For instance, cholesterol management guidelines dictate when statins are indicated, target LDL levels, and recommend follow-up schedules, all of which rely on pharmacological understanding. Mastering these intersections helps candidates anticipate NAPLEX questions that blend pharmacology with practical clinical application. Beyond rules and numbers, students must grasp the rationale behind guideline recommendations, understanding why certain therapies are preferred in specific populations. Integrating guideline knowledge with drug mechanisms, interactions, and adverse effect profiles produces a holistic framework, enabling confident clinical judgment under examination pressure and enhancing patient safety in professional practice.
Enhancing Retention through Active Learning
Active learning techniques transform pharmacology study from rote memorization into enduring comprehension. Concept mapping, for example, encourages visualization of relationships among drug classes, mechanisms, and side effects, revealing patterns that facilitate recall. Case-based learning bridges theory and practice, presenting realistic patient scenarios that demand application of pharmacologic principles. Flashcards remain valuable, but when paired with elaboration—explaining the “why” behind each fact—they promote deeper understanding. Spaced repetition further reinforces long-term retention, gradually strengthening memory by revisiting information at strategic intervals. Group discussions and teaching peers also solidify knowledge, as articulating concepts clarifies understanding. By embracing these strategies, learners cultivate a robust pharmacologic foundation, capable of supporting both high-stakes exams and the nuanced decisions required in everyday pharmacy practice.
Emphasizing Patient-Centered Pharmacology
At its core, pharmacology is a patient-centered discipline. Understanding drug mechanisms, interactions, and adverse effects is meaningless without considering the individual receiving therapy. Effective pharmacists anticipate complications, counsel on side effects, and personalize treatment based on age, comorbidities, and lifestyle factors. For the NAPLEX, this translates into scenario-based questions that assess the ability to balance efficacy and safety, suggest alternatives, and communicate recommendations clearly. Practicing patient counseling and reviewing mock clinical cases fosters empathy and practical skill, enhancing both exam performance and professional readiness. Furthermore, awareness of emerging therapies and updated clinical protocols ensures that candidates remain at the forefront of practice. By prioritizing the patient in every decision, learners transform pharmacology from abstract knowledge into a tangible tool for improving outcomes and building trust in healthcare settings.
Understanding Pharmacokinetics and Drug Dynamics
Pharmacokinetics forms the bedrock of effective medication management, bridging the gap between laboratory science and patient care. It involves the study of how drugs move through the body, encompassing absorption, distribution, metabolism, and excretion. Each phase of pharmacokinetics influences the drug’s efficacy and safety, making comprehension vital for accurate dosing. Absorption determines how quickly a drug enters the bloodstream, while distribution reflects how it disperses among tissues and organs. Metabolism, primarily occurring in the liver, transforms drugs into active or inactive forms, and excretion, most often via the kidneys, removes substances from the body. Understanding these processes allows pharmacists to anticipate drug behavior and tailor treatments according to individual patient characteristics.
The dynamic interaction between drugs and receptors underpins pharmacodynamics. This field examines how medications exert their effects at cellular or systemic levels. Concepts such as receptor binding, agonist and antagonist activity, and dose-response relationships are central to understanding therapeutic outcomes. For instance, two patients receiving the same medication might respond differently due to variations in receptor sensitivity or genetic factors affecting metabolism. Recognizing these nuances helps in predicting both efficacy and potential adverse effects. Mastery of pharmacokinetics and pharmacodynamics requires more than memorization; it demands the ability to apply principles to complex clinical scenarios, where multiple variables converge.
Clinical application of these principles extends to special populations, including pediatrics, geriatrics, and patients with organ dysfunction. Children, for example, may metabolize drugs faster or slower than adults depending on age, growth, and developmental stage. Similarly, older adults often experience reduced renal or hepatic function, necessitating careful dose adjustments. In both cases, integrating pharmacokinetic knowledge with patient-specific factors ensures safety and maximizes therapeutic benefit. Pharmacists must maintain vigilance in monitoring therapy, interpreting laboratory results, and modifying treatment plans when necessary. The NAPLEX evaluates these abilities indirectly through questions that require analytical reasoning rather than rote calculation.
Precision in Dosage and Compounding
Precision in dosage calculation is fundamental to safe and effective pharmacy practice. Every calculation must account for patient weight, age, organ function, and concurrent medications. Even minor errors can have significant consequences, especially when dealing with potent medications or narrow therapeutic index drugs. Compounding adds another layer of complexity, requiring the pharmacist to convert between forms, concentrations, and volumes while maintaining sterility and stability. Compounding exercises often include the preparation of suspensions, ointments, or intravenous admixtures, demanding meticulous attention to measurement and technique.
Understanding the principles behind each formula and process allows pharmacists to adjust calculations with confidence. Memorizing steps without comprehension can lead to mistakes when confronted with unfamiliar scenarios. For example, a compounded intravenous solution may require adjustment based on the patient’s current laboratory values or fluid restrictions. Recognizing the relationships between concentration, volume, and rate ensures safe preparation and administration. Systematic approaches, such as verifying calculations, cross-referencing orders, and performing independent checks, serve as safeguards against errors. These practices reflect professional responsibility and cultivate trust in patient care.
Consistency in execution reinforces competence. Regular practice with diverse calculation types, including oral medications, parenteral therapies, and compounded preparations, builds both speed and accuracy. Over time, pharmacists develop a mental framework for approaching problems, allowing them to navigate complex tasks efficiently. This process mirrors real-world pharmacy practice, where rapid and precise decision-making is essential. By integrating theoretical knowledge with practical exercises, candidates strengthen their ability to perform confidently under exam conditions and in professional environments.
Interpreting Laboratory Data for Medication Management
Laboratory data interpretation plays a pivotal role in guiding medication therapy. Pharmacists must understand normal ranges, trends, and the clinical significance of various tests to make informed decisions. Renal function tests, liver enzyme levels, and electrolyte measurements are among the most frequently referenced parameters. Alterations in these values often necessitate dose adjustments or monitoring strategies. For instance, impaired kidney function can reduce drug clearance, increasing the risk of toxicity unless doses are modified appropriately.
Beyond individual values, the integration of trends over time provides deeper insight into patient response. Rising or falling biomarkers can indicate changes in disease progression, therapeutic efficacy, or potential adverse effects. Pharmacists analyze these patterns in conjunction with clinical signs, symptoms, and medication history to guide therapy. Understanding the mechanisms behind laboratory abnormalities allows for proactive intervention, improving patient outcomes. The ability to interpret complex data is both a cognitive and practical skill, cultivated through exposure to real-world scenarios and focused study.
Laboratory-guided therapy is particularly critical for medications with narrow therapeutic indices, such as anticoagulants, anticonvulsants, or immunosuppressants. Accurate interpretation prevents underdosing, which can lead to treatment failure, and overdosing, which can cause harm. Pharmacists often calculate individualized doses based on creatinine clearance, liver function, or other biomarkers, reinforcing the intersection between mathematical precision and clinical judgment. This competency reflects the holistic understanding expected of practitioners and the level of analytical thinking assessed by licensing examinations.
Mastering Drug Interactions and Safety Considerations
Drug interactions represent a complex but essential component of pharmacy practice. Medications can interact in ways that enhance, diminish, or alter their intended effects. These interactions may occur at the level of absorption, metabolism, protein binding, or receptor activity. Understanding potential interactions allows pharmacists to anticipate risks and implement strategies to mitigate harm. For example, concurrent administration of certain antibiotics and anticoagulants may increase bleeding risk, requiring dose adjustment or alternative therapy. Recognizing these relationships involves both knowledge of pharmacology and critical reasoning skills.
Safety considerations extend beyond drug interactions to encompass adverse effects, contraindications, and patient-specific risk factors. Pharmacists evaluate the appropriateness of therapy by considering age, comorbidities, allergies, and prior drug reactions. For instance, medications with sedative properties may pose a heightened risk for falls in elderly patients. Vigilant monitoring, patient education, and careful documentation ensure that therapy remains both effective and safe. Developing a systematic approach to evaluating risk enhances clinical judgment and minimizes errors.
Continuous learning is integral to maintaining expertise in drug interactions and safety. As new medications and evidence emerge, pharmacists must update their knowledge and adjust practice accordingly. Simulated case studies, review exercises, and evidence-based guidelines provide structured opportunities to apply principles in diverse scenarios. These experiences cultivate an analytical mindset and reinforce the pharmacist’s role as a vigilant guardian of patient well-being. The integration of pharmacologic knowledge with critical assessment skills exemplifies the holistic proficiency expected of professionals in the field.
Strategies for Time Management and Exam Readiness
Time management is a critical element of effective exam preparation and professional practice. The NAPLEX, with its extensive question set and time constraints, challenges candidates to balance accuracy with efficiency. Developing a structured study plan ensures comprehensive coverage of essential topics while allowing for repeated practice in calculation, pharmacokinetics, and clinical reasoning. Allocating time based on personal strengths and weaknesses optimizes learning and reduces stress. For instance, dedicating focused sessions to complex calculation problems or laboratory data interpretation can strengthen proficiency in high-stakes areas.
Simulated exams and timed practice sessions provide realistic preparation, fostering familiarity with the pacing and cognitive demands of the testing environment. These exercises encourage the development of intuitive strategies, such as identifying familiar question types, prioritizing problems, and verifying answers efficiently. Over time, repeated exposure enhances both speed and confidence, translating into improved performance. The combination of structured study, practical application, and reflective review cultivates a resilient approach to examination challenges.
Beyond preparation, time management is equally vital in daily pharmacy practice. Efficient workflow, prioritization of tasks, and systematic problem-solving ensure that patient care remains uninterrupted and accurate. Pharmacists must navigate prescription verification, counseling, inventory management, and clinical interventions within finite time frames. The skills honed during exam preparation carry forward into professional routines, reinforcing the synergy between academic mastery and real-world application. A disciplined approach to time management fosters competence, reduces error, and enhances overall effectiveness in both testing and practice settings.
Developing Clinical Reasoning and Decision-Making Skills
Clinical reasoning represents the synthesis of knowledge, analysis, and judgment in guiding patient care. It involves integrating pharmacologic principles, laboratory data, patient history, and therapeutic guidelines to arrive at safe and effective decisions. Developing these skills requires exposure to diverse clinical scenarios, allowing practitioners to recognize patterns, anticipate outcomes, and adjust therapy accordingly. Unlike rote memorization, clinical reasoning emphasizes the application of knowledge to dynamic and unpredictable situations.
Decision-making in pharmacy is iterative, combining observation, assessment, and intervention. Each step requires critical evaluation of available information and thoughtful consideration of potential consequences. For example, adjusting an antihypertensive regimen based on blood pressure trends and comorbid conditions demands both analytical precision and clinical insight. Reflective practice, case discussion, and simulation exercises enhance this competency, reinforcing the link between theoretical understanding and practical application. Pharmacists who cultivate strong clinical reasoning skills are better equipped to navigate complex patient needs and contribute meaningfully to healthcare teams.
The development of judgment extends to ethical considerations and professional responsibility. Balancing patient safety, therapeutic efficacy, and evidence-based practice requires careful thought and integrity. Pharmacists must communicate effectively, advocate for optimal treatment, and recognize limitations in their knowledge or authority. By fostering a thoughtful, reflective approach to clinical decision-making, practitioners not only ensure safe outcomes but also model professionalism and accountability. Mastery of these skills represents the culmination of education, experience, and continuous intellectual engagement in the field of pharmacy.
Clinical Decision-Making and Patient Care
Clinical decision-making forms the foundation of modern pharmacy practice, representing the confluence of scientific knowledge, experiential insight, and human empathy. At its core, the practice demands more than rote memorization; it necessitates the capacity to evaluate multifaceted patient scenarios, synthesize disparate data, and chart a pathway that prioritizes both safety and therapeutic effectiveness. Pharmacists serve not merely as dispensers of medications but as integral participants in a patient’s journey toward wellness, balancing the intricacies of pharmacology with the nuances of human behavior. In this context, clinical decision-making is both an art and a science, tested rigorously in professional licensure assessments. The challenge lies in anticipating complications, weighing competing options, and making choices that reflect an understanding of the patient as a holistic being rather than a collection of symptoms.
Pharmacists encounter situations where the margin between optimal and suboptimal care is razor-thin. For instance, a patient managing chronic heart failure and concurrent diabetes may present with subtle signs of infection. The decision to select an antibiotic requires careful consideration of renal function, potential drug-drug interactions, and the cumulative burden of polypharmacy. In these moments, a pharmacist’s reasoning extends beyond standard guidelines; it demands foresight, creativity, and precision. The ability to navigate such multidimensional problems distinguishes practitioners who can adapt to the fluidity of real-world clinical environments from those who operate strictly within theoretical confines. Mastery of clinical decision-making, therefore, is cultivated through iterative practice, exposure to diverse cases, and reflective engagement with one’s choices.
Patient care transcends pharmacological intervention. Counseling, education, and reassurance are pillars of effective practice. Pharmacists must articulate complex medical information in terms comprehensible to patients, ensuring adherence while fostering trust. Explaining potential adverse effects, dietary considerations, and the timing of administration requires patience and clarity. Beyond instruction, pharmacists anticipate questions, address misconceptions, and tailor guidance to individual lifestyles. These interactions are not peripheral; they are central to successful outcomes. Exams often simulate such encounters, challenging candidates to integrate interpersonal skill with clinical reasoning. Developing these soft skills entails more than memorization—it calls for active engagement through role-playing, workshops, and the analysis of narrative case studies. Each patient interaction becomes an opportunity to refine judgment, empathy, and communication.
Integrating Pharmacology and Patient Context
Effective clinical decision-making requires a seamless integration of pharmacology with patient-specific contexts. Understanding a drug’s mechanism, metabolism, and potential adverse effects is foundational. However, translating this knowledge into actionable plans requires attention to comorbidities, age-related considerations, and the patient’s socio-economic environment. For example, selecting a hypoglycemic agent involves evaluating renal clearance, risk of hypoglycemia, and compatibility with other cardiovascular medications. Similarly, dosing adjustments in hepatic impairment necessitate a nuanced grasp of pharmacokinetics alongside vigilance for clinical manifestations. The synthesis of theoretical knowledge with patient realities transforms abstract information into tangible solutions, guiding interventions that are both safe and effective.
Pharmacists must also anticipate the longitudinal trajectory of disease progression. Chronic illnesses, such as diabetes, hypertension, and heart failure, unfold over months and years, with medication needs evolving alongside complications. Predicting potential adverse outcomes or therapy resistance requires critical thinking and foresight. In practice, this might involve preemptively adjusting dosages, introducing adjunctive therapies, or monitoring for early signs of organ dysfunction. These anticipatory actions exemplify the proactive dimension of pharmacy care, wherein clinical reasoning extends beyond the immediate snapshot of patient status to encompass future possibilities. The capacity to harmonize pharmacologic principles with the fluidity of patient needs underscores the sophistication required for competent practice.
Navigating Multidimensional Clinical Scenarios
Clinical cases frequently present with overlapping complexities that challenge linear reasoning. A patient may exhibit symptoms that straddle multiple organ systems, with interventions in one domain influencing outcomes elsewhere. Managing polypharmacy requires an intricate dance: balancing therapeutic efficacy, minimizing adverse interactions, and preserving patient adherence. Consider a patient with chronic kidney disease, hypertension, and depression. Each medication choice reverberates across other systems, demanding vigilant analysis. Pharmacists must prioritize interventions, determining which symptoms pose the greatest immediate risk and which therapeutic modifications can mitigate long-term complications. The capacity to deconstruct intricate cases into manageable components while preserving a holistic perspective is central to both exam performance and professional competence.
Strategic prioritization is vital. Not all clinical issues carry equal weight, and discerning urgency requires an understanding of pathophysiology and pharmacodynamics. Decisions are rarely binary; they involve weighing risks, benefits, and patient preferences. For instance, initiating a potent immunosuppressant may quell inflammation but increase susceptibility to infection. Evaluating such trade-offs demands not only knowledge but moral reasoning and empathy. By cultivating a structured approach to complex scenarios, pharmacists refine their ability to respond decisively, maintaining patient safety while optimizing therapeutic outcomes. In exams, questions often replicate these multidimensional scenarios, testing analytical agility and practical foresight simultaneously.
Patient Counseling and Communication Mastery
Communication is an inseparable component of clinical decision-making. The capacity to convey therapeutic instructions, discuss adverse effects, and encourage adherence hinges on clarity and interpersonal acumen. Pharmacists must anticipate the patient’s knowledge gaps, fears, and misconceptions, framing explanations in accessible language. Beyond verbal instruction, nonverbal cues, tone, and empathetic engagement reinforce the message, enhancing receptivity and trust. Counseling is not a perfunctory task but a dynamic interaction that can influence adherence, outcomes, and overall patient satisfaction. Clinical reasoning is incomplete without considering how patients internalize information and translate it into behavior.
In practice, counseling involves layering information strategically. Initial discussions may focus on medication purpose, dosage, and timing, with subsequent sessions addressing side effects, lifestyle modifications, and monitoring. Role-playing exercises and simulation-based training strengthen these skills, fostering confidence in both routine and challenging interactions. Importantly, pharmacists must remain attuned to individual differences—cultural context, health literacy, and prior experiences shape comprehension and engagement. By integrating communication mastery with clinical knowledge, pharmacists not only prescribe safely but empower patients, transforming care from a transaction into a collaborative partnership.
Ethical Considerations in Therapeutic Decisions
Ethical reasoning permeates all aspects of pharmacy practice. Pharmacists confront dilemmas wherein information is incomplete, conflicting, or ambiguous, demanding principled judgment. Decisions often involve trade-offs between competing values: maximizing efficacy, minimizing harm, ensuring equity, and respecting autonomy. For example, a patient may request a treatment that conflicts with evidence-based guidelines. Navigating such scenarios requires tact, transparency, and adherence to professional standards. Ethical frameworks guide decision-making, yet their application is contextual, informed by clinical insight, patient circumstances, and regulatory requirements.
Professional judgment also entails responsibility for outcomes. Pharmacists must recognize the limitations of their knowledge, seek consultation when appropriate, and document rationales for interventions. Reflective practice—reviewing past decisions to identify strengths, gaps, and biases—enhances ethical competence over time. Exams evaluate this capacity through ambiguous or challenging case scenarios, prompting candidates to weigh options thoughtfully, anticipate consequences, and justify recommendations. Mastery of ethical reasoning is inseparable from clinical acumen, reinforcing the pharmacist’s role as a trustworthy and conscientious healthcare professional.
Evidence-Based Practice and Guideline Application
Evidence-based practice anchors clinical decision-making in empirical research, translating data into patient-centered interventions. Pharmacists must appraise literature critically, discerning methodological rigor, relevance, and applicability. Guideline familiarity provides a framework, yet individual patient factors necessitate adaptation. For instance, while protocols may dictate first-line therapy, comorbidities, prior drug reactions, or patient preferences may warrant deviation. The ability to reconcile evidence with real-world complexity distinguishes adept practitioners, fostering both efficacy and personalization.
Continual learning is central to this process. The pharmacological landscape evolves rapidly, with new therapies, safety alerts, and clinical trials influencing practice. Lifelong engagement with research, professional development, and interprofessional dialogue ensures that decisions remain current and evidence-informed. Integrating data appraisal into daily practice cultivates analytical rigor, enhancing confidence and precision. In exams, scenarios may simulate decision-making under uncertain or evolving evidence, challenging candidates to balance guideline fidelity with pragmatic judgment. Such preparation reinforces the integration of theory and practice, equipping pharmacists to navigate dynamic healthcare environments effectively.
Interprofessional Collaboration and Patient Advocacy
Clinical decision-making rarely occurs in isolation. Pharmacists operate within teams, collaborating with physicians, nurses, and allied health professionals to optimize outcomes. Effective collaboration requires clear communication, mutual respect, and shared understanding of goals. Pharmacists contribute unique expertise in pharmacotherapy, identifying interactions, suggesting alternatives, and monitoring safety. By advocating for the patient’s best interest, they bridge gaps between disciplines, ensuring cohesive and informed care. Active participation in interdisciplinary discussions strengthens reasoning, providing perspectives that enrich decision-making.
Patient advocacy extends beyond professional dialogue. Pharmacists act as intermediaries between patients and the healthcare system, facilitating access to medications, navigating insurance complexities, and educating about self-management strategies. This role reinforces the ethical imperative to prioritize patient welfare, empowering individuals to engage actively in their health journey. Case-based exercises, team simulations, and reflective practice cultivate these collaborative and advocacy skills, translating into both exam readiness and effective real-world practice. The capacity to merge clinical insight, ethical reasoning, and teamwork epitomizes comprehensive pharmacy care.
Understanding the Foundation of Pharmacological Knowledge
The cornerstone of effective NAPLEX preparation lies in a robust understanding of pharmacological principles. Without a firm grasp of drug mechanisms, interactions, and therapeutic applications, candidates risk faltering when integrating knowledge into clinical scenarios. Pharmacology is not merely the memorization of drug names and doses; it requires comprehension of physiological systems, biochemical pathways, and molecular targets. Recognizing patterns in drug classes, such as shared adverse effects or similar mechanisms, facilitates rapid recall under examination pressure.
Integrating foundational sciences, such as physiology, microbiology, and pathology, into study routines enhances contextual understanding. For instance, understanding renal and hepatic metabolism can illuminate why certain drugs necessitate dosage adjustments or monitoring. The synergy between core sciences and applied pharmacology allows candidates to approach questions with analytical reasoning rather than rote memorization. Reinforcing these connections through visual aids, diagrams, and scenario-based learning deepens retention and fosters a more holistic view of clinical therapeutics.
Mastering Calculations Through Methodical Practice
Dosage calculations and pharmacokinetic problem-solving form a critical component of the NAPLEX, requiring precision and mental agility. Candidates often experience anxiety in this domain, yet systematic, methodical practice can alleviate stress and improve performance. Breaking down complex calculations into incremental steps ensures accuracy and reduces the risk of errors during high-pressure exam situations.
Utilizing multiple modalities of practice, such as handwritten problem-solving, digital simulations, and timed exercises, cultivates both speed and accuracy. Spaced repetition of calculation exercises prevents skill decay and strengthens numerical intuition. Equally important is understanding the rationale behind each calculation, such as why loading doses are employed or how half-life influences dosing intervals. By combining repetitive practice with conceptual comprehension, students develop a reliable, adaptable approach to calculations, essential for both the exam and real-world pharmacy practice.
Integrating Clinical Reasoning with Case-Based Learning
Clinical reasoning serves as the linchpin of NAPLEX success, bridging theoretical knowledge with practical application. Engaging in case-based learning allows candidates to synthesize multiple layers of information, from pharmacodynamics to patient-specific variables. These scenarios encourage analytical thinking, prompting students to consider drug interactions, contraindications, and individualized treatment plans.
Effective case integration also involves reflective practice. After working through a scenario, reviewing decision pathways, and identifying alternative strategies fortifies cognitive flexibility. Exposure to diverse clinical cases, encompassing chronic diseases, acute conditions, and specialized populations, ensures familiarity with a broad spectrum of patient presentations. The iterative cycle of practice, reflection, and review sharpens judgment, reinforces knowledge, and instills confidence in applying pharmacological principles under exam conditions.
Leveraging Diverse Study Resources
Diversity in study materials enriches learning and accommodates different cognitive styles. Comprehensive textbooks offer structured, sequential coverage of core topics, ensuring no essential content is overlooked. Conversely, digital question banks provide dynamic engagement through scenario-based questions, instant feedback, and adaptive difficulty levels. Supplementing these resources with video tutorials and interactive modules caters to visual and auditory learners, translating abstract concepts into accessible understanding.
Collaborative learning further enhances comprehension. Study groups create forums for discussion, enabling students to articulate reasoning, challenge assumptions, and clarify misunderstandings. Mentorship programs or peer-to-peer coaching offer guidance and insight from those with prior exam experience, providing strategies for efficient preparation. Staying updated with evolving clinical guidelines and newly approved medications fosters readiness for emerging practice trends, ensuring candidates remain current and clinically competent.
Developing Resilient Study Habits
Effective study strategies extend beyond content mastery to encompass discipline and consistency. Establishing a structured study schedule cultivates routine, reduces procrastination, and optimizes cognitive performance. Allocating time according to individual strengths and weaknesses ensures a balanced approach, emphasizing areas requiring additional reinforcement while maintaining proficiency in stronger domains.
Variety within study sessions maintains engagement and prevents cognitive fatigue. Rotating between reading, problem-solving, and active recall exercises stimulates different cognitive pathways, enhancing retention and understanding. Incorporating short, purposeful breaks prevents burnout and refreshes mental focus. Additionally, maintaining a conducive environment—quiet, organized, and free from distractions—supports sustained attention and productivity, critical for comprehensive exam preparation.
Psychological Preparation and Stress Management
The psychological dimension of exam readiness is often underestimated yet profoundly influential. High-stakes testing induces stress that can impair memory recall and decision-making. Incorporating mindfulness techniques, such as meditation, deep-breathing exercises, and visualization, mitigates anxiety and promotes mental clarity. Positive reinforcement, self-affirmation, and goal-setting sustain motivation and build resilience.
Physical well-being is intrinsically linked to cognitive performance. Adequate sleep, balanced nutrition, and regular exercise bolster memory, attention, and endurance. Structured routines that integrate physical activity and restorative practices create mental and physical equilibrium, reducing susceptibility to fatigue and stress. Recognizing the importance of self-care and maintaining a supportive study-life balance equips candidates to approach preparation and examination with confidence and composure.
Enhancing Memory Retention Through Active Techniques
Long-term retention is a pivotal element of NAPLEX preparation, demanding active engagement with material rather than passive exposure. Techniques such as spaced repetition, interleaved practice, and self-testing consolidate knowledge into durable memory traces. Revisiting previously studied material at strategic intervals strengthens recall and counteracts forgetting, particularly for intricate drug information and therapeutic protocols.
Concept mapping and visual association further reinforce understanding by linking ideas in meaningful ways. Creating personalized mnemonics or story-based associations enables rapid retrieval during high-pressure examination scenarios. Integrating multiple sensory modalities, such as reading aloud or drawing diagrams, engages different neural pathways, enhancing both comprehension and memorization. By employing these active learning strategies consistently, candidates cultivate a robust, accessible knowledge base capable of withstanding the demands of the exam.
Embarking on a career in pharmacy is a pursuit that blends intellectual rigor with compassionate service. The pathway toward professional mastery demands more than memorization; it requires a synthesis of knowledge, analytical skill, and moral discernment. Every stage of this journey—from foundational coursework to clinical exposure—cultivates a mindset capable of navigating complex therapeutic landscapes. Pharmacists do not merely dispense medications; they interpret biochemical interactions, anticipate adverse outcomes, and guide patients through nuanced treatment pathways. Success in this field emerges from a delicate equilibrium of cognitive precision and empathetic engagement, where each decision carries the weight of human well-being.
The process of cultivating expertise is neither linear nor brief. It encompasses rigorous academic training, immersive experiential learning, and disciplined self-reflection. Early exposure to clinical scenarios fosters the development of critical reasoning, enabling the practitioner to synthesize information from diverse sources. Equally important is the cultivation of humility—the recognition that knowledge is expansive, evolving, and often incomplete. Professional mastery in pharmacy is therefore a dynamic endeavor, one that intertwines intellectual acumen with ethical responsibility, demanding constant vigilance and intentional practice.
Cognitive Strategies for Deep Understanding
The acquisition of knowledge in pharmacy transcends rote memorization. Effective learning is grounded in active engagement, mental integration, and contextual application. Cognitive strategies that facilitate deep understanding enable practitioners to navigate multifaceted clinical problems with agility and precision. For example, constructing mental frameworks that connect pharmacological mechanisms with physiological responses allows for a comprehensive grasp of therapeutic principles. Similarly, iterative rehearsal, spaced repetition, and reflective synthesis enhance retention while fostering adaptive expertise.
Critical thinking forms the cornerstone of clinical reasoning. When confronted with ambiguous or evolving patient scenarios, the ability to evaluate evidence, anticipate outcomes, and weigh alternatives becomes indispensable. Integrating information from pharmacology, pathophysiology, and patient-specific factors requires mental dexterity and sustained focus. Moreover, the development of metacognitive awareness—attuning to the processes by which one thinks and learns—empowers pharmacists to self-correct, refine strategies, and maintain a trajectory of continuous growth.
The Role of Ethical Deliberation
Pharmacy is inherently a moral enterprise, where decisions carry profound implications for individual and public health. Ethical deliberation is not an abstract exercise but a practical necessity, guiding choices in situations of uncertainty or conflict. Pharmacists confront dilemmas ranging from balancing therapeutic efficacy against potential harm to ensuring equitable access to care. Cultivating ethical judgment involves integrating professional codes, societal expectations, and personal integrity into clinical decision-making.
The cultivation of ethical acuity begins during formative training and extends throughout professional life. Engaging with case studies, ethical discourse, and reflective practice strengthens the capacity to navigate moral complexity. Beyond individual practice, ethical deliberation shapes the profession itself, fostering a culture of accountability, transparency, and patient-centered advocacy. Pharmacists who embrace ethical reasoning contribute not only to the health of those they serve but also to the credibility and integrity of the profession as a whole.
Clinical Application and Experiential Learning
Knowledge in pharmacy attains its fullest meaning when applied within real-world contexts. Experiential learning bridges the gap between theory and practice, providing opportunities to develop technical proficiency, interpersonal skill, and clinical judgment. Through rotations in hospitals, community pharmacies, and specialized care settings, practitioners encounter diverse patient populations, medical conditions, and therapeutic regimens. Each encounter becomes a case study, a chance to refine skills, test assumptions, and integrate knowledge into actionable solutions.
The iterative nature of clinical experience fosters resilience and adaptability. Errors and near misses, when approached reflectively, catalyze improvement and strengthen decision-making frameworks. Equally important is the cultivation of interpersonal competence; effective communication with patients, caregivers, and interdisciplinary teams enhances outcomes, builds trust, and reduces the likelihood of adverse events. Experiential learning, therefore, is both an intellectual and relational endeavor, nurturing the holistic capabilities required of a competent and compassionate pharmacist.
Lifelong Learning as a Professional Imperative
The conclusion of formal examinations does not signify the end of education in pharmacy. Rather, it inaugurates a sustained commitment to lifelong learning, a principle central to maintaining professional competence. The landscape of healthcare is dynamic, characterized by continuous innovations in pharmacotherapy, evolving regulatory standards, and emerging public health challenges. Pharmacists who remain intellectually curious, agile, and engaged position themselves to anticipate changes, adopt evidence-based practices, and contribute meaningfully to patient care.
Lifelong learning encompasses multiple dimensions. It involves ongoing acquisition of clinical knowledge, mastery of emerging technologies, and refinement of communication skills. It also includes ethical vigilance, cultural sensitivity, and reflective practice. Engaging in professional networks, attending educational symposia, and mentoring peers are not merely ancillary activities; they constitute deliberate strategies for sustaining expertise. In essence, lifelong learning transforms the practitioner from a repository of information into a dynamic agent of innovation, advocacy, and excellence in healthcare delivery.
The Interconnected Role of Pharmacists in Healthcare
Pharmacists occupy a unique nexus within the healthcare ecosystem, integrating scientific knowledge, clinical reasoning, and patient advocacy. Their role extends beyond medication management to encompass education, safety oversight, and interdisciplinary collaboration. Pharmacists interpret complex pharmacological data, reconcile drug interactions, and ensure therapeutic adherence, safeguarding patients against preventable harm. Simultaneously, they serve as accessible resources for health literacy, empowering individuals to participate actively in their care.
The societal trust vested in pharmacists underscores the responsibility inherent in this profession. Accurate, ethical, and patient-centered practice forms the foundation of this trust, demanding rigorous attention to detail and unwavering professional integrity. The decisions made by pharmacists ripple outward, influencing health outcomes, institutional practices, and community well-being. Recognizing the scope of this influence reinforces the importance of continual development, reflective practice, and conscientious engagement across every dimension of professional activity.
Cultivating a Mindset of Adaptability and Innovation
The modern healthcare environment is defined by constant transformation, technological advancement, and unforeseen challenges that demand flexibility and foresight. Pharmacists, like many healthcare professionals, operate at the intersection of science, technology, and patient-centered care, where rigid routines are increasingly insufficient. Cultivating a mindset of adaptability and innovation is no longer optional; it is essential for professional growth, enhanced patient outcomes, and meaningful contributions to the evolving healthcare ecosystem.
Adaptability in pharmacy practice involves more than simply responding to immediate changes. It requires an anticipatory stance, a capacity to recognize emerging trends, and a willingness to integrate new information into daily practice. Whether it is adopting updated clinical guidelines, navigating the integration of electronic health records, or adjusting to the introduction of novel therapeutics, adaptable pharmacists embrace change with agility rather than resistance. This mindset enables practitioners to remain effective in environments that are dynamic, complex, and often unpredictable.
Innovation, on the other hand, extends beyond reactive adaptability. It entails a proactive approach to problem-solving, the courage to challenge established norms, and the capacity to synthesize knowledge from multiple disciplines. Innovative pharmacists identify gaps in care, design creative solutions, and implement strategies that improve patient outcomes, optimize workflows, and enhance operational efficiency. Innovation thrives where curiosity intersects with critical thinking and is fueled by a commitment to continuous learning.
One of the key drivers of innovation in pharmacy is technological integration. Advances in digital health tools, artificial intelligence, and data analytics have revolutionized patient care, yet their potential can only be fully realized by professionals willing to engage with these resources thoughtfully. Pharmacists who leverage predictive analytics can anticipate medication-related risks, personalize therapeutic regimens, and monitor outcomes with unprecedented precision. Similarly, telepharmacy and digital communication platforms enable timely interventions, improved patient education, and more efficient coordination of care across multidisciplinary teams. By integrating technology into practice with creativity and insight, pharmacists move beyond traditional roles and contribute to a more responsive, patient-centered healthcare system.
An adaptive and innovative mindset also supports resilience, an increasingly vital attribute in healthcare. Change often brings uncertainty, and the ability to navigate ambiguity with composure is critical. Pharmacists who approach challenges with flexibility, curiosity, and a solution-oriented attitude are less likely to experience professional burnout and more likely to find fulfillment in their work. This resilience is reinforced by a growth-oriented perspective that reframes obstacles as opportunities for learning and professional development. Mistakes or setbacks are no longer viewed as failures but as catalysts for reflection, refinement, and improved decision-making.
Collaboration serves as another cornerstone of adaptability and innovation. The complexity of modern healthcare requires pharmacists to work seamlessly with physicians, nurses, data analysts, and other allied health professionals. By cultivating strong communication skills and a collaborative mindset, pharmacists can contribute novel insights, integrate diverse perspectives, and co-create solutions that improve clinical and operational outcomes. Interdisciplinary collaboration also stimulates creativity, as exposure to varied experiences, thought processes, and problem-solving approaches encourages the generation of ideas that might not arise within siloed practice.
Embracing adaptability and innovation in pharmacy is not limited to technology or collaboration; it also manifests in patient engagement and education. Patients today are more informed and active participants in their care than ever before, demanding personalized, transparent, and evidence-based interventions. Pharmacists who adapt their communication strategies, tailor educational materials, and innovate methods for improving adherence and self-management create a more meaningful therapeutic relationship. This patient-centered innovation ensures that advancements in medicine and technology translate into tangible improvements in health outcomes.
Moreover, a mindset of adaptability and innovation encourages lifelong learning. The pace of medical research, regulatory updates, and emerging therapies is relentless, and static knowledge rapidly becomes obsolete. Pharmacists who actively seek continuing education, participate in professional development, and engage with evolving literature remain at the forefront of their field. This commitment to learning reinforces both competence and confidence, enabling professionals to approach challenges with informed judgment and a sense of mastery.
Ethical awareness is another dimension enriched by adaptability and innovation. In a rapidly changing healthcare environment, pharmacists encounter complex ethical dilemmas involving emerging treatments, digital patient data, and resource allocation. An innovative mindset allows for critical evaluation of options, creative problem-solving, and ethically sound decision-making. Pharmacists who balance ingenuity with moral responsibility ensure that advancements benefit patients while upholding professional standards.
Organizational contribution is a further aspect of professional growth supported by these qualities. Adaptable and innovative pharmacists often emerge as leaders within their institutions, shaping policy, guiding process improvements, and mentoring colleagues. Their capacity to anticipate challenges, propose solutions, and implement change creates a culture of continuous improvement, fostering both staff development and enhanced patient care. Leadership in this context is not about hierarchy but about influence, initiative, and the ability to inspire others toward shared goals.
Finally, cultivating adaptability and innovation transforms professional identity. Pharmacists are no longer solely dispensers of medication; they are integrators of knowledge, coordinators of care, and innovators in clinical practice. This expanded role requires courage, creativity, and the willingness to embrace complexity. Those who adopt this mindset not only improve their practice but also shape the broader trajectory of healthcare, contributing to systems that are more efficient, patient-centered, and responsive to change.
In essence, the development of an adaptive and innovative mindset is a multidimensional process that encompasses technological engagement, collaborative practice, resilience, patient-centered care, lifelong learning, ethical discernment, and leadership. Pharmacists who cultivate these qualities are well-positioned to navigate the evolving landscape of healthcare with confidence, creativity, and a profound sense of purpose. By transforming challenges into opportunities, they advance both individual and organizational excellence while delivering meaningful impact on the patients and communities they serve.
Conclusion
The journey to conquering the NAPLEX is both challenging and transformative, blending deep knowledge, critical thinking, and patient-centered decision-making. Success requires more than memorizing facts; it demands mastery of pharmacology, precision in calculations, and the ability to synthesize clinical information into safe and effective patient care. Effective preparation combines structured study strategies, active engagement with practice scenarios, and thoughtful stress management to ensure readiness under the pressures of the exam.
Beyond the test itself, the NAPLEX serves as a gateway to professional growth and lifelong learning. Passing the exam validates not only technical competence but also the judgment, ethics, and communication skills essential to modern pharmacy practice. Pharmacists who embrace continuous learning, reflect on their experiences, and remain curious and adaptable are best positioned to provide high-quality care and make meaningful contributions to the healthcare system.
Ultimately, the NAPLEX is more than an exam; it is a milestone that marks the transition from student to professional, laying the foundation for a career defined by expertise, responsibility, and dedication to patient well-being. Success comes from preparation, perseverance, and a commitment to excellence, ensuring that every pharmacist stepping into practice is equipped to make a real difference in the lives of those they serve.
Frequently Asked Questions
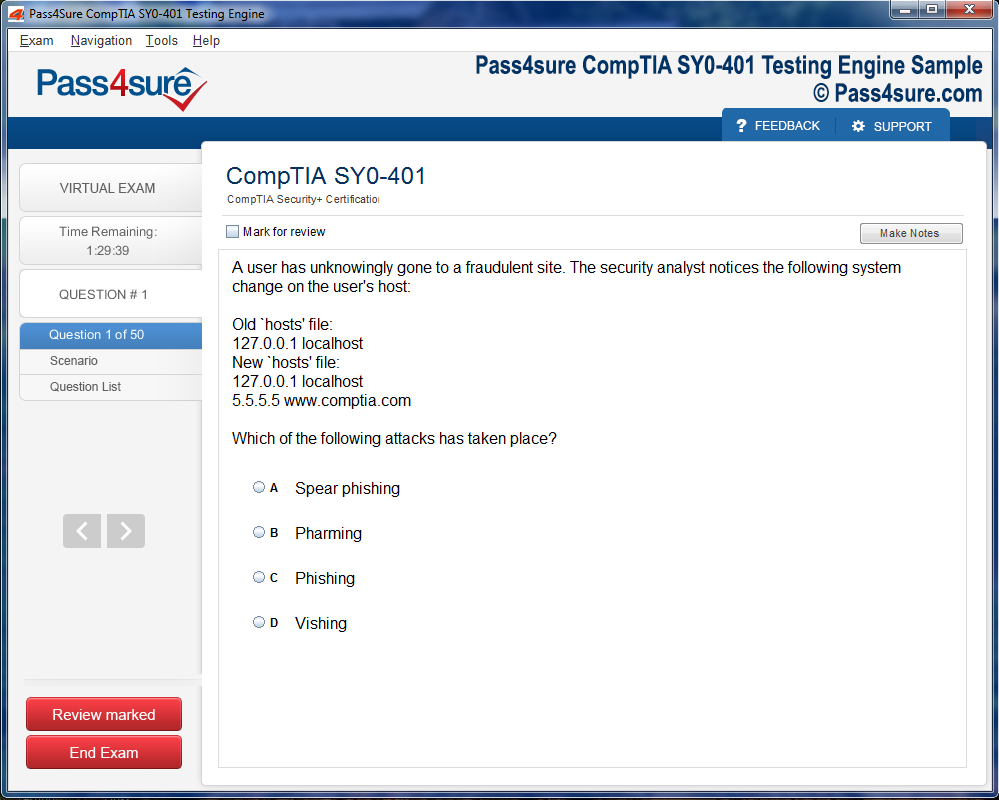
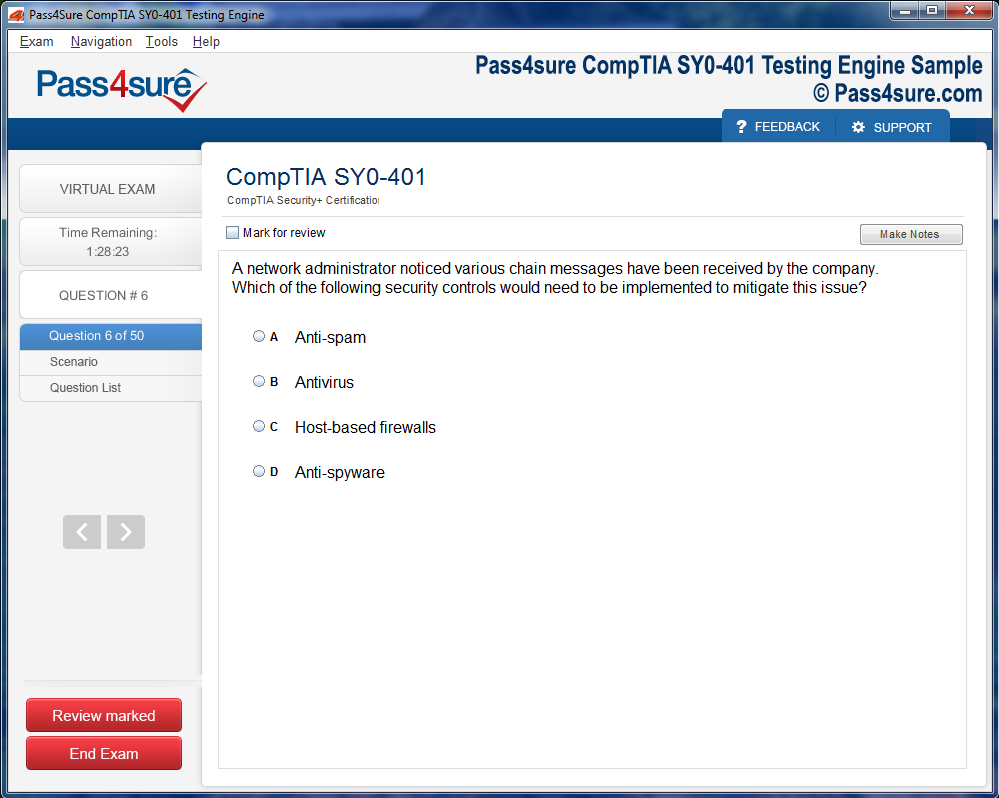
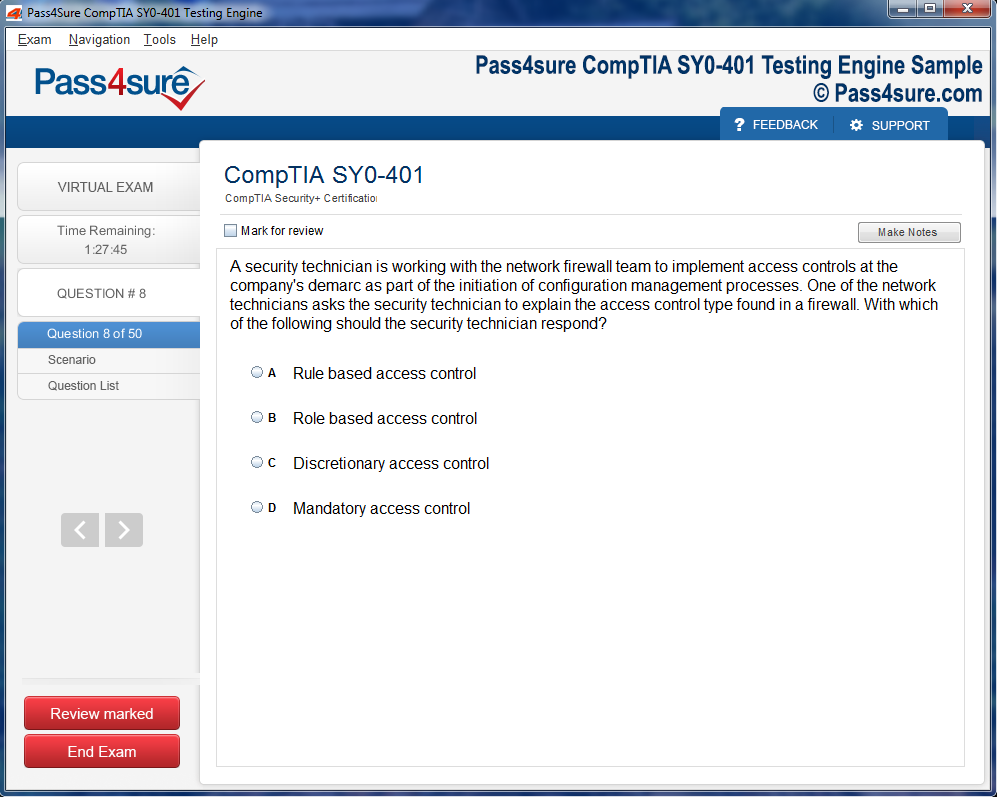
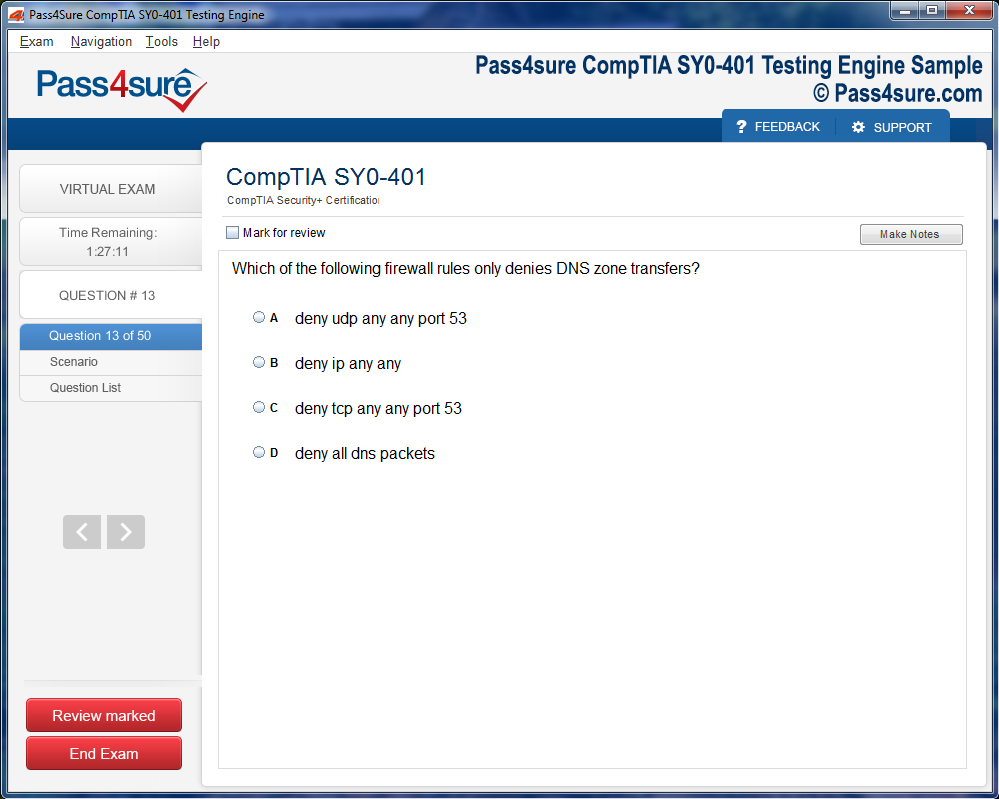
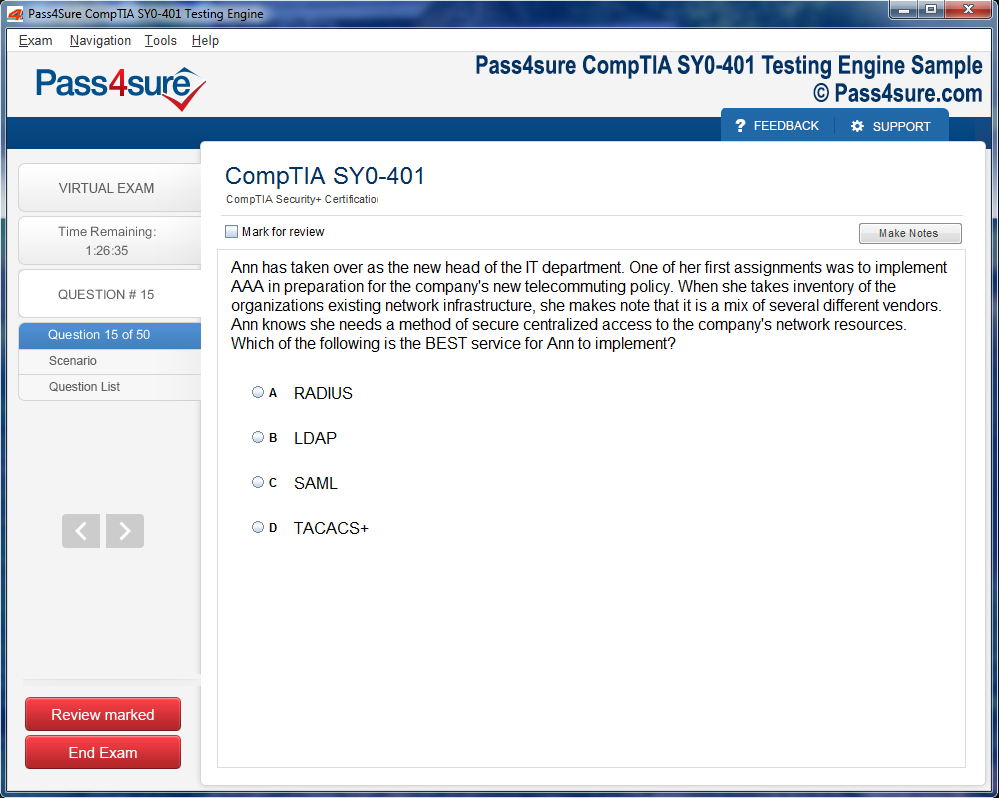
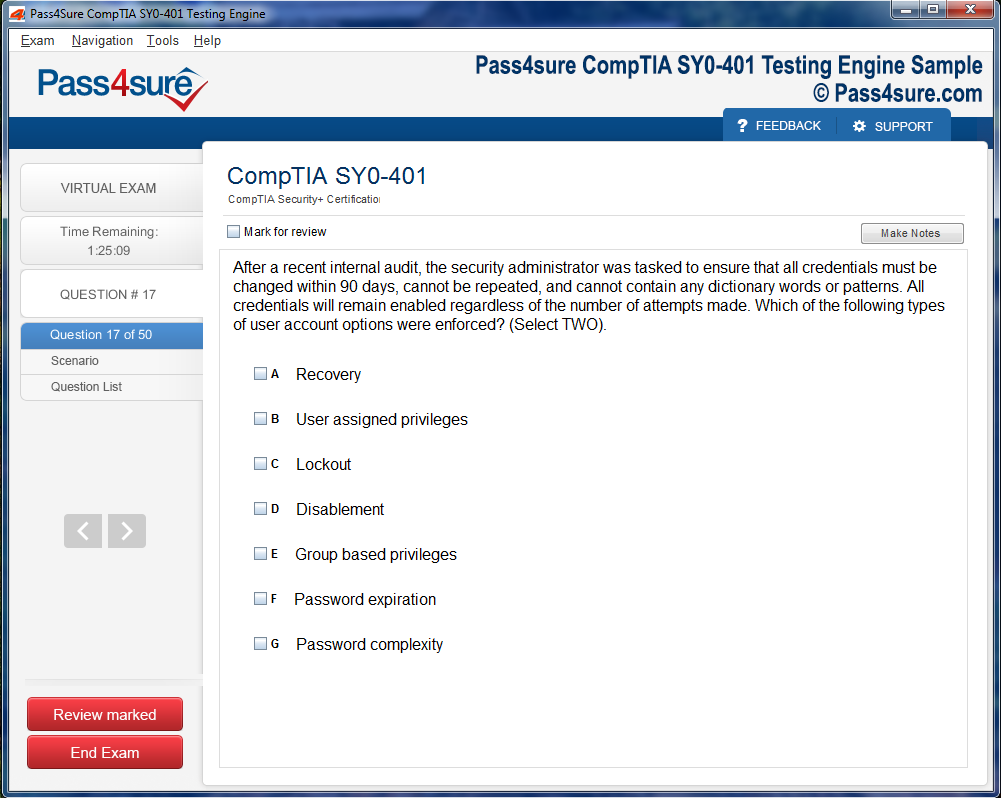
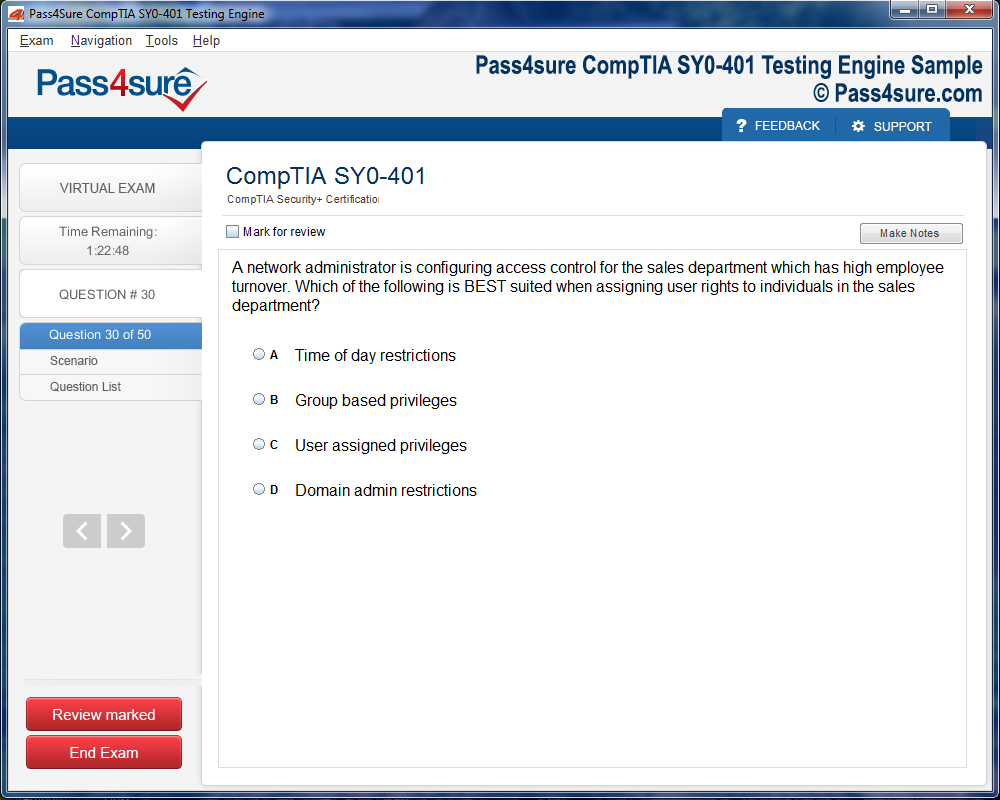
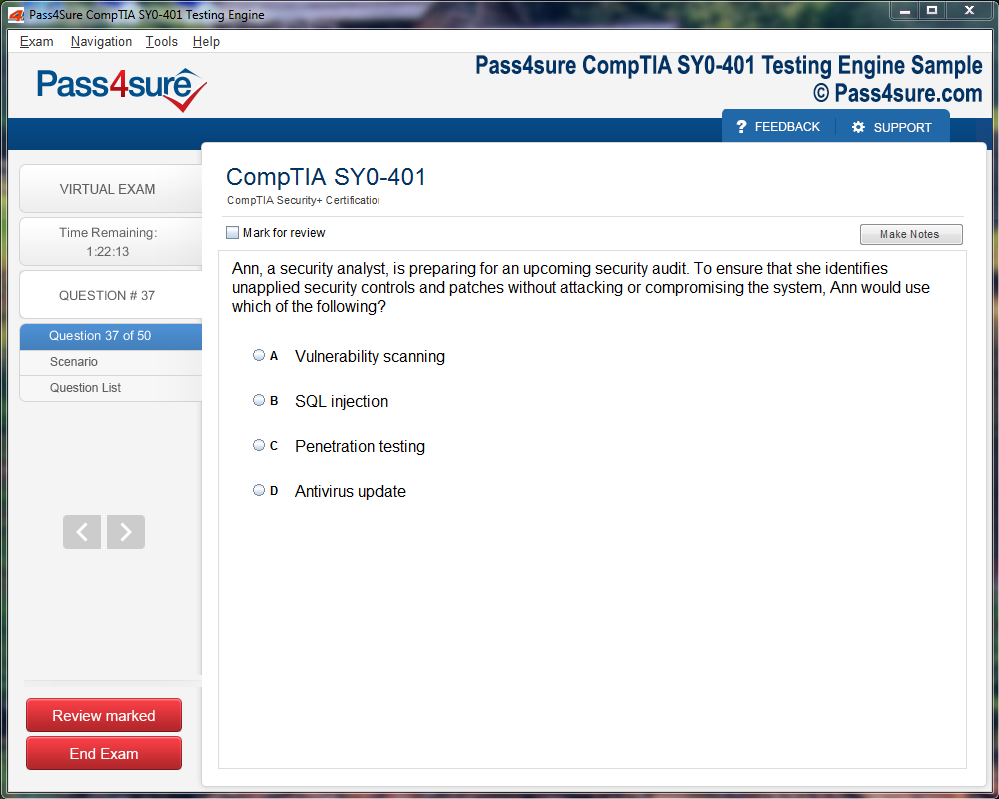
How does your testing engine works?
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations).
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.