Test Name: MCQS - Multiple-choice questions for general practitioner (GP) Doctor
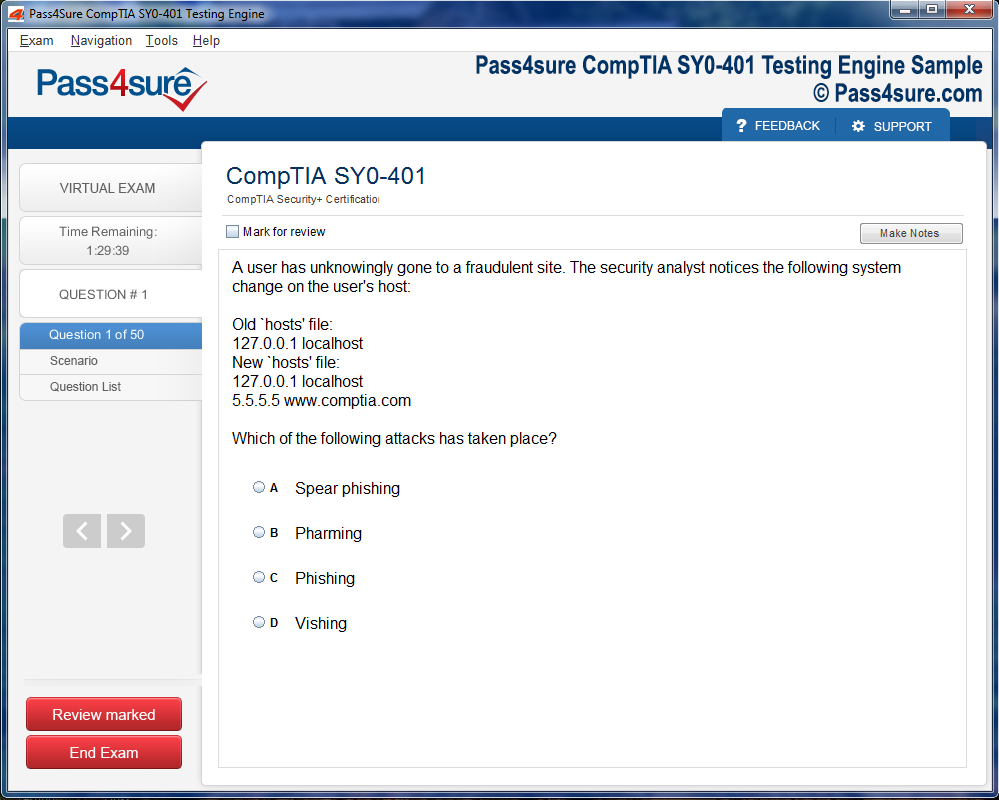
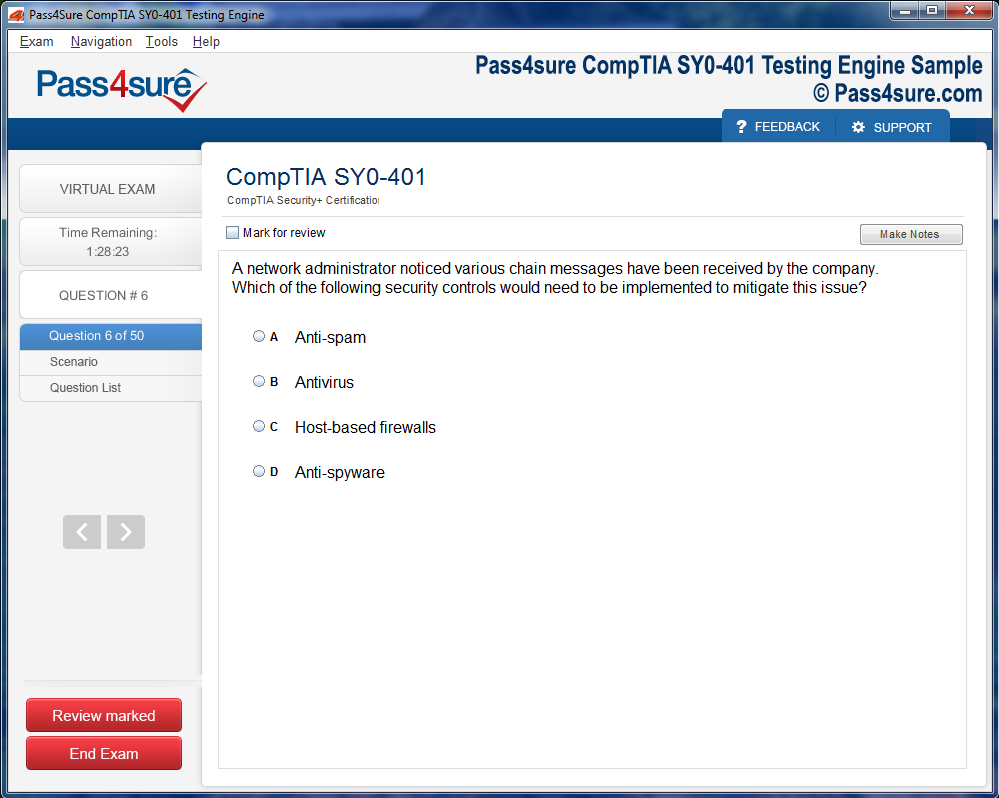
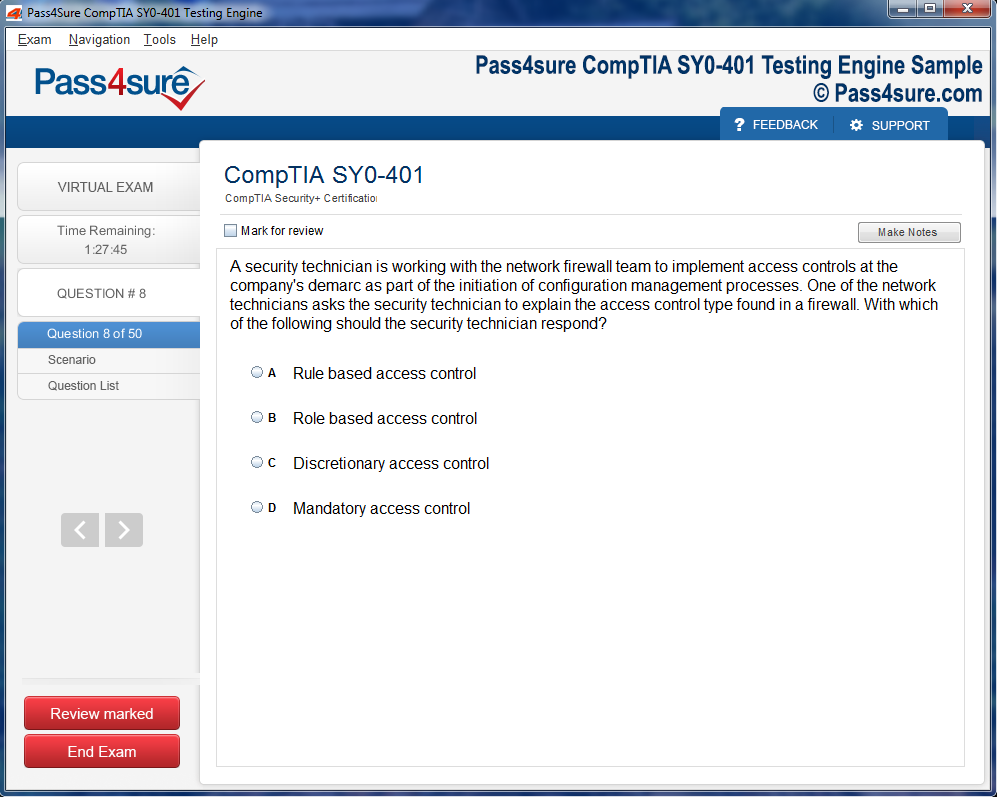
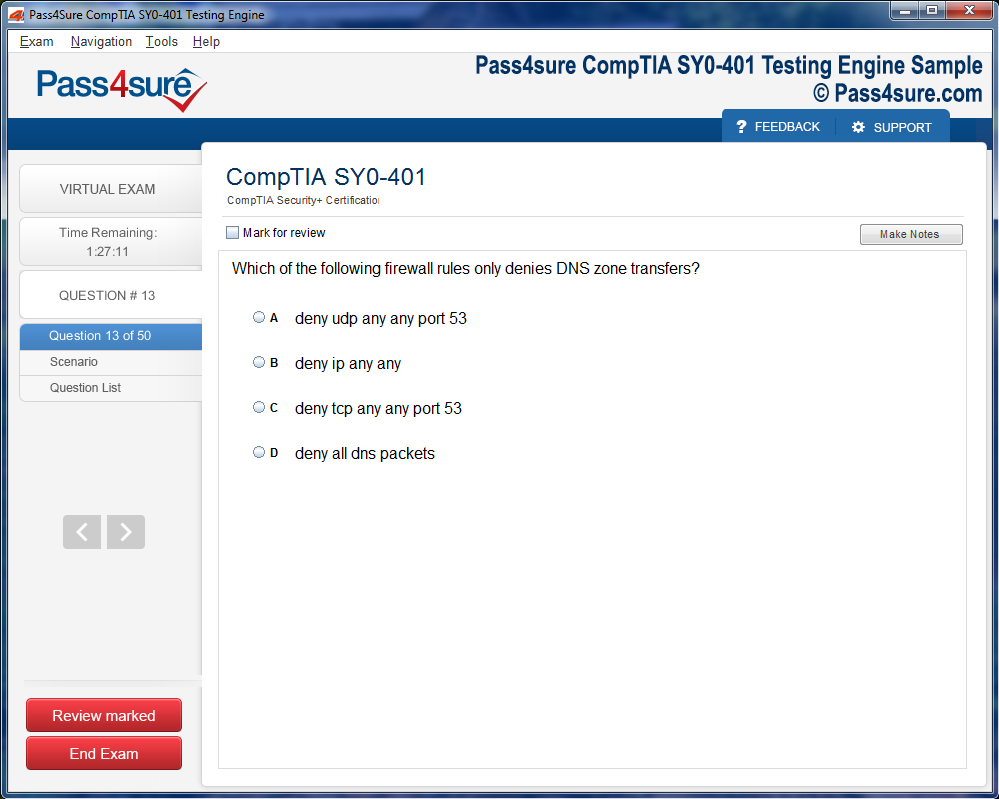
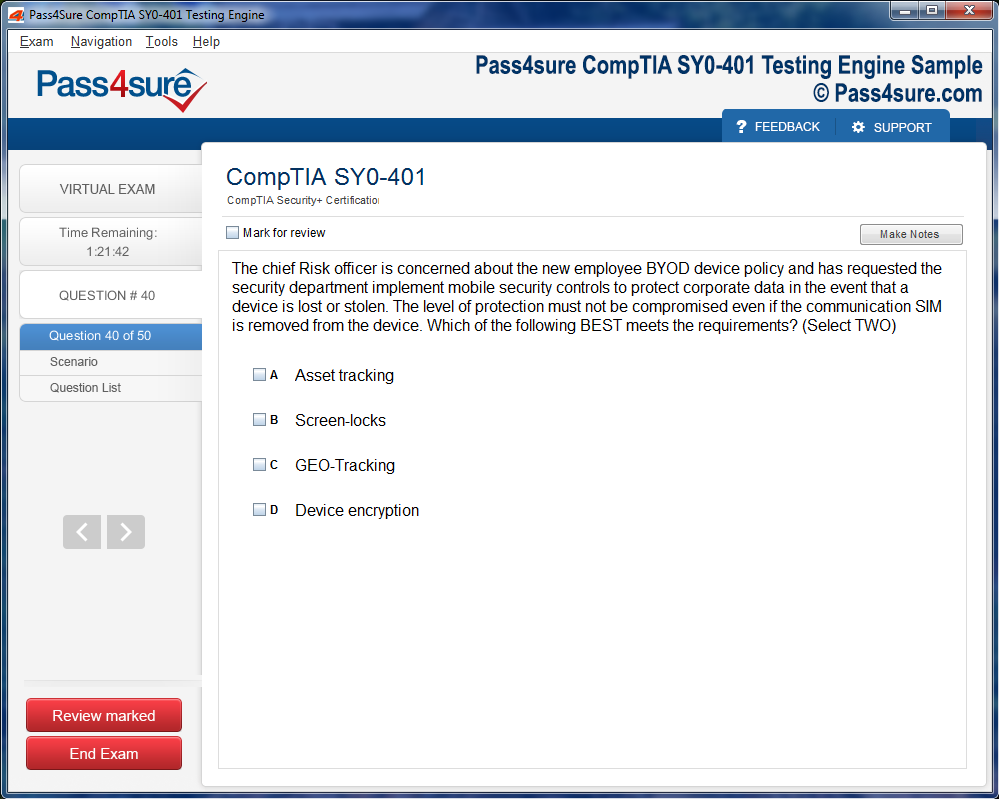
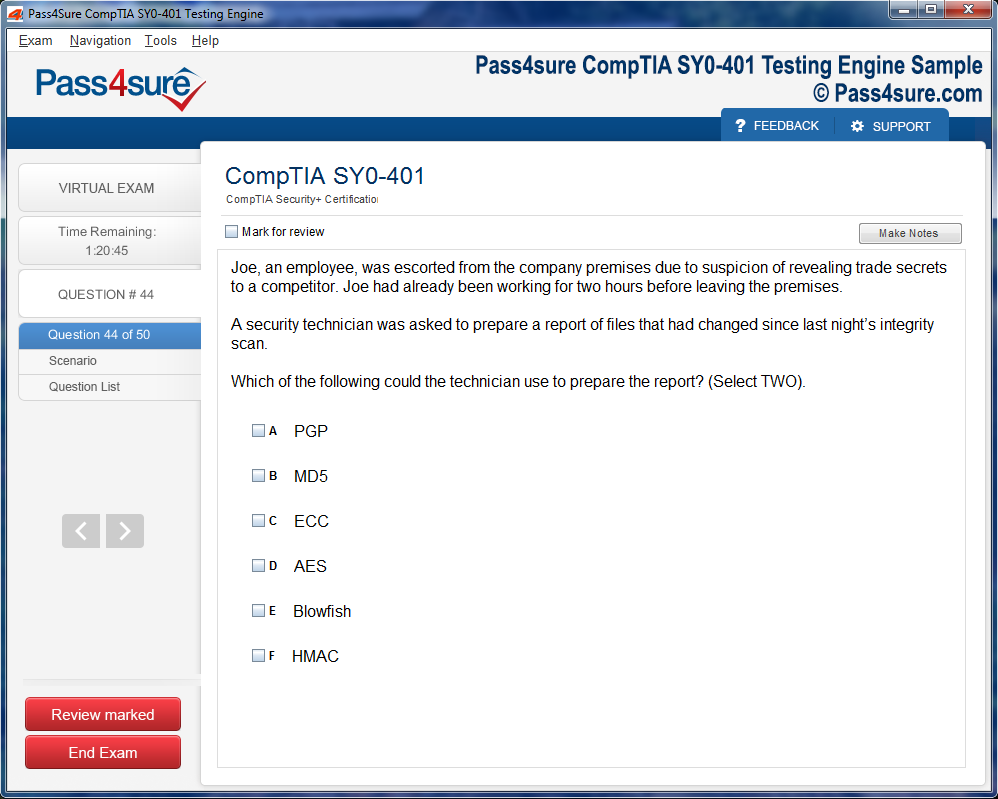
Product Screenshots
Mastering Medicine: MCQs for Aspiring and Practicing GPs
The cornerstone of general practice lies in the artful extraction of a patient’s narrative. Beyond the superficial chronology of symptoms, the practitioner must attune to the subtleties embedded within speech patterns, emotional undertones, and behavioral cues. A seemingly trivial remark can serve as a keystone, revealing the presence of systemic stressors or early-stage disease processes. The clinician’s task is to create a space of trust where the patient feels both heard and understood, allowing the narrative to unfold with authenticity.
Effective history-taking is a delicate dance between structured inquiry and adaptive improvisation. While checklists and protocols ensure coverage of essential information, they must be interwoven with flexibility, allowing the clinician to follow the patient’s lead when unexpected yet significant details emerge. The attentive observer notices slight variations in phrasing, hesitation, or incongruence between verbal reports and non-verbal signals. These insights frequently inform the direction of the physical examination, guide the choice of investigative modalities, and refine the differential diagnosis.
Moreover, the integration of social determinants of health into patient assessment is indispensable. Economic constraints, educational background, living conditions, and familial structures all exert profound influence over disease manifestation and adherence to treatment. Recognizing these factors requires curiosity and cultural sensitivity, ensuring that recommendations are practical, respectful, and contextually appropriate. A history taken in this comprehensive manner forms the scaffold upon which safe, individualized care can be constructed.
Physical Examination as an Interpretive Art
While technology continues to transform medicine, the physical examination retains an irreplaceable role in clinical discernment. It is not merely a procedural ritual but a sensory exploration that complements the patient narrative. Skilled clinicians observe with both eyes and intuition, noting subtleties in skin tone, gait, posture, and involuntary movements that may escape cursory inspection. Palpation, auscultation, and percussion are performed not as rote maneuvers but as investigative tools that reveal the invisible currents of pathophysiology beneath the surface.
The interpretive quality of the physical examination depends heavily on accumulated experience. Patterns recognized over years of practice allow the clinician to anticipate complications, differentiate between similar presentations, and detect early warning signs. Each encounter serves as an opportunity to refine this interpretive skill, enhancing the clinician’s ability to perceive nuances that may otherwise remain concealed. The act of examining a patient thus becomes a conversation between touch, observation, and clinical reasoning—a dialogue in which subtleties speak volumes about the underlying disease process.
Simultaneously, the physical examination offers a unique opportunity to reinforce the therapeutic alliance. Demonstrating care through deliberate, respectful, and patient-centered examination fosters confidence and mitigates anxiety. It transforms a purely diagnostic procedure into an experiential reassurance, highlighting the dual role of the GP as both diagnostician and healer.
Cognitive Precision and the Avoidance of Diagnostic Pitfalls
Clinical acumen is inseparable from the careful navigation of cognitive biases. Anchoring, premature closure, confirmation bias, and availability heuristic can subtly distort judgment, leading even seasoned clinicians astray. Awareness of these mental pitfalls is the first defense against error, enabling the GP to approach each case with deliberate caution and critical scrutiny.
A methodical approach to differential diagnosis is therefore essential. Initial impressions must be interrogated, and alternative explanations explored with equal rigor. The clinician must remain vigilant for atypical presentations, recognizing that common diseases often masquerade in uncommon ways while rare conditions occasionally reveal themselves through subtle, easily overlooked signs. Diagnostic tools—laboratory tests, imaging studies, and functional assessments—must be employed strategically, serving to confirm or exclude hypotheses rather than supplant careful clinical reasoning.
Repetition and reflective practice are vital in cultivating cognitive precision. By reviewing outcomes, analyzing near misses, and engaging in peer discussions, clinicians enhance their ability to anticipate pitfalls, recognize subtle cues, and make judicious decisions under uncertainty. This reflective discipline transforms episodic knowledge into durable insight, ensuring that each encounter contributes to a cumulative and resilient clinical intuition.
Therapeutic Planning and Individualized Care
Once diagnostic clarity is achieved, the challenge shifts to designing therapeutic strategies that are both evidence-informed and individually tailored. Effective management in general practice transcends generic protocols, requiring nuanced adjustment to the patient’s lifestyle, comorbidities, preferences, and psychosocial context. Treatment is therefore a collaborative endeavor in which the GP negotiates objectives, explains rationale, and cultivates shared responsibility for outcomes.
Pharmacologic interventions are only one element of this broader tapestry. Behavioral modifications, nutritional guidance, physical rehabilitation, and psychosocial support frequently carry equal or greater weight in promoting long-term health. The GP must possess the discernment to prioritize interventions, sequence them logically, and anticipate barriers to adherence. By aligning treatment plans with the patient’s lived reality, the practitioner transforms medical directives into achievable, sustainable actions that empower rather than overwhelm.
Furthermore, longitudinal care emphasizes continuity and adaptation. Conditions evolve, patient circumstances shift, and responses to therapy vary. Effective GPs monitor progress vigilantly, recalibrating strategies based on emerging evidence, patient feedback, and subtle physiological cues. This iterative process underscores the dynamic nature of general practice, in which flexibility, foresight, and attentive follow-up define excellence.
Emotional Intelligence and the Therapeutic Relationship
The physician-patient relationship is both a conduit for clinical information and a medium of psychological support. Emotional intelligence—the ability to recognize, interpret, and respond to emotional states—enhances diagnostic accuracy, facilitates adherence, and mitigates conflict. By attuning to a patient’s affect, the GP can identify distress, fear, or ambivalence that may otherwise obscure the clinical picture.
Empathy, as a component of emotional intelligence, is cultivated through deliberate attention and self-reflection. It entails not only understanding the patient’s perspective but also communicating that understanding authentically. Patients who perceive genuine concern are more likely to disclose sensitive information, comply with recommendations, and maintain engagement in their care. The therapeutic relationship thus functions as both diagnostic amplifier and healing medium, amplifying the efficacy of clinical interventions through trust and relational depth.
Equally, the GP must manage their own emotional responses. Compassion fatigue, vicarious trauma, and ethical dilemmas are inherent in clinical practice. Developing resilience through reflective practice, professional supervision, and self-care strategies ensures that emotional engagement enhances rather than diminishes effectiveness. The clinician who balances empathy with self-regulation achieves both professional sustainability and higher quality patient care.
Integrating Technology and Evidence-Based Practice
The modern GP operates within a rapidly evolving technological landscape. Diagnostic imaging, point-of-care testing, telemedicine, and digital health platforms expand the capacity for precise, timely intervention. Yet technology must be integrated judiciously, guided by clinical acumen rather than novelty. The discerning practitioner evaluates the relevance, limitations, and potential harms of technological interventions, ensuring that patient welfare remains paramount.
Evidence-based medicine underpins this technological integration. Critical appraisal of literature, synthesis of guidelines, and judicious application of research findings enable clinicians to balance innovation with prudence. Each new advance is assessed not only for statistical significance but for practical relevance to individual patients. By cultivating both scientific literacy and technological fluency, the GP bridges the worlds of research and daily practice, translating complex knowledge into actionable, patient-centered care.
The interplay between technology, evidence, and clinical intuition exemplifies the modern evolution of general practice. It requires adaptability, discernment, and an unwavering focus on the human element of medicine, ensuring that patients benefit from progress without losing the personal touch that defines high-quality care.
Professionalism, Ethics, and the Stewardship of Care
Professionalism in general practice extends beyond competence to encompass accountability, integrity, and ethical stewardship. Decisions are frequently made under uncertainty, balancing potential benefits, risks, and resource considerations. Ethical deliberation guides choices that may profoundly affect patients’ lives, requiring both moral clarity and humility.
Stewardship also involves advocacy for patient welfare, resource-conscious decision-making, and commitment to equitable care. The GP acts not only as a clinician but as a custodian of public health, recognizing the broader implications of individual decisions. Upholding confidentiality, obtaining informed consent, and practicing with transparency reinforce trust, which is foundational to sustainable, high-impact practice.
Resilience, reflective practice, and ongoing professional development sustain this ethical commitment. By engaging continuously with evolving knowledge, emerging societal expectations, and personal growth, the clinician ensures that ethical principles are not static abstractions but living guides that shape every interaction and intervention.
The Foundations of General Practice
General practice occupies a unique realm in medicine, demanding a synthesis of knowledge, observation, and human understanding. Unlike narrowly defined specialties, general practitioners encounter a spectrum of ailments that defy singular categorization. Each patient presents not merely as a set of symptoms, but as a living narrative woven from physical, emotional, and social threads. Establishing a foundation in this field requires an appreciation of its breadth, where mastery depends as much on cognitive flexibility as on factual expertise. The GP must navigate an intricate landscape where common conditions intermingle with rare presentations, and where subtle cues often hold greater significance than overt signs.
The clinical environment itself shapes the approach. Consultations occur under varied circumstances: hurried mornings, complex chronic management, or emotionally charged discussions. Each scenario tests the practitioner’s capacity for attention, patience, and empathy. Building resilience in this context involves cultivating a mental framework that accommodates ambiguity and uncertainty, allowing for measured yet decisive actions. The ability to remain composed under pressure becomes a cornerstone of effective practice, reinforcing the integration of knowledge, intuition, and situational awareness.
Observation and Subtlety in Patient Assessment
Observation constitutes the silent language of clinical insight. The careful GP discerns meaning in nuances that might escape the untrained eye. A slight tremor, a fleeting pallor, or the cadence of a patient’s speech can suggest underlying pathology long before formal investigations reveal it. These observations are not incidental; they are deliberate acts of attentiveness that require consistent practice. Developing this skill entails learning to parse signals from noise, distinguishing fleeting idiosyncrasies from significant indicators.
Subtlety in assessment extends beyond the visual domain. Auditory cues, tactile impressions, and even olfactory signals may provide insight into a patient’s condition. Recognizing patterns across multiple senses strengthens diagnostic confidence and allows early detection of deviations from health. Over time, the GP internalizes a repertoire of micro-indicators, enabling a near-instinctive grasp of complexity. This mastery does not emerge from passive exposure; it demands reflection, repeated encounters, and a commitment to continuous observation.
Narrative Medicine and Effective History-Taking
History-taking transcends a mere catalog of complaints. It is an art of narrative reconstruction, where the GP pieces together fragments of lived experience into coherent diagnostic possibilities. Patients communicate through a lens shaped by emotion, memory, and cultural context, often obscuring critical information. Attentive listening allows the practitioner to sift through this complexity, identifying patterns, contradictions, and subtle hints that point to underlying disease processes.
This narrative approach requires patience and an openness to diverse forms of communication. The GP must tolerate pauses, silences, and deviations from linear storytelling, recognizing that these elements often carry meaning. Contextual understanding enhances interpretation, allowing the clinician to appreciate how lifestyle, environment, and personal values intersect with physical health. History-taking thus becomes an exercise in empathy and analytical rigor, linking the patient’s lived reality to plausible medical explanations.
Physical Examination as a Diagnostic Language
Physical examination is the vocabulary through which the body communicates its internal state. Each palpation, auscultation, and inspection represents a sentence in the unfolding story of health and disease. Skillful interpretation requires not only technical proficiency but also familiarity with normative variations. Recognizing the boundary between normality and pathology is subtle work, demanding attentive comparison and experience-driven intuition.
The sequential and integrative nature of examination allows the GP to construct a multi-dimensional understanding of the patient’s physiology. Observations in one system often inform interpretations in another, highlighting interconnections and revealing hidden patterns. This synthesis exemplifies the holistic approach of general practice, where findings are not isolated data points but components of a dynamic network. The GP who integrates empirical observation with reflective insight develops a nuanced diagnostic lens capable of early detection and anticipatory guidance.
Differential Diagnosis and Cognitive Agility
Differential diagnosis represents the crucible where knowledge, reasoning, and clinical intuition converge. Generating a differential list involves more than enumerating possible conditions; it requires prioritization based on likelihood, severity, and the immediacy of risk. A flexible mindset permits the practitioner to reassess hypotheses as new information emerges, avoiding premature closure and cognitive rigidity.
Cognitive agility is essential in navigating this process. It allows the GP to pivot seamlessly, recalibrate probabilities, and incorporate emerging evidence without losing sight of the patient’s broader context. While evidence-based guidelines provide a scaffold for decision-making, they are most effective when integrated with situational judgment. The dynamic interplay between structured knowledge and adaptive reasoning ensures that the clinician’s approach remains precise, patient-centered, and resilient to uncertainty.
Laboratory and Imaging Interpretation
Laboratory tests and imaging serve as extensions of clinical acumen, offering objective data that can corroborate or challenge initial impressions. However, the judicious application of these modalities is crucial. Overreliance can dilute observational skills and impose unnecessary burdens on patients. Strategic ordering, guided by thoughtful history and examination, maximizes diagnostic value while minimizing risk.
Interpreting results demands more than rote memorization of reference ranges. Sensitivity, specificity, and predictive value must be contextualized within the individual patient’s presentation. Recognizing false positives, incidental findings, and the limitations of technology sharpens clinical judgment. The practitioner who balances empirical evidence with holistic insight navigates the delicate interface between quantifiable data and the artful understanding of human health.
Systems Thinking and Anticipatory Care
General practice thrives on systems thinking, where the patient is viewed as a network of interdependent processes rather than isolated organs. Chronic conditions frequently interact, influencing the trajectory of acute episodes and shaping responses to treatment. Anticipating these interactions requires foresight, an understanding of pathophysiological mechanisms, and a keen sense of timing.
Longitudinal care exemplifies this principle, demanding continuity, monitoring, and proactive adjustment. The GP who anticipates complications, understands comorbidity, and visualizes the cascade of interventions enhances patient safety and overall outcomes. This forward-looking perspective transforms reactive medicine into proactive stewardship, fostering resilience, prevention, and the sustained promotion of health.
Communication and Shared Decision-Making
Communication remains central to effective practice, transforming technical expertise into shared understanding. Explaining rationale, discussing uncertainties, and inviting patient participation cultivates trust and adherence. The relational dimension of medicine is inseparable from its diagnostic and therapeutic components. Without clear communication, even the most precise clinical reasoning risks ineffectiveness.
The GP who practices transparent, empathetic dialogue empowers patients to engage actively with their care. This collaborative approach aligns therapeutic goals with patient values, enhancing satisfaction, and reinforcing the clinician-patient bond. Communication is thus both a clinical tool and an ethical imperative, bridging the gap between knowledge and lived experience.
Continuous Learning and Reflective Practice
The landscape of medicine is ever-evolving, demanding a commitment to lifelong learning. Advances in understanding disease mechanisms, novel therapies, and shifting epidemiology necessitate that the GP maintains intellectual agility. Reflective practice complements ongoing education, allowing the clinician to analyze past decisions, integrate feedback, and refine judgment.
Curiosity fuels this process, encouraging exploration beyond immediate practice needs. Critical appraisal of emerging evidence, engagement with peers, and self-directed study cultivate resilience against obsolescence. The GP who embraces reflective learning develops a mental architecture that supports adaptive reasoning, anticipates challenges, and maintains a high standard of care in a constantly shifting environment.
Mastery Through Experience and Mentorship
Experience serves as the crucible for integrating knowledge with practice. Repeated patient encounters, exposure to rare conditions, and iterative reflection deepen understanding and sharpen intuition. Mentorship amplifies this process, providing guidance, feedback, and modeling professional behavior. The interplay between direct experience and informed supervision accelerates skill acquisition, embedding clinical acumen within the practitioner’s cognitive framework.
Through sustained engagement, the GP internalizes patterns, hones observational sensitivity, and refines judgment. Errors, when approached constructively, become powerful learning tools, enhancing resilience and fostering humility. Mastery emerges as a composite of knowledge, intuition, reflection, and relational competence, equipping the clinician to navigate complexity with confidence and precision.
Ethical Awareness and Moral Responsibility
Ethics permeates every dimension of general practice. Decisions carry profound implications for patient welfare, autonomy, and trust. The GP must navigate tensions between beneficence, nonmaleficence, and respect for individual values. Ethical awareness is not a static checklist but a dynamic process of reflection, balancing competing priorities, and anticipating consequences.
Moral responsibility extends beyond immediate clinical outcomes. The practitioner considers the broader societal context, resource stewardship, and implications for public health. Integrating ethical deliberation with clinical reasoning ensures that care is not only technically sound but morally coherent. This fusion of intellect and conscience exemplifies the holistic ethos of general practice.
The Essence of Preventive Strategies in General Practice
Preventive strategies form the cornerstone of general practice, reflecting a philosophy that prioritizes foresight over reaction. General practitioners who excel in preventive care embrace an anticipatory mindset, seeking to identify risk factors before they escalate into full-blown disease. This approach demands a sophisticated understanding of epidemiology, population health trends, and the subtleties of individual vulnerability. Each consultation becomes an opportunity to weave preventive guidance into everyday life, whether through vaccinations, screenings, or lifestyle adjustments. Preventive interventions are most effective when they resonate with the patient’s lived experience, requiring practitioners to tailor their advice to social, cultural, and psychological realities. Through careful observation and thoughtful questioning, GPs can detect early warning signs, subtle deviations from normal physiology, and nascent behavioral patterns that may predispose individuals to chronic conditions. The artistry of prevention lies not merely in identifying risks but in translating that awareness into practical, achievable action plans that patients can internalize and sustain.
The implementation of preventive strategies also demands adaptability and persistence. Health education, for instance, must evolve with the patient’s understanding and readiness to change. Repetition, reinforcement, and reinforcement through positive feedback often consolidate beneficial behaviors. Moreover, preventive care extends beyond the individual, encompassing family and community dynamics. Encouraging healthy habits in a broader context can amplify the impact of interventions, fostering environments that support well-being. A GP’s ability to balance individual guidance with population-level awareness exemplifies a sophisticated form of clinical acumen that transforms reactive medicine into proactive health stewardship.
Navigating Chronic Illness with Precision and Compassion
Chronic illness management represents a delicate interplay of clinical knowledge, empathy, and long-term engagement. General practitioners function as both diagnosticians and guides, steering patients through prolonged trajectories of care. Conditions such as diabetes, hypertension, chronic obstructive pulmonary disease, and cardiovascular disorders demand consistent monitoring and iterative adjustments. A nuanced approach recognizes that adherence is influenced by more than understanding—it is shaped by motivation, social support, emotional resilience, and the subtle fluctuations of daily life. GPs must balance protocol-driven interventions with individualized adaptations, ensuring that therapeutic plans remain flexible enough to accommodate lifestyle changes, comorbidities, and patient preferences. The long-term nature of chronic disease management often unveils the relational dimension of practice, as trust, rapport, and ongoing communication directly influence clinical outcomes.
Beyond medication adherence, lifestyle counseling constitutes a central pillar of chronic illness management. Structured guidance on nutrition, exercise, sleep hygiene, and stress reduction can profoundly affect disease trajectory. The practitioner’s role is to integrate these non-pharmacological strategies seamlessly with medical treatment, fostering patient agency while ensuring safety. Continuous assessment, reflective observation, and empathetic engagement enable the GP to recognize barriers, celebrate incremental progress, and recalibrate plans as necessary. In this context, mastery is measured not only by clinical outcomes but by the ability to maintain patient motivation and confidence across months and years of complex care.
Precision in Pharmacological Stewardship
Pharmacological stewardship is the bedrock of therapeutic mastery, demanding meticulous attention to detail, anticipation of interactions, and dynamic responsiveness. Effective medication management encompasses the intricate balance of efficacy, safety, adherence potential, and cost-effectiveness. In primary care, polypharmacy is common, particularly among aging populations with multiple comorbidities. Here, the clinician’s skill is revealed in their ability to streamline regimens, mitigate adverse interactions, and optimize dosing schedules to align with patient routines. The smallest alteration—a change in timing, formulation, or combination—can yield meaningful improvements or prevent serious complications. This attention to nuance distinguishes proficient practitioners from average ones, transforming pharmacology into an instrument of precision rather than a mere checklist of prescriptions.
Pharmacological stewardship also requires ongoing vigilance. Laboratory monitoring, periodic review of therapeutic response, and anticipatory adjustment are essential to maintaining efficacy while preventing harm. Equally important is patient education, as understanding the rationale, potential side effects, and expected outcomes of medications fosters adherence and empowers self-management. A GP’s ability to translate complex pharmacological principles into clear, actionable guidance exemplifies the intersection of technical mastery and effective communication, reinforcing the centrality of the patient-practitioner partnership in sustaining therapeutic success.
Integrating Behavioral and Lifestyle Interventions
Behavioral and lifestyle interventions occupy a crucial role in patient-centered care, offering pathways to wellness that extend beyond traditional medical treatment. Nutritional optimization, structured physical activity, stress reduction, and sleep regulation are among the pillars that support holistic health. These interventions demand careful personalization, as each patient’s context, preferences, and cultural framework shape the feasibility and sustainability of change. The GP must employ motivational strategies, practical guidance, and empathetic encouragement, translating general recommendations into specific, attainable actions. In this way, lifestyle intervention becomes an exercise in creativity and patience, requiring continuous dialogue, feedback, and reinforcement.
The subtle power of behavioral interventions lies in their capacity to produce lasting physiological and psychological benefits. Chronic stress, sedentary habits, and poor dietary choices often underpin disease progression, and yet they are amenable to structured, consistent modification. The practitioner’s role is to scaffold patient agency, supporting incremental progress while anticipating setbacks. Success is rarely instantaneous; it is measured by sustained engagement, enhanced self-efficacy, and the slow accrual of measurable health improvements. Mastery in this domain reflects not only knowledge but the ability to inspire, adapt, and cultivate enduring change.
Holistic Monitoring and Adaptive Care Planning
Monitoring patient progress extends far beyond the documentation of objective measurements. It is an art of observation, interpretation, and anticipatory adjustment. Regular follow-up allows the GP to evaluate therapeutic efficacy, detect adverse reactions early, and recalibrate interventions to reflect evolving needs. Clinical signs, laboratory results, and patient-reported experiences converge to create a nuanced picture of health status. The practitioner must synthesize this information into actionable insight, discerning patterns, deviations, and emerging risks with both analytical precision and intuitive sensitivity. Adaptive care planning ensures that interventions remain aligned with patient goals, lifestyle realities, and evolving evidence, reinforcing the dynamic nature of general practice.
This continuous monitoring also underpins the relational dimension of care. Ongoing engagement fosters trust, reinforces accountability, and enhances adherence. Patients are more likely to sustain beneficial behaviors when they perceive that their practitioner is attuned, responsive, and genuinely invested in their well-being. By integrating technical assessment with empathetic observation, the GP transforms routine follow-ups into rich opportunities for personalized intervention, reinforcing the longitudinal depth that defines high-quality primary care.
Fostering Patient Engagement and Shared Decision-Making
Patient engagement represents the fulcrum upon which effective care pivots. General practitioners cultivate shared decision-making by actively listening, validating concerns, and aligning clinical recommendations with the patient’s values and priorities. Every interaction becomes a negotiation between expertise and autonomy, with success measured by adherence, satisfaction, and meaningful outcomes. Cultivating engagement requires clear communication, cultural sensitivity, and an ability to frame complex medical information in accessible, relatable terms. When patients feel empowered to participate in decisions, they are more likely to embrace treatment plans, maintain consistent follow-up, and achieve sustainable lifestyle modifications.
The relational aspect of patient engagement is reinforced by empathy, transparency, and consistency. Trust is built through attentive listening, reassurance, and respect for patient perspectives. Even subtle gestures—acknowledging concerns, celebrating progress, and addressing anxieties—can significantly strengthen therapeutic alliances. By fostering this depth of engagement, the GP transforms care from a transactional process into a collaborative journey, ensuring that clinical expertise is amplified by patient agency and commitment.
Continuous Professional Evolution and Reflective Practice
The pursuit of therapeutic mastery is incomplete without ongoing professional evolution. Medicine is dynamic, and new research, guidelines, and technological innovations continuously reshape clinical paradigms. Reflective practice enables general practitioners to critically appraise their own decisions, identify areas for improvement, and integrate emerging evidence into patient care. Case review, peer discussion, and participation in professional development activities cultivate both technical expertise and adaptive thinking. Reflection also reinforces ethical judgment, ensuring that interventions remain patient-centered, evidence-based, and contextually sensitive.
Professional growth extends beyond acquiring knowledge; it encompasses cultivating resilience, humility, and curiosity. Practitioners who embrace reflective practice are better equipped to navigate uncertainty, manage complexity, and respond to evolving patient needs with insight and creativity. By integrating technical skill with adaptive reasoning and humanistic understanding, general practitioners achieve a level of competence that transforms routine practice into a dynamic, responsive, and deeply impactful vocation.
The Subtle Art of Communication and Patient Engagement
Effective communication in general practice transcends mere words. It shapes the very fabric of the therapeutic relationship, influencing diagnostic precision, treatment adherence, and patient satisfaction. Each patient encounter unfolds as an intricate dance, where verbal expressions, gestures, and silences intertwine to reveal both the apparent symptoms and the hidden narratives of human experience. The physician’s skill lies not only in technical knowledge but in the capacity to interpret, empathize, and respond thoughtfully. This nuanced interplay defines the subtle art of communication, an essential cornerstone of patient engagement.
The first moments of a consultation often determine the trajectory of the encounter. A physician’s demeanor, posture, and attentiveness send signals as potent as spoken words. Patients convey crucial information through hesitation, facial expressions, and bodily cues, often before articulating concerns explicitly. Attentive observation, combined with active listening, allows the physician to decode these subtleties. Pauses, reflective statements, and gentle prompts invite patients to share deeper layers of their experience. This approach transforms the clinical interaction into a collaborative dialogue, where trust and understanding flourish alongside diagnostic insight.
Equally vital is the ability to translate complex medical concepts into language that patients can grasp. Health literacy varies widely, and the physician’s role includes bridging the gap between scientific precision and accessible explanation. Analogies, narrative illustrations, and stepwise explanations empower patients to comprehend their condition, the rationale for treatment, and the anticipated outcomes. Clear communication not only fosters understanding but nurtures confidence, encouraging patients to participate actively in decision-making. Miscommunication, by contrast, can generate anxiety, erode trust, and compromise adherence to therapy. Precision in language, combined with empathy, forms the backbone of meaningful engagement.
Handling sensitive topics demands heightened skill and emotional awareness. Conversations about mental health, sexual health, chronic illness, or terminal conditions require tact, honesty, and compassion. Patients often carry fear, stigma, or guilt, and these emotions must be acknowledged rather than dismissed. The physician’s capacity to navigate such dialogues without inducing shame or overwhelm strengthens the therapeutic alliance. Emotional presence—acknowledging uncertainty, grief, or anxiety—reinforces trust and promotes openness. Experience, reflection, and deliberate practice cultivate this competence, allowing physicians to approach sensitive discussions with grace and professionalism.
Patient engagement extends far beyond the confines of the consultation room. Encouraging adherence to treatment regimens, lifestyle modifications, and preventive measures demands ongoing dialogue, support, and reinforcement. Physicians act as both guides and collaborators, shaping behaviors through education, motivation, and feedback. The integration of digital tools, reminders, and community resources can augment engagement, provided they respect individual preferences and circumstances. Sustained patient participation hinges on relational continuity, personalized care, and consistent reinforcement of health-promoting behaviors.
Cultural competence underpins all aspects of communication and engagement. Patients’ perceptions of illness, treatment expectations, and decision-making processes are profoundly shaped by cultural beliefs, social norms, and familial dynamics. A physician attuned to these influences can tailor interventions, anticipate challenges, and reduce barriers to effective care. Cultural sensitivity enriches routine consultations, transforming them into holistic encounters that honor both scientific rigor and the patient’s lived experience. It allows the practitioner to navigate complexities that transcend the biomedical model, recognizing the intersection of health, identity, and context.
Reflective practice consolidates these communication skills. Regularly reviewing consultations, seeking feedback from colleagues, and identifying missed opportunities fosters continual growth. Mastery emerges not solely from innate talent but from deliberate observation, adaptive learning, and mindful engagement. Physicians who embrace reflective practice refine their capacity to connect, understand, and influence patients meaningfully. This ongoing process ensures that communication remains a dynamic, evolving skill rather than a static competence.
The Dynamics of Empathetic Listening
Empathetic listening forms the foundation of effective patient interaction. It requires more than simply hearing words; it involves attending to tone, rhythm, and the unspoken emotions embedded within language. Each patient brings a unique constellation of experiences, fears, and expectations, and the ability to perceive these subtleties differentiates superficial consultations from transformative ones. Empathetic listening fosters trust, encourages disclosure, and enables physicians to discern the underlying drivers of illness, whether psychological, social, or physiological. This depth of understanding guides accurate diagnosis and tailored interventions, enhancing the therapeutic impact.
Active listening encompasses several dimensions. It requires intentional presence, allowing the patient to speak without interruption while signaling comprehension through verbal and non-verbal cues. Reflective feedback, gentle summarization, and thoughtful questioning confirm understanding and encourage patients to elaborate. Silence, when employed judiciously, can be a powerful tool, granting space for reflection and disclosure. The mastery of this subtle interplay demands patience, emotional intelligence, and a willingness to embrace uncertainty inherent in human narratives. Over time, physicians cultivate an intuitive sensitivity to when and how to probe, support, or simply bear witness to their patients’ stories.
Empathetic listening also influences patient adherence. When patients feel truly understood, they are more likely to embrace therapeutic recommendations and sustain behavioral change. Conversely, inattentive or mechanical interactions can breed frustration, distrust, or disengagement. Physicians who prioritize listening create an environment where patients are empowered to take an active role in their care. The resulting partnership nurtures resilience, fosters collaboration, and enhances both satisfaction and health outcomes. Listening becomes not merely a skill but a form of relational artistry, shaping the experience and trajectory of care.
Translating Medical Knowledge into Understanding
The capacity to convey medical knowledge clearly and meaningfully is as vital as the acquisition of that knowledge itself. Medical jargon, while precise, can obscure understanding and intimidate patients. Physicians must translate complex concepts into narratives that resonate with the patient’s cognitive and emotional framework. Metaphors, analogies, and visual representations transform abstract ideas into tangible understanding. Stepwise explanations, tailored to individual literacy levels, demystify conditions and interventions, promoting adherence and informed decision-making.
This process requires sensitivity to cognitive and emotional states. Patients may approach consultations with fear, anxiety, or preconceived notions. Recognizing and addressing these emotions allows physicians to adjust explanations, pacing, and tone. The objective is not merely to impart information but to cultivate comprehension, trust, and confidence. Effective communication, therefore, blends scientific precision with psychological insight, transforming knowledge transfer into a collaborative endeavor. In doing so, physicians foster agency, enabling patients to navigate their health journey with clarity and purpose.
Clear communication also mitigates the risk of misinformation. In a landscape where health information is abundant yet variable in quality, the physician’s voice provides a reliable anchor. Accurate, accessible explanations counter confusion, reduce anxiety, and encourage adherence. Patients who understand the rationale behind recommendations are more likely to integrate them into daily life, whether through medication compliance, lifestyle adjustments, or preventive behaviors. This alignment between understanding and action exemplifies the tangible benefits of skilled communication.
Navigating Sensitive and Complex Topics
Discussions surrounding sensitive health matters challenge physicians to balance honesty, empathy, and discretion. Conversations about mental health, chronic disease, or end-of-life care demand emotional presence and strategic communication. Patients may struggle with stigma, fear, or denial, requiring the physician to modulate approach with compassion and clarity. A delicate equilibrium must be maintained, conveying necessary information while avoiding overwhelm or disengagement. This nuanced dialogue fosters trust, reduces anxiety, and reinforces the therapeutic alliance.
Physicians often encounter emotional expression in various forms: tears, silence, anger, or defensiveness. Responding appropriately requires both attunement and restraint, validating emotions without allowing them to derail the consultation. Empathetic acknowledgment—such as recognizing grief, frustration, or anxiety—demonstrates presence and enhances rapport. These skills are cultivated through experience, reflection, and a conscious effort to engage with discomfort constructively. Mastery in navigating sensitive topics transforms potentially stressful encounters into opportunities for connection, understanding, and patient empowerment.
The physician’s approach to complexity extends beyond emotion to incorporate ethical considerations. Decisions about treatment options, prognosis, or intervention timing may intersect with values, beliefs, or personal priorities. Sensitivity to these dimensions enables shared decision-making, where patients feel respected and heard. Communication in these contexts becomes both art and science, requiring clarity, compassion, and ethical discernment. The resulting engagement strengthens adherence, reduces conflict, and supports holistic care.
Sustaining Engagement Beyond the Consultation
Patient engagement is an ongoing process, extending far beyond the immediate consultation. Physicians play a crucial role in guiding behavior, reinforcing adherence, and supporting lifestyle modifications. Engagement involves regular dialogue, feedback, and encouragement, helping patients navigate challenges and maintain commitment to therapeutic goals. Trust established during initial consultations becomes the foundation for sustained interaction, fostering resilience and accountability.
Digital tools, reminders, and community resources can support engagement when integrated thoughtfully. Mobile applications, monitoring devices, or online educational content extend the physician’s influence, providing timely reinforcement and information. However, the human element remains paramount; technology complements rather than replaces relational connection. Personalized guidance, empathy, and active support ensure that interventions are meaningful, practical, and sustainable. In this way, engagement becomes an iterative process, shaped by interaction, adaptation, and collaboration.
The physician’s role also encompasses motivational support. Encouraging patients to adopt preventive measures, adhere to lifestyle changes, or manage chronic conditions requires a balance of accountability and reinforcement. Recognition of progress, acknowledgment of challenges, and adaptive strategies create a supportive environment that nurtures persistence. By fostering a sense of partnership, physicians transform engagement into a shared responsibility, where patients are active participants rather than passive recipients of care.
Cultural Sensitivity as a Core Competence
Cultural sensitivity underpins effective communication and engagement. Health beliefs, social norms, and family dynamics profoundly influence patient perceptions, decisions, and behaviors. Physicians attuned to these factors can tailor interventions, anticipate challenges, and reduce barriers to adherence. Recognizing cultural diversity enriches the consultation process, transforming standard protocols into meaningful, individualized care.
Cultural competence requires more than superficial acknowledgment; it demands deep understanding and respect. Physicians must consider language preferences, belief systems, and social context when framing explanations, offering recommendations, and engaging patients in shared decision-making. This awareness reduces miscommunication, enhances trust, and promotes equitable care. It also allows physicians to navigate potential conflicts between medical advice and cultural expectations, finding solutions that honor both clinical evidence and patient identity.
Integrating cultural sensitivity into practice strengthens patient engagement by affirming dignity, respect, and relevance. Patients are more likely to embrace recommendations when they feel understood and respected within their cultural framework. This alignment fosters adherence, reduces anxiety, and enhances the overall quality of care. Cultural competence, therefore, is not ancillary but central to effective communication and meaningful patient engagement.
Reflection and Continuous Improvement
Reflective practice consolidates the skills and insights gained through patient interactions. Physicians who review consultations, seek feedback, and analyze outcomes cultivate a deeper understanding of their communication strengths and areas for growth. Reflection encourages self-awareness, adaptability, and continuous learning, ensuring that patient engagement evolves in response to changing needs and contexts.
The process of reflection involves identifying missed opportunities, evaluating responses, and considering alternative approaches. This deliberate examination transforms experience into wisdom, enhancing future interactions. Feedback from colleagues, mentors, or patients provides additional perspective, fostering a culture of learning and improvement. By embracing reflection, physicians refine their capacity to listen, explain, empathize, and guide, ensuring that communication remains effective, compassionate, and impactful.
Reflective practice also supports emotional resilience. Engaging deeply with patient narratives, emotions, and challenges can be taxing. Reflection allows physicians to process experiences, maintain professional equilibrium, and sustain motivation. It transforms the art of communication into a consciously cultivated skill, where insight, empathy, and adaptability converge. In doing so, physicians ensure that their practice not only addresses medical needs but also enriches the patient experience through intentional, thoughtful engagement.
The Essence of Preventive Medicine in General Practice
Preventive medicine occupies a central role in general practice, transforming the clinical encounter from reactive treatment to proactive health stewardship. In this framework, physicians are not merely responders to illness but architects of wellness, anticipating potential health challenges and guiding patients toward resilience. The practice necessitates a deep understanding of biological predispositions, environmental exposures, and lifestyle influences that converge to shape an individual’s trajectory. By integrating these factors, the general practitioner becomes a sentinel, discerning subtle signals that precede disease and intervening before pathology manifests.
Preventive medicine also relies on keen observation and methodical assessment. The GP’s office is a microcosm of the population, with each patient reflecting broader epidemiological patterns. Understanding these patterns requires continuous engagement with data, both clinical and societal. Risk stratification becomes essential, allowing clinicians to identify those most susceptible to illness, while tailoring interventions to personal circumstances. The interplay between individual and community health underscores the unique position of general practice, where the art of medicine merges seamlessly with public health science.
Strategic Screening and Early Detection
Screening remains a pillar of preventive strategy, enabling the identification of conditions before they progress to significant morbidity. The value of screening lies not merely in detection but in the precise targeting of individuals whose risk profiles warrant intervention. General practitioners must balance the potential benefits with ethical considerations, avoiding unnecessary testing and the psychological burden of overdiagnosis. Effective screening incorporates variables such as age, family history, comorbidities, and lifestyle, thereby personalizing preventive care.
Systematic screening programs, when judiciously applied, have the potential to reshape population health. Early detection of conditions such as hypertension, diabetes, and certain cancers allows for timely management and improved outcomes. Beyond physical measurements, screening encompasses behavioral and psychological assessments, recognizing that mental and social health significantly influence physical well-being. The GP who integrates these elements into routine practice ensures a comprehensive approach, fostering early intervention and sustained wellness.
Vaccination as a Cornerstone of Community Health
Immunization represents one of the most potent tools in preventive medicine, protecting both individuals and communities from infectious disease. Vaccination programs have dramatically reduced the prevalence of once-common illnesses, yet their effectiveness relies on more than mere availability. Patient education, communication, and trust are essential components of successful immunization campaigns. General practitioners who address misconceptions, explain the rationale for vaccines, and manage potential side effects foster adherence and reinforce the therapeutic alliance.
In addition, vaccination discussions illustrate the delicate interplay between scientific expertise and interpersonal skill. The GP must convey complex immunological concepts in accessible language while navigating cultural beliefs and apprehensions. This interaction exemplifies the broader challenge of preventive medicine: translating evidence-based recommendations into practical, patient-centered care. In doing so, general practitioners not only protect individuals but also enhance the resilience of the wider population, contributing to herd immunity and community stability.
Lifestyle Interventions and Behavioral Transformation
The domain of preventive medicine extends far beyond clinical procedures, encompassing lifestyle modification as a fundamental pillar of health. Nutrition, physical activity, stress management, and avoidance of harmful substances constitute the foundational behaviors that influence long-term outcomes. General practitioners serve as guides in this terrain, helping patients establish realistic goals, sustain motivation, and navigate barriers to change.
Behavioral transformation is rarely linear. Relapse, ambivalence, and external challenges are common, requiring patience, empathy, and continual reinforcement. The GP who cultivates a collaborative relationship with patients enhances adherence and empowers individuals to take ownership of their health. Techniques such as motivational interviewing, incremental goal setting, and consistent feedback can transform tentative intentions into durable habits. By addressing lifestyle factors, preventive medicine reduces the burden of chronic disease while enriching quality of life, illustrating the profound impact of sustained behavior change.
Chronic Disease Prevention and Societal Determinants
Chronic conditions such as obesity, hypertension, and diabetes are not merely biological phenomena; they are deeply intertwined with social determinants of health. Access to nutritious food, safe spaces for physical activity, education, income, and cultural norms all shape the risk landscape. Effective preventive care requires that the GP recognize these broader influences and advocate for systemic solutions while delivering individualized guidance.
Interventions at the population level, when harmonized with personal counseling, create environments conducive to health. Community programs promoting physical activity, policies addressing food security, and initiatives supporting mental well-being complement the GP’s office-based efforts. By bridging individual and societal interventions, preventive medicine amplifies its efficacy, ensuring that health gains are sustainable and equitable. This dual approach underscores the holistic nature of general practice, wherein personal care is inseparable from community health advocacy.
Integrating Mental Health into Preventive Strategies
Mental well-being is an integral component of preventive medicine, influencing both physical health and overall resilience. Conditions such as chronic stress, anxiety, and depression can precipitate or exacerbate physical illnesses, from cardiovascular disease to metabolic disorders. Early identification and intervention are therefore critical, and general practitioners are uniquely positioned to incorporate mental health strategies into routine care.
Preventive mental health encompasses a spectrum of approaches, including counseling, stress reduction techniques, mindfulness, and appropriate referrals. The GP’s role involves both detection and guidance, offering supportive frameworks that reduce risk and foster coping mechanisms. Recognizing the intricate interplay between psychological and physiological health reinforces the holistic philosophy of general practice. Patients benefit not only from the management of symptoms but from strategies that cultivate enduring mental and emotional resilience, enhancing their capacity for health maintenance over a lifetime.
Monitoring Population Health Trends in Practice
A final dimension of preventive medicine lies in continuous surveillance and adaptation. Epidemiological trends, emerging infections, and public health initiatives provide critical insights that shape individual and collective care strategies. Staying abreast of such developments allows the general practitioner to anticipate risks, adjust screening protocols, and educate patients proactively.
The integration of population-level data into everyday clinical practice exemplifies the dynamic nature of preventive medicine. Evidence-based strategies must be continually refined to reflect shifting patterns, new discoveries, and societal changes. The GP’s ability to synthesize this information ensures that interventions remain timely, relevant, and effective. By combining vigilance, knowledge, and patient-centered engagement, preventive medicine becomes a living practice—responsive to both the individual and the broader community it serves.
Advancing Preventive Care Through Patient Engagement
Patient engagement is not a passive endeavor; it is an active collaboration that lies at the heart of preventive medicine. Encouraging individuals to participate in their own care fosters accountability, enhances adherence, and strengthens the therapeutic alliance. Engagement strategies range from personalized counseling to the use of health technology for monitoring and feedback, creating a participatory environment in which patients feel empowered rather than dictated to.
Sustained engagement relies on trust, empathy, and clear communication. The GP who invests in understanding a patient’s values, beliefs, and motivations can tailor preventive strategies that resonate meaningfully. This approach acknowledges the human dimension of health, recognizing that behavior change is influenced by psychological, social, and cultural factors. Through deliberate engagement, preventive medicine transcends the mere avoidance of illness, cultivating proactive, informed, and resilient individuals who contribute to the well-being of their communities.
The Interplay of Evidence and Intuition in Prevention
Preventive medicine thrives at the intersection of empirical evidence and clinical intuition. While guidelines, statistical models, and research provide a foundation for action, the GP’s judgment is indispensable in interpreting and applying this knowledge. Every patient encounter offers subtle cues—variations in energy, mood, lifestyle patterns—that guide the practitioner’s recommendations and interventions.
This interplay underscores the artistry inherent in general practice. Evidence informs, but intuition personalizes. By integrating data with nuanced understanding, the GP can craft preventive strategies that are not only scientifically sound but also contextually appropriate. Patients experience care that is tailored, empathetic, and attuned to their unique circumstances, fostering engagement and long-term adherence. Preventive medicine, in this light, becomes both a science and a humanistic endeavor, blending objective rigor with compassionate insight.
The Pillars of Expertise in General Practice
General practice is an intricate art, intertwining scientific precision with humanistic understanding. It is a realm where the practitioner balances empirical knowledge with emotional insight, treating not just disease but the person as a whole. Achieving expertise in this field demands dedication to continuous improvement and an unwavering commitment to the patient’s welfare. Unlike specialty practice, which often focuses narrowly on a body system or procedure, general practice requires a panoramic vision, encompassing prevention, diagnosis, management, and the social contexts that influence health.
Each patient encounter becomes a microcosm of broader human experience, offering opportunities for learning and growth. The physician’s judgment is tested not only by the complexity of symptoms but also by the nuances of individual values, family dynamics, and cultural beliefs. Expertise emerges not merely from technical proficiency but from an ability to synthesize these dimensions into coherent, empathetic care. A seasoned general practitioner becomes adept at discerning subtle patterns, anticipating complications, and providing guidance that balances hope with realism.
Clinical acumen alone, however, is insufficient. Effective practice demands adaptability, humility, and reflective insight. The landscape of medicine is ever-evolving, shaped by new research, technological advances, and shifting social expectations. A practitioner committed to excellence does not simply accumulate knowledge but continually reassesses assumptions, refines processes, and integrates emerging evidence into practice. This intellectual vigilance ensures that care remains current, relevant, and aligned with the highest ethical standards.
Ethical Foundations and Moral Integrity
Ethical practice forms the backbone of professional life in general practice. Each clinical decision, from prescribing medication to discussing end-of-life care, is embedded in a framework of moral responsibility. The principles of autonomy, beneficence, nonmaleficence, and justice guide interactions, ensuring that patient welfare remains paramount. Respecting autonomy means acknowledging each patient’s right to make informed choices, even when those decisions diverge from the clinician’s recommendations. This respect for personal agency is balanced with the duty to provide clear, comprehensible information and compassionate guidance.
Confidentiality is another cornerstone, requiring vigilance and discretion. Patients entrust sensitive information to their physicians with the expectation of privacy. Breaching this trust, whether through negligence or casual disclosure, erodes the therapeutic relationship and undermines professional credibility. Equally, conflicts of interest must be navigated with transparency and integrity, prioritizing patient welfare over financial or personal gain.
Ethical dilemmas are frequent and multifaceted. Decisions about allocating limited resources, managing chronic or terminal illness, and communicating prognostic uncertainty demand both analytical and emotional intelligence. These challenges underscore the need for a well-calibrated moral compass, reinforced through professional codes, reflective practice, and mentorship. Ethical mastery is not a static state but a dynamic process, shaped by experience, dialogue, and conscious deliberation.
Reflective Practice as a Tool for Growth
Reflective practice transforms routine experience into a reservoir of enduring wisdom. Through deliberate reflection, the general practitioner examines clinical decisions, acknowledges missteps, and identifies opportunities for improvement. This process nurtures humility, resilience, and adaptive problem-solving, enabling growth that extends beyond technical skill. Reflective practice is not mere introspection; it involves structured analysis, often enriched through discussion with peers, mentors, and professional networks.
Case-based reflection is particularly powerful. Revisiting complex cases allows practitioners to dissect diagnostic reasoning, evaluate treatment choices, and assess interpersonal communication. Peer feedback adds objectivity, uncovering blind spots that might otherwise persist unnoticed. Mentorship provides guidance and perspective, linking individual experience with broader professional norms. Over time, these practices cultivate a habit of critical self-assessment, fostering continuous refinement of both clinical judgment and relational aptitude.
Reflective practice also fortifies resilience. Medicine can be emotionally taxing, with encounters that test patience, empathy, and emotional equilibrium. By processing these experiences thoughtfully, practitioners develop strategies to manage stress, maintain well-being, and sustain professional engagement. Reflection thus functions as both a cognitive and emotional tool, enhancing competence while safeguarding the physician’s inner equilibrium.
Lifelong Learning and Intellectual Curiosity
Lifelong learning is indispensable for mastery in general practice. The pace of medical advancement, from emerging therapies to evolving guidelines, requires persistent curiosity and commitment. Learning is not confined to formal education; it spans journal reading, online courses, conference attendance, and experiential exposure. The discerning practitioner synthesizes these diverse inputs, critically appraising relevance and applicability to practice.
Experiential learning is particularly significant. Direct patient care provides insights that textbooks cannot fully convey. Through hands-on management of conditions, practitioners refine diagnostic acumen, procedural dexterity, and communication skills. Combining this practical wisdom with contemporary evidence fosters informed, patient-centered care. The general practitioner thus occupies a dual role as both lifelong student and educator, modeling intellectual rigor and curiosity for colleagues, trainees, and patients alike.
Engagement with the wider scientific community further enhances growth. Participation in professional societies, collaborative research, and academic discourse exposes the practitioner to novel perspectives, emerging challenges, and innovative solutions. This engagement nurtures adaptability, equipping the physician to respond effectively to evolving patterns of disease, healthcare policy shifts, and societal expectations. Lifelong learning is, therefore, both a professional imperative and a moral commitment to excellence.
Time Management and Personal Resilience
The demands of general practice are relentless, encompassing administrative duties, patient care, and ongoing learning. Effective time management is essential to sustain high-quality care without compromising personal well-being. Prioritization, task delegation, and boundary-setting are practical strategies that preserve energy and focus. Equally important is the cultivation of personal resilience, allowing the practitioner to navigate the stresses inherent in medical practice.
Emotional intelligence underpins resilience. The ability to recognize, regulate, and respond to one’s own emotions, as well as to empathize with patients and colleagues, mitigates burnout and enhances interpersonal effectiveness. Mindfulness, reflective journaling, and structured rest periods contribute to mental fortitude, supporting sustained engagement and satisfaction. Resilient practitioners are not invulnerable; they simply cultivate strategies to adapt, recover, and maintain professional and personal equilibrium amidst challenges.
Resilience also extends to adaptability in clinical scenarios. Medicine is unpredictable, with patients presenting complex, multifaceted problems. A practitioner’s ability to remain composed, flexible, and solution-oriented under pressure directly influences outcomes and patient trust. Over time, resilience transforms from reactive coping into proactive mastery, shaping a practice characterized by both competence and compassion.
Interprofessional Collaboration and Coordinated Care
No general practitioner operates in isolation. Optimal care is achieved through collaboration with a network of specialists, nurses, therapists, and community resources. Interprofessional teamwork enhances comprehensiveness, safety, and efficiency, ensuring that patients receive coordinated, holistic care. Effective collaboration relies on mutual respect, clear communication, and shared objectives. It requires balancing professional autonomy with cooperative engagement, integrating diverse expertise to optimize patient outcomes.
The GP serves as a nexus, orchestrating care across disciplines and settings. This role demands not only clinical knowledge but also negotiation, leadership, and diplomacy. By fostering collaborative relationships, the practitioner amplifies the impact of individual interventions, translating multidisciplinary input into cohesive management plans. Team-based care also offers opportunities for reciprocal learning, exposing practitioners to alternative approaches, emerging insights, and novel strategies. Collaboration, therefore, strengthens both patient care and professional development.
Moreover, interprofessional collaboration extends beyond clinical logistics. It encompasses shared ethical deliberation, collective problem-solving, and mutual support. In complex cases, the combined judgment of a diverse team reduces error, enhances innovation, and reinforces accountability. By embracing collaboration as an integral aspect of practice, the general practitioner magnifies both efficacy and impact, ensuring that care transcends the limitations of any single professional perspective.
Integrating Knowledge, Skill, and Humanity
Mastery in general practice is a dynamic interplay of technical skill, ethical integrity, relational acumen, and intellectual curiosity. It requires proficiency in diagnosis and management, but also the capacity to listen deeply, empathize sincerely, and communicate effectively. It is shaped by reflective practice, informed by ongoing learning, and sustained by resilience and self-care. Mastery is neither static nor easily defined; it is a continuum of growth, adaptation, and refinement, evolving with each patient encounter and professional challenge.
The GP’s role is both scientific and humanistic. Each decision, intervention, and conversation carries ethical, emotional, and practical weight. The practitioner must integrate knowledge with judgment, compassion with pragmatism, and expertise with humility. This synthesis is cultivated over years of attentive practice, reinforced by reflection, dialogue, and continuous learning. Mastery is manifested not solely in procedural excellence but in the capacity to inspire trust, alleviate suffering, and guide patients through the uncertainties of life and health.
Enduring excellence in general practice emerges when skill, empathy, ethics, and curiosity converge. The practitioner navigates ambiguity with confidence, communicates with clarity and compassion, and applies knowledge judiciously. Patients benefit not only from accurate diagnosis and effective treatment but also from a professional presence that conveys reassurance, respect, and reliability. The general practitioner’s impact, therefore, extends beyond individual encounters, shaping the health, confidence, and well-being of the broader community.
Conclusion
Mastering medicine in general practice is a journey rather than a destination. It weaves together clinical knowledge, diagnostic acumen, therapeutic skill, patient communication, preventive strategies, and professional growth into a cohesive and dynamic practice. Each patient encounter offers an opportunity to refine judgment, strengthen empathy, and expand understanding, highlighting that expertise is not solely measured by technical skill, but by the ability to navigate complexity with precision and compassion.
The role of the GP extends beyond treating disease; it encompasses anticipating risk, promoting wellness, and fostering resilience in both patients and practitioners. Diagnostic reasoning, when combined with attentive listening and careful observation, transforms uncertainty into actionable insight. Treatment is most effective when it balances evidence-based strategies with individualized care, acknowledging the interplay of lifestyle, psychosocial factors, and patient preferences. Preventive medicine and public health perspectives amplify impact, ensuring that care benefits not only individuals but the communities they inhabit.
Equally important is the cultivation of professional integrity and reflective practice. Ethical decision-making, continuous learning, and interprofessional collaboration create a foundation for sustained excellence. Resilience, emotional intelligence, and adaptability allow the GP to navigate the inevitable challenges and ambiguities of practice without compromising quality of care or personal well-being.
Ultimately, mastery in general practice is defined by the ability to integrate science and humanity, knowledge and intuition, skill and empathy. It is a lifelong pursuit, shaped by curiosity, reflection, and dedication to the welfare of others. Those who embrace this journey not only elevate their own professional competence but profoundly enhance the lives of the patients and communities they serve. The essence of general practice lies in this balance—where clinical expertise meets compassionate care, and where the art and science of medicine converge into a practice that is both skilled and deeply human.
Frequently Asked Questions
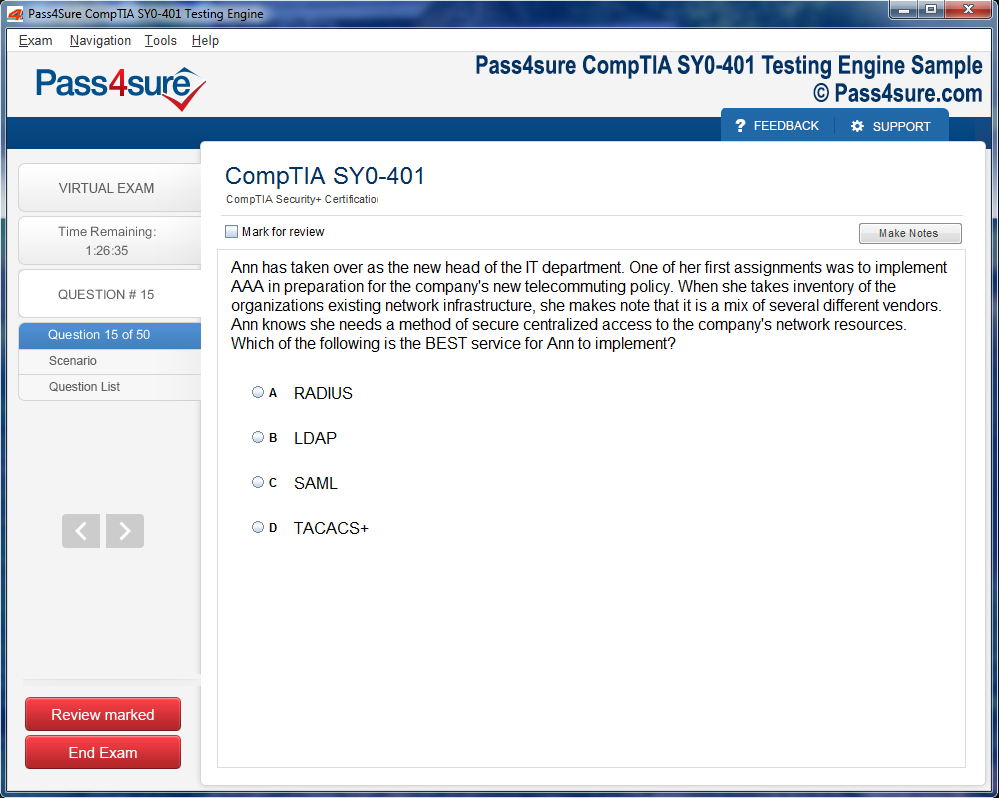
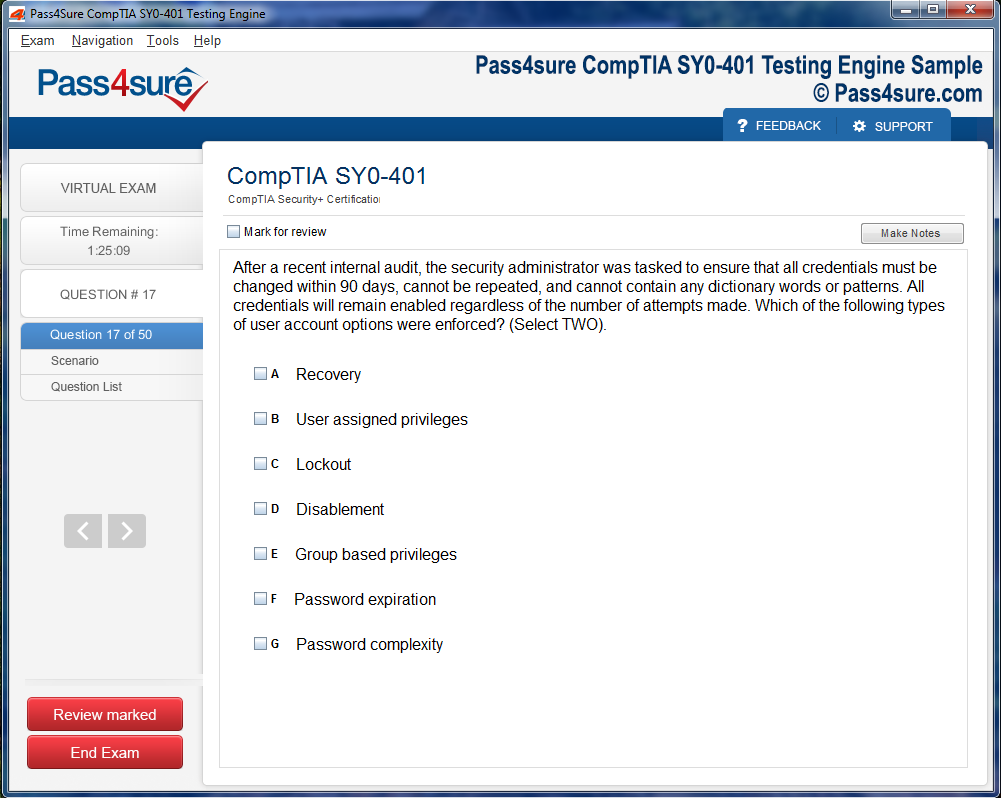
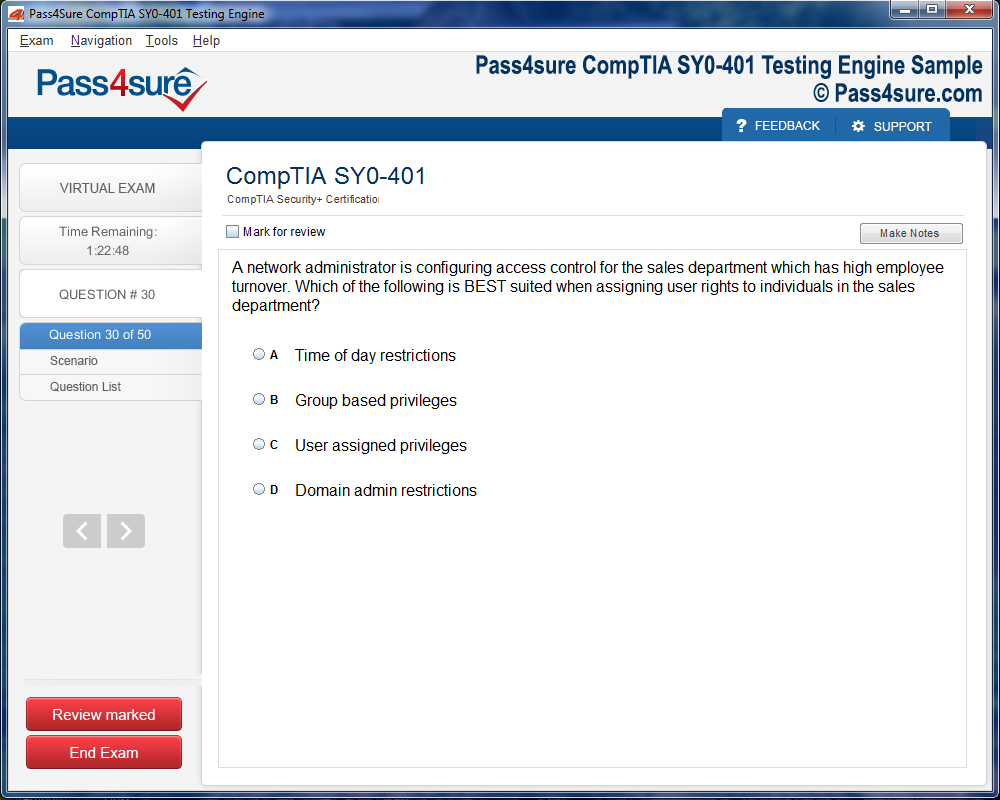
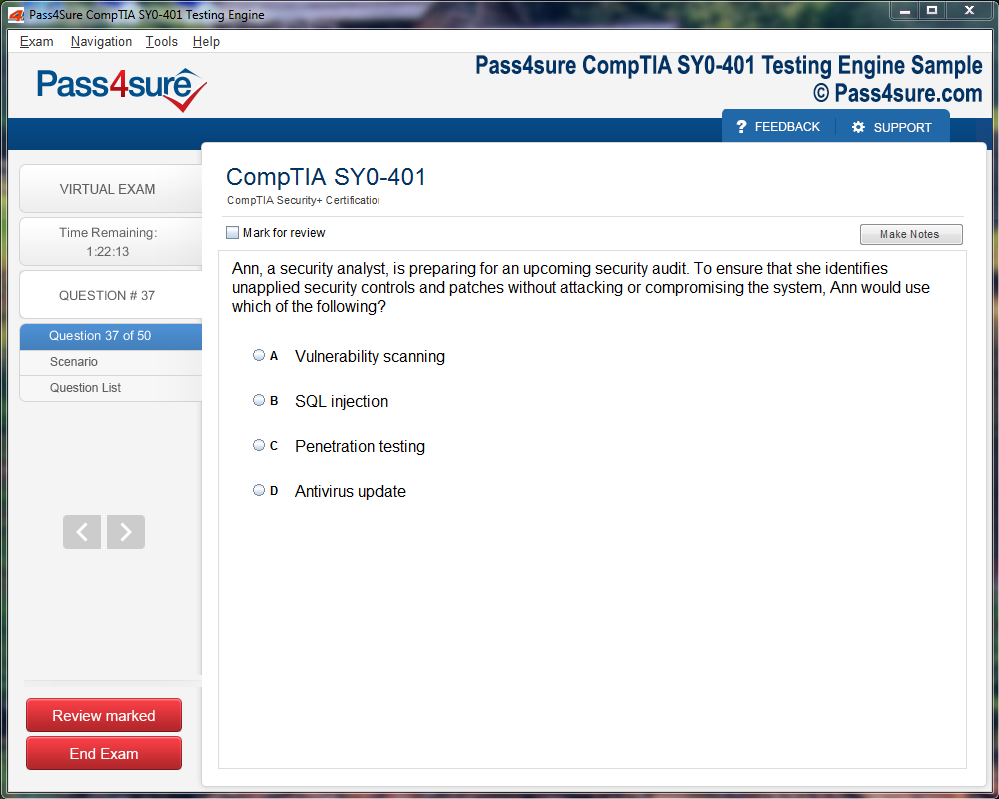
How does your testing engine works?
Once download and installed on your PC, you can practise test questions, review your questions & answers using two different options 'practice exam' and 'virtual exam'. Virtual Exam - test yourself with exam questions with a time limit, as if you are taking exams in the Prometric or VUE testing centre. Practice exam - review exam questions one by one, see correct answers and explanations).
How can I get the products after purchase?
All products are available for download immediately from your Member's Area. Once you have made the payment, you will be transferred to Member's Area where you can login and download the products you have purchased to your computer.
How long can I use my product? Will it be valid forever?
Pass4sure products have a validity of 90 days from the date of purchase. This means that any updates to the products, including but not limited to new questions, or updates and changes by our editing team, will be automatically downloaded on to computer to make sure that you get latest exam prep materials during those 90 days.
Can I renew my product if when it's expired?
Yes, when the 90 days of your product validity are over, you have the option of renewing your expired products with a 30% discount. This can be done in your Member's Area.
Please note that you will not be able to use the product after it has expired if you don't renew it.
How often are the questions updated?
We always try to provide the latest pool of questions, Updates in the questions depend on the changes in actual pool of questions by different vendors. As soon as we know about the change in the exam question pool we try our best to update the products as fast as possible.
How many computers I can download Pass4sure software on?
You can download the Pass4sure products on the maximum number of 2 (two) computers or devices. If you need to use the software on more than two machines, you can purchase this option separately. Please email sales@pass4sure.com if you need to use more than 5 (five) computers.
What are the system requirements?
Minimum System Requirements:
- Windows XP or newer operating system
- Java Version 8 or newer
- 1+ GHz processor
- 1 GB Ram
- 50 MB available hard disk typically (products may vary)
What operating systems are supported by your Testing Engine software?
Our testing engine is supported by Windows. Andriod and IOS software is currently under development.